-
PDF
- Split View
-
Views
-
Cite
Cite
Mirela Habibović, Krista C. van den Broek, Dominic A.M.J. Theuns, Luc Jordaens, Marco Alings, Pepijn H. van der Voort, Susanne S. Pedersen, Gender disparities in anxiety and quality of life in patients with an implantable cardioverter–defibrillator, EP Europace, Volume 13, Issue 12, December 2011, Pages 1723–1730, https://doi.org/10.1093/europace/eur252
Close - Share Icon Share
Abstract
A paucity of studies in implantable cardioverter–defibrillator (ICD) patients has examined gender disparities in patient-reported outcomes, such as anxiety and quality of life (QoL). We investigated (i) gender disparities in anxiety and QoL and (ii) the magnitude of the effect of gender vs. New York Heart Association (NYHA) functional class (III/IV), ICD shock, and Type D personality on these outcomes.
Implantable cardioverter–defibrillator patients (n = 718; 81% men) completed the State-Trait Anxiety Inventory (STAI) and the Short-Form Health Survey 36 (SF-36) at baseline and 12 months post-implantation. The magnitude of the effect was indicated using Cohen's effect size index. Multivariate analysis of covariance for repeated measures showed no differences between men and women on mean scores of anxiety (F(1,696) = 2.67, P= 0.10). Differences in QoL were observed for only two of the eight subscales of the SF-36, with women reporting poorer physical functioning (F(1,696) = 7.14, P= 0.008) and vitality (F(1,696) = 4.88, P= 0.028) than men. With respect to anxiety, effect sizes at baseline and 12 months for gender, NYHA class, and ICD shocks were small. A large effect size for Type D personality was found at both time points. For QoL, at baseline and 12 months, the effect sizes for gender were small, while the influence of NYHA class and Type D personality was moderate to large.
Men and women did not differ on mean anxiety or QoL scores, except for women reporting poorer QoL on two domains. The relative influence of gender on anxiety and QoL was less than that of NYHA functional class and Type D personality.
Introduction
Implantable cardioverter–defibrillator (ICD) therapy is the mainstay of treatment for primary and secondary prevention of sudden cardiac death.1 Implantable cardioverter–defibrillator treatment is generally well accepted by most patients, but a significant subgroup (i.e. 24–33% of ICD patients) experiences psychological difficulties, with the most profound manifestations being anxiety and depression,2,3 post-traumatic stress disorder,4,5 and poor quality of life (QoL). 3,6 In turn, these patient-reported outcomes have been associated with risk of ventricular tachyarrhythmia's7–9 and mortality10,11 in ICD patients. Hence, it is important to be able to identify patients who are at risk of adverse psychological outcomes and to provide extra support if needed.
Implantable cardioverter–defibrillator shock is generally considered the primary culprit in the event of the development of psychological distress and deterioration in QoL.12,13 Although ICD shock may have a profound influence on individual patients, the evidence for an influence of shock on psychological outcomes and QoL is inconsistent and likely to be more complex than generally assumed.14,15 The evidence for an influence of ICD indication and device advisories is also mixed, with some but not all studies finding an effect on psychological outcomes and poor QoL.16–20 Younger age,21 symptomatic heart failure,22 lack of optimism,23 diabetes,24 and Type D personality25 (patients who experience a range of negative emotions, but inhibit the expression of these emotions) constitute other factors that have been associated with risk of poorer psychological and QoL outcomes.
Gender has also been proposed as a potentially important risk factor for psychological distress and poor QoL.6,26 Gender disparities may be attributed to differences in the way of dealing with stressful situations,27 in the acceptance of mechanical devices28 and pain sensitivity.29 Based on these findings, it would make sense to expect that women experience more psychological distress after ICD implantation than men. However, recent studies on gender differences in anxiety and QoL have shown mixed findings, with some of the studies indicating that women are more prone to experiencing anxiety than men,3,30 while other studies found no gender differences in anxiety.31–33 Studies on QoL also show inconsistent findings, with some30,34 but not all studies supporting the presence of gender differences in QoL.31,35–37 These mixed findings are corroborated in a recent viewpoint focusing on gender disparities in patient-reported outcomes, such as anxiety, depression, and QoL,38 and may in part be explained by heterogeneity in study designs but also by the use of smaller scale ad hoc studies that were not designed a priori to examine gender differences on these outcomes, with the risk that some studies were not sufficiently powered to find an effect if present.
Hence, in a large multi-centre study of ICD patients with a 12-month follow-up, we examined (i) potential gender disparities in anxiety and QoL and (ii) the magnitude of the effect of gender vs. NYHA functional class III/IV (as an indicator of disease severity), ICD shock, and Type D personality as determinants of anxiety and QoL, using Cohen's effect size index.39 We expected that women and men would adapt equally well to the ICD and that the effect of gender on anxiety and QoL would be less compared with the effect of NYHA class, ICD shock, and Type D personality.
Methods
Patient sample and procedure
Patients from three Dutch hospitals (Amphia Hospital, Breda; Catharina Hospital, Eindhoven; Erasmus Medical Center, Rotterdam) who were hospitalized between May 2003 and June 2009 for an ICD implantation were included in the study and completed a set of standardized and validated questionnaires. Patients included in the Erasmus Medical Centre were part of the ongoing Mood and personality as precipitants of arrhythmia in patients with an Implantable cardioverter–Defibrillator: A prospective Study (MIDAS). Exclusion criteria were significant cognitive impairments (e.g. dementia), life-threatening comorbidities (e.g. cancer), a history of psychiatric illness other than affective/anxiety disorders, and insufficient knowledge of the Dutch language.
The study was approved by the Medical Ethics Committee of the participating hospitals and conducted in accordance with the Helsinki Declaration. All patients provided written informed consent.
Demographic and clinical variables
Information on demographic and clinical variables were obtained either via purpose-designed questions in the questionnaire or via the patients’ medical records. Demographic variables included age, gender, marital status (single vs. having a partner), education (primary school vs. higher), and working status (working vs. not working). Clinical variables included ICD indication (primary vs. secondary prevention), cardiac resynchronization therapy (CRT), coronary artery disease (CAD), New York Heart Association (NYHA) functional class (NYHA class I/II vs. III/IV), left ventricular ejection fraction (LVEF <35%), QRS width (QRS >120 ms), diabetes, smoking, and cardiac [i.e. angiotensin-converting enzyme (ACE)-inhibitors, amiodarone, beta-blockers, digoxin, diuretics, and statins], and psychotropic medication.
Information on ICD shocks (appropriate and inappropriate) occurring during the 12-month follow-up period was obtained via device interrogation and extracted from the patients’ medical records. To enhance the power, appropriate and inappropriate shocks were combined in one variable.
Measures
Anxiety
The state version of the State-Trait Anxiety Inventory (STAI) was used to assess general symptoms of anxiety, such as worries and concerns, and tension.40 In the current study we only used the State (STAI-S) measure because we wanted to assess the presence of symptoms of anxiety at baseline and not anxiety as a stable trait. The STAI-S is a self-report questionnaire, consisting of two 10-item scales, measuring, respectively, the presence and absence of anxiety symptoms. Items are answered on a 4-point Likert scale ranging from 1 (not at all) to 4 (very much so), with total scores ranging from 20 to 80, with a high score indicating a high level of anxiety. A cut-off score ≥40 indicates probable clinical levels of anxiety.40 The STAI-S has shown to be a valid and reliable measure, with Cronbach's alpha ranging from 0.87 to 0.92.40 The STAI-S was administered at baseline and at 12 months post-implantation.
Quality of life
The Dutch version of the Short-Form Health Survey (SF-36) was administered to assess QoL.41 The SF-36 consists of eight subscales: Physical Functioning (PF; 10 items), Social Functioning (SF; 2 items), Role Limitations due to Physical Functioning (RP; 4 items), Role Limitations due to Emotional Functioning (RE; 3 items), Mental Health (MH; 5 items), Vitality (VT; 4 items), Bodily Pain (BP; 2 items), and General Health (GH; 5 items). Items are answered according to standardized response choices. Raw scores are transformed to scale scores ranging from 0 to 100, with higher scores indicating better levels of functioning.42 For the BP subscale, a higher score denotes the absence of pain. The validity and reliability of the Dutch SF-36 are good, with a mean alpha of 0.84 across groups from the Dutch general population, migraine patients, and cancer patients.41 The SF-36 was administered at baseline and at 12 months post-implantation.
Type D personality
Type D personality was assessed with the 14-item Type D scale (DS14).43 The DS14 consists of two 7-item subscales measuring Negative Affectivity (‘I am often in a bad mood’) and Social Inhibition (‘I often feel inhibited in social interactions’), respectively. Each item is rated on a 5-point Likert scale from 0 (false) to 4 (true), with total scores ranging from 0 to 28 for both subscales. Patients scoring ≥10 on both subscales are classified as Type D, which has shown to be the most optimal cut-off for both subscales for determining caseness.43,44 Both subscales are internally consistent, with a Cronbach's alpha of 0.88 for Negative Affectivity and 0.86 for Social Inhibition, and a test–retest reliability over a 3-month period of r= 0.72 and r= 0.82 for the two subscales, respectively.43 The DS14 is a stable personality measure over an 18-month period in post-myocardial infarction patients.45
Statistical analysis
Discrete variables were compared with the χ2 test and continuous variables with Student's t-test for independent samples. To compare the relative influence of gender with that of NYHA functional class (III/IV), ICD shocks, and Type D personality on anxiety and QoL, the effect size was calculated using Cohen's effect size d.39 According to Cohen's d, an effect size index of 0.20 represents a small effect, 0.50 a moderate effect and ≥0.80 a large effect. Multivariate analysis of variance (MANOVA) for repeated measures was performed to examine the relationship between gender and anxiety and gender and QoL, respectively. To adjust for potential confounders, we used MANCOVA. Two models were tested in the adjusted analysis. In the first model, we adjusted for all covariates except for NYHA functional class, LVEF, and QRS width. These variables all form part of the criteria for CRT indication and were excluded from analysis to avoid the problem of multicollinearity. In the second model, we added NYHA functional class to the set of covariates in the first model to control for symptomatic heart failure. In both models we also adjusted for site of implantation. In secondary analyses, we differentiated between appropriate and inappropriate shocks and whether type of shock had a differential impact on anxiety and QoL. To reduce the chance of Type 1 error (that is, finding a significant result when in fact there is none), we applied a Bonferroni correction to the t-tests. The original alpha value of 0.05 was divided by the number of comparisons that were made (i.e. 0.05/9), which resulted in an alpha of 0.006 to indicate statistical significance. All tests were two-tailed and an alpha of 0.05 was used to indicate statistical significance for the χ2 test. Data were analysed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics
Of 1080 patients who agreed to participate in the study, 82 (7.6%) patients died between baseline and 12 months follow-up, 68 (6.3%) patients refused to participate at 12 months follow-up, 12 (1.1%) were lost to follow-up, and 200 (18.5%) patients had missing data on self-report measures or clinical variables. Hence, statistical analyses are based on 718 (66.5%) patients. Patients who were excluded from analyses did not differ systematically on any of the study variables from the included patients (all P’s >0.05; data not shown).
Patient baseline characteristics for the total sample and stratified by gender are shown in Table 1. Women were more likely to be younger, to have a higher educational level, and to have a more preserved LVEF, but less likely to have a partner, to have CAD, and to be prescribed ACE-inhibitors, amiodarone, and statins compared with men.
Patient baseline characteristics for the total sample and stratified by gendera
| . | Total . | Male . | Female . | P . |
|---|---|---|---|---|
| . | n = 718 . | n = 579 . | n = 139 . | . |
| Demographics | ||||
| Age | 60.81 ± 10.97 | 61.4 ± 10.55 | 58.3 ± 12.29 | 0.003 |
| Partner | 647 (90.1) | 534 (92.2) | 113 (81.3) | <0.001 |
| Smoking | 100 (13.9) | 80 (13.8) | 20 (14.4) | 0.86 |
| Low education | 378 (52.6) | 286 (49.4) | 92 (66.2) | <0.001 |
| Not working status (yes) | 206 (28.7) | 167 (28.8) | 39 (28.1) | 0.85 |
| Center | 0.31 | |||
| Amphia | 186 (25.9) | 146 (25.2) | 40 (28.8) | |
| Catharina | 257 (35.8) | 215 (937.1) | 42 (30.2) | |
| Erasmus | 275 (38.3) | 218 (37.7) | 57 (41.0) | |
| Clinical factors | ||||
| Indication (secondary) | 345 (48.1) | 282 (48.7) | 63 (45.3) | 0.47 |
| CADb | 484 (67.4) | 423 (73.1) | 61 (43.9) | <0.001 |
| NYHA class III/IV1,c | 187 (31.6) | 144 (30.4) | 43 (36.4) | 0.21 |
| LVEF<35%2,d | 558 (83.5) | 459 (85.2) | 99 (76.7) | 0.021 |
| QRS > 1203 | 386 (55.3) | 318 (56.5) | 68 (50.4) | 0.20 |
| CRTe | 176 (24.5) | 133 (23.0) | 43 (30.9) | 0.05 |
| Shocksf | 85 (11.8) | 72 (12.4) | 13 (9.4) | 0.31 |
| Appropriate shocks | 58 (8.1) | 50 (8.7) | 8 (5.8) | 0.27 |
| Inappropriate shocks | 28 (3.9) | 24 (4.2) | 4 (2.9) | 0.50 |
| Diabetes | 115 (16.0) | 98 (16.9) | 17 (12.2) | 0.18 |
| Psychological factors | ||||
| Type D personality | 146 (20.3) | 119 (20.6) | 27 (19.4) | 0.77 |
| Medication | ||||
| Psychotropics | 123 (17.1) | 92 (15.9) | 31 (22.3) | 0.07 |
| ACE-inhibitors | 503 (70.1) | 417 (72.0) | 86 (61.9) | 0.019 |
| Amiodarone | 132 (18.4) | 116 (20.0) | 16 (11.5) | 0.021 |
| Beta-blockers | 584 (81.3) | 471 (81.3) | 113 (81.3) | 0.99 |
| Digoxin | 95 (13.2) | 78 (13.5) | 17 (12.2) | 0.70 |
| Diuretics | 438 (61.0) | 356 (61.5) | 82 (59.0) | 0.59 |
| Statins | 479 (66.7) | 415 (71.7) | 64 (46.0) | <0.001 |
| . | Total . | Male . | Female . | P . |
|---|---|---|---|---|
| . | n = 718 . | n = 579 . | n = 139 . | . |
| Demographics | ||||
| Age | 60.81 ± 10.97 | 61.4 ± 10.55 | 58.3 ± 12.29 | 0.003 |
| Partner | 647 (90.1) | 534 (92.2) | 113 (81.3) | <0.001 |
| Smoking | 100 (13.9) | 80 (13.8) | 20 (14.4) | 0.86 |
| Low education | 378 (52.6) | 286 (49.4) | 92 (66.2) | <0.001 |
| Not working status (yes) | 206 (28.7) | 167 (28.8) | 39 (28.1) | 0.85 |
| Center | 0.31 | |||
| Amphia | 186 (25.9) | 146 (25.2) | 40 (28.8) | |
| Catharina | 257 (35.8) | 215 (937.1) | 42 (30.2) | |
| Erasmus | 275 (38.3) | 218 (37.7) | 57 (41.0) | |
| Clinical factors | ||||
| Indication (secondary) | 345 (48.1) | 282 (48.7) | 63 (45.3) | 0.47 |
| CADb | 484 (67.4) | 423 (73.1) | 61 (43.9) | <0.001 |
| NYHA class III/IV1,c | 187 (31.6) | 144 (30.4) | 43 (36.4) | 0.21 |
| LVEF<35%2,d | 558 (83.5) | 459 (85.2) | 99 (76.7) | 0.021 |
| QRS > 1203 | 386 (55.3) | 318 (56.5) | 68 (50.4) | 0.20 |
| CRTe | 176 (24.5) | 133 (23.0) | 43 (30.9) | 0.05 |
| Shocksf | 85 (11.8) | 72 (12.4) | 13 (9.4) | 0.31 |
| Appropriate shocks | 58 (8.1) | 50 (8.7) | 8 (5.8) | 0.27 |
| Inappropriate shocks | 28 (3.9) | 24 (4.2) | 4 (2.9) | 0.50 |
| Diabetes | 115 (16.0) | 98 (16.9) | 17 (12.2) | 0.18 |
| Psychological factors | ||||
| Type D personality | 146 (20.3) | 119 (20.6) | 27 (19.4) | 0.77 |
| Medication | ||||
| Psychotropics | 123 (17.1) | 92 (15.9) | 31 (22.3) | 0.07 |
| ACE-inhibitors | 503 (70.1) | 417 (72.0) | 86 (61.9) | 0.019 |
| Amiodarone | 132 (18.4) | 116 (20.0) | 16 (11.5) | 0.021 |
| Beta-blockers | 584 (81.3) | 471 (81.3) | 113 (81.3) | 0.99 |
| Digoxin | 95 (13.2) | 78 (13.5) | 17 (12.2) | 0.70 |
| Diuretics | 438 (61.0) | 356 (61.5) | 82 (59.0) | 0.59 |
| Statins | 479 (66.7) | 415 (71.7) | 64 (46.0) | <0.001 |
aResults are presented as numbers (percentages) unless otherwise indicated.
bCoronary artery disease.
cNew York Heart Association functional class.
dLeft ventricular ejection fraction.
eCardiac resynchronization therapy.
fAppropriate and inappropriate shocks received between implantation and 12 months follow-up.
1n = 592
2n = 668
3n = 698
Patient baseline characteristics for the total sample and stratified by gendera
| . | Total . | Male . | Female . | P . |
|---|---|---|---|---|
| . | n = 718 . | n = 579 . | n = 139 . | . |
| Demographics | ||||
| Age | 60.81 ± 10.97 | 61.4 ± 10.55 | 58.3 ± 12.29 | 0.003 |
| Partner | 647 (90.1) | 534 (92.2) | 113 (81.3) | <0.001 |
| Smoking | 100 (13.9) | 80 (13.8) | 20 (14.4) | 0.86 |
| Low education | 378 (52.6) | 286 (49.4) | 92 (66.2) | <0.001 |
| Not working status (yes) | 206 (28.7) | 167 (28.8) | 39 (28.1) | 0.85 |
| Center | 0.31 | |||
| Amphia | 186 (25.9) | 146 (25.2) | 40 (28.8) | |
| Catharina | 257 (35.8) | 215 (937.1) | 42 (30.2) | |
| Erasmus | 275 (38.3) | 218 (37.7) | 57 (41.0) | |
| Clinical factors | ||||
| Indication (secondary) | 345 (48.1) | 282 (48.7) | 63 (45.3) | 0.47 |
| CADb | 484 (67.4) | 423 (73.1) | 61 (43.9) | <0.001 |
| NYHA class III/IV1,c | 187 (31.6) | 144 (30.4) | 43 (36.4) | 0.21 |
| LVEF<35%2,d | 558 (83.5) | 459 (85.2) | 99 (76.7) | 0.021 |
| QRS > 1203 | 386 (55.3) | 318 (56.5) | 68 (50.4) | 0.20 |
| CRTe | 176 (24.5) | 133 (23.0) | 43 (30.9) | 0.05 |
| Shocksf | 85 (11.8) | 72 (12.4) | 13 (9.4) | 0.31 |
| Appropriate shocks | 58 (8.1) | 50 (8.7) | 8 (5.8) | 0.27 |
| Inappropriate shocks | 28 (3.9) | 24 (4.2) | 4 (2.9) | 0.50 |
| Diabetes | 115 (16.0) | 98 (16.9) | 17 (12.2) | 0.18 |
| Psychological factors | ||||
| Type D personality | 146 (20.3) | 119 (20.6) | 27 (19.4) | 0.77 |
| Medication | ||||
| Psychotropics | 123 (17.1) | 92 (15.9) | 31 (22.3) | 0.07 |
| ACE-inhibitors | 503 (70.1) | 417 (72.0) | 86 (61.9) | 0.019 |
| Amiodarone | 132 (18.4) | 116 (20.0) | 16 (11.5) | 0.021 |
| Beta-blockers | 584 (81.3) | 471 (81.3) | 113 (81.3) | 0.99 |
| Digoxin | 95 (13.2) | 78 (13.5) | 17 (12.2) | 0.70 |
| Diuretics | 438 (61.0) | 356 (61.5) | 82 (59.0) | 0.59 |
| Statins | 479 (66.7) | 415 (71.7) | 64 (46.0) | <0.001 |
| . | Total . | Male . | Female . | P . |
|---|---|---|---|---|
| . | n = 718 . | n = 579 . | n = 139 . | . |
| Demographics | ||||
| Age | 60.81 ± 10.97 | 61.4 ± 10.55 | 58.3 ± 12.29 | 0.003 |
| Partner | 647 (90.1) | 534 (92.2) | 113 (81.3) | <0.001 |
| Smoking | 100 (13.9) | 80 (13.8) | 20 (14.4) | 0.86 |
| Low education | 378 (52.6) | 286 (49.4) | 92 (66.2) | <0.001 |
| Not working status (yes) | 206 (28.7) | 167 (28.8) | 39 (28.1) | 0.85 |
| Center | 0.31 | |||
| Amphia | 186 (25.9) | 146 (25.2) | 40 (28.8) | |
| Catharina | 257 (35.8) | 215 (937.1) | 42 (30.2) | |
| Erasmus | 275 (38.3) | 218 (37.7) | 57 (41.0) | |
| Clinical factors | ||||
| Indication (secondary) | 345 (48.1) | 282 (48.7) | 63 (45.3) | 0.47 |
| CADb | 484 (67.4) | 423 (73.1) | 61 (43.9) | <0.001 |
| NYHA class III/IV1,c | 187 (31.6) | 144 (30.4) | 43 (36.4) | 0.21 |
| LVEF<35%2,d | 558 (83.5) | 459 (85.2) | 99 (76.7) | 0.021 |
| QRS > 1203 | 386 (55.3) | 318 (56.5) | 68 (50.4) | 0.20 |
| CRTe | 176 (24.5) | 133 (23.0) | 43 (30.9) | 0.05 |
| Shocksf | 85 (11.8) | 72 (12.4) | 13 (9.4) | 0.31 |
| Appropriate shocks | 58 (8.1) | 50 (8.7) | 8 (5.8) | 0.27 |
| Inappropriate shocks | 28 (3.9) | 24 (4.2) | 4 (2.9) | 0.50 |
| Diabetes | 115 (16.0) | 98 (16.9) | 17 (12.2) | 0.18 |
| Psychological factors | ||||
| Type D personality | 146 (20.3) | 119 (20.6) | 27 (19.4) | 0.77 |
| Medication | ||||
| Psychotropics | 123 (17.1) | 92 (15.9) | 31 (22.3) | 0.07 |
| ACE-inhibitors | 503 (70.1) | 417 (72.0) | 86 (61.9) | 0.019 |
| Amiodarone | 132 (18.4) | 116 (20.0) | 16 (11.5) | 0.021 |
| Beta-blockers | 584 (81.3) | 471 (81.3) | 113 (81.3) | 0.99 |
| Digoxin | 95 (13.2) | 78 (13.5) | 17 (12.2) | 0.70 |
| Diuretics | 438 (61.0) | 356 (61.5) | 82 (59.0) | 0.59 |
| Statins | 479 (66.7) | 415 (71.7) | 64 (46.0) | <0.001 |
aResults are presented as numbers (percentages) unless otherwise indicated.
bCoronary artery disease.
cNew York Heart Association functional class.
dLeft ventricular ejection fraction.
eCardiac resynchronization therapy.
fAppropriate and inappropriate shocks received between implantation and 12 months follow-up.
1n = 592
2n = 668
3n = 698
Anxiety
Multivariate analysis of variance for repeated measures showed a statistically significant difference in anxiety scores between women and men (F(1,716) = 4.67, P= 0.031). At baseline, women reported higher mean levels compared with men (40.1 ± 12.1 vs. 37.5 ± 11.7; t(716) = −2.33, P= 0.02), however, this was not significant after a Bonferroni correction (P> 0.006). Similarly, at 12 months women reported non-significantly higher mean levels of anxiety compared with men (36.5 ± 12.3 vs. 34.8 ± 11.79; t(716)= −1.49, P= 0.14). Gender exerted a stable effect on anxiety, as indicated by the non-significant interaction effect for time by gender (F(1,716) = 0.76, P= 0.39). Generally, anxiety scores decreased over time, as indicated by a significant main effect for time (F(1,716) = 34.90, P< 0.001).
After adjustment for age, marital status, education, and working status, ICD indication CRT, CAD, diabetes, smoking, shocks, and cardiac- and psychotropic medication, MANCOVA for repeated measures showed no statistically significant difference in mean anxiety scores between women and men (F(1,696) = 2.67, P= 0.10) (Table 2). As listed in Table 2, age (F(1,696) = 7.85, P= 0.005), lower education (F(1,696) = 18.81, P< 0.001), working status (yes) (F(1,696) = 10.14, P= 0.002), smoking (F(1,696) = 3.91, P= 0.048), diabetes (F(1,696) = 5.17, P= 0.023), Type D personality (F(1,696) = 152.48, P< 0.001), and use of psychotropic medication (F(1,696) = 26.23, P= < 0.001) were independently associated with anxiety. The main results did not change when adding NYHA functional class as a covariate to the first model.
Influence of gender on anxiety and quality of life (multivariate analysis of covariance for repeated measures)
| . | PF . | SF . | RP . | RE . | MH . | VT . | BP . | GH . | Anxiety . |
|---|---|---|---|---|---|---|---|---|---|
| . | F . | F . | F . | F . | F . | F . | F . | F . | F . |
| Time | 3.07 | 1.03 | 5.14§ | 4.66§ | 11.36§ | 0.64 | 2.61 | 2.75 | 2.42 |
| Gender | 7.14§ | 0.73 | 1.50 | 0.88 | 0.25 | 4.88§ | 2.65 | 0.20 | 2.67 |
| Age | 1.46 | 8.12§ | 2.32 | 7.74§ | 3.10 | 8.39§ | 1.10 | 14.12|| | 7.85§ |
| Marital status (yes) | 0.12 | 0.11 | 0.15 | 1.58 | 0.00 | 1.64 | 0.86 | 0.60 | 0.00 |
| Smoking | 3.44 | 3.45 | 2.28 | 3.30 | 3.31 | 7.08§ | 2.05 | 4.06§ | 3.91§ |
| Education (low) | 10.71|| | 1.92 | 9.82# | 17.84# | 12.67|| | 13.04|| | 5.31§ | 2.58 | 18.81# |
| Working status (yes) | 16.28# | 14.88# | 13.54|| | 19.76# | 0.01 | 5.05§ | 2.84 | 12.69|| | 10.14|| |
| Site of implantation | 0.93 | 4.56§ | 0.38 | 1.41 | 5.08§ | 4.55§ | 0.38 | 0.91 | 1.93 |
| Indication | 0.10 | 0.00 | 0.01 | 0.00 | 0.11 | 0.53 | 0.20 | 0.38 | 0.46 |
| CADa | 1.36 | 0.66 | 2.01 | 0.43 | 0.38 | 0.06 | 3.06 | 5.14§ | 0.23 |
| CRTb | 10.80|| | 0.35 | 11.06|| | 2.89 | 4.15§ | 14.82# | 0.01 | 11.99|| | 1.46 |
| Shocksc | 0.08 | 0.88 | 1.35 | 0.65 | 0.15 | 0.09 | 0.02 | 0.97 | 2.47 |
| Diabetes | 17.23# | 9.86§ | 10.14§ | 9.72§ | 0.93 | 11.77§ | 6.79 | 14.97|| | 5.17§ |
| Type D personality | 10.70|| | 33.72# | 15.67# | 34.08# | 122.96# | 35.76# | 9.07|| | 45.16# | 152.47# |
| Psychotropics | 13.70# | 22.49# | 12.08§ | 8.98§ | 38.02# | 21.77# | 27.59# | 12.55§ | 26.23# |
| ACE-inhibitors | 0.08 | 1.79 | 0.32 | 0.44 | 4.34§ | 0.28 | 3.13 | 0.14 | 0.19 |
| Amiodarone | 1.99 | 2.32 | 0.06 | 0.05 | 0.20 | 0.97 | 0.45 | 0.89 | 1.22 |
| Beta-blockers | 0.26 | 0.08 | 2.76 | 0.27 | 0.41 | 0.07 | 0.17 | 4.32§ | 0.23 |
| Digoxin | 0.30 | 1.80 | 0.15 | 0.00 | 0.58 | 0.58 | 1.48 | 2.61 | 2.30 |
| Diuretics | 22.38# | 10.70|| | 11.55|| | 1.75 | 0.23 | 9.57|| | 4.30§ | 10.94|| | 1.13 |
| Statins | 0.12 | 1.80 | 0.19 | 1.30 | 0.00 | 0.00 | 0.36 | 0.70 | 0.17 |
| . | PF . | SF . | RP . | RE . | MH . | VT . | BP . | GH . | Anxiety . |
|---|---|---|---|---|---|---|---|---|---|
| . | F . | F . | F . | F . | F . | F . | F . | F . | F . |
| Time | 3.07 | 1.03 | 5.14§ | 4.66§ | 11.36§ | 0.64 | 2.61 | 2.75 | 2.42 |
| Gender | 7.14§ | 0.73 | 1.50 | 0.88 | 0.25 | 4.88§ | 2.65 | 0.20 | 2.67 |
| Age | 1.46 | 8.12§ | 2.32 | 7.74§ | 3.10 | 8.39§ | 1.10 | 14.12|| | 7.85§ |
| Marital status (yes) | 0.12 | 0.11 | 0.15 | 1.58 | 0.00 | 1.64 | 0.86 | 0.60 | 0.00 |
| Smoking | 3.44 | 3.45 | 2.28 | 3.30 | 3.31 | 7.08§ | 2.05 | 4.06§ | 3.91§ |
| Education (low) | 10.71|| | 1.92 | 9.82# | 17.84# | 12.67|| | 13.04|| | 5.31§ | 2.58 | 18.81# |
| Working status (yes) | 16.28# | 14.88# | 13.54|| | 19.76# | 0.01 | 5.05§ | 2.84 | 12.69|| | 10.14|| |
| Site of implantation | 0.93 | 4.56§ | 0.38 | 1.41 | 5.08§ | 4.55§ | 0.38 | 0.91 | 1.93 |
| Indication | 0.10 | 0.00 | 0.01 | 0.00 | 0.11 | 0.53 | 0.20 | 0.38 | 0.46 |
| CADa | 1.36 | 0.66 | 2.01 | 0.43 | 0.38 | 0.06 | 3.06 | 5.14§ | 0.23 |
| CRTb | 10.80|| | 0.35 | 11.06|| | 2.89 | 4.15§ | 14.82# | 0.01 | 11.99|| | 1.46 |
| Shocksc | 0.08 | 0.88 | 1.35 | 0.65 | 0.15 | 0.09 | 0.02 | 0.97 | 2.47 |
| Diabetes | 17.23# | 9.86§ | 10.14§ | 9.72§ | 0.93 | 11.77§ | 6.79 | 14.97|| | 5.17§ |
| Type D personality | 10.70|| | 33.72# | 15.67# | 34.08# | 122.96# | 35.76# | 9.07|| | 45.16# | 152.47# |
| Psychotropics | 13.70# | 22.49# | 12.08§ | 8.98§ | 38.02# | 21.77# | 27.59# | 12.55§ | 26.23# |
| ACE-inhibitors | 0.08 | 1.79 | 0.32 | 0.44 | 4.34§ | 0.28 | 3.13 | 0.14 | 0.19 |
| Amiodarone | 1.99 | 2.32 | 0.06 | 0.05 | 0.20 | 0.97 | 0.45 | 0.89 | 1.22 |
| Beta-blockers | 0.26 | 0.08 | 2.76 | 0.27 | 0.41 | 0.07 | 0.17 | 4.32§ | 0.23 |
| Digoxin | 0.30 | 1.80 | 0.15 | 0.00 | 0.58 | 0.58 | 1.48 | 2.61 | 2.30 |
| Diuretics | 22.38# | 10.70|| | 11.55|| | 1.75 | 0.23 | 9.57|| | 4.30§ | 10.94|| | 1.13 |
| Statins | 0.12 | 1.80 | 0.19 | 1.30 | 0.00 | 0.00 | 0.36 | 0.70 | 0.17 |
PF, Physical Functioning; SF, Social Functioning; RP, Role Physical Functioning; RE, Role Emotional Functioning; MH, Mental Health; VT, Vitality; BP, Bodily Pain; GH, General Health.
aCoronary artery disease.
bCardiac resynchronization therapy.
cBoth appropriate and inappropriate shocks received between implantation and 12 months follow-up.
§P < 0.05; ||P < 0.01; #P < 0.001.
Influence of gender on anxiety and quality of life (multivariate analysis of covariance for repeated measures)
| . | PF . | SF . | RP . | RE . | MH . | VT . | BP . | GH . | Anxiety . |
|---|---|---|---|---|---|---|---|---|---|
| . | F . | F . | F . | F . | F . | F . | F . | F . | F . |
| Time | 3.07 | 1.03 | 5.14§ | 4.66§ | 11.36§ | 0.64 | 2.61 | 2.75 | 2.42 |
| Gender | 7.14§ | 0.73 | 1.50 | 0.88 | 0.25 | 4.88§ | 2.65 | 0.20 | 2.67 |
| Age | 1.46 | 8.12§ | 2.32 | 7.74§ | 3.10 | 8.39§ | 1.10 | 14.12|| | 7.85§ |
| Marital status (yes) | 0.12 | 0.11 | 0.15 | 1.58 | 0.00 | 1.64 | 0.86 | 0.60 | 0.00 |
| Smoking | 3.44 | 3.45 | 2.28 | 3.30 | 3.31 | 7.08§ | 2.05 | 4.06§ | 3.91§ |
| Education (low) | 10.71|| | 1.92 | 9.82# | 17.84# | 12.67|| | 13.04|| | 5.31§ | 2.58 | 18.81# |
| Working status (yes) | 16.28# | 14.88# | 13.54|| | 19.76# | 0.01 | 5.05§ | 2.84 | 12.69|| | 10.14|| |
| Site of implantation | 0.93 | 4.56§ | 0.38 | 1.41 | 5.08§ | 4.55§ | 0.38 | 0.91 | 1.93 |
| Indication | 0.10 | 0.00 | 0.01 | 0.00 | 0.11 | 0.53 | 0.20 | 0.38 | 0.46 |
| CADa | 1.36 | 0.66 | 2.01 | 0.43 | 0.38 | 0.06 | 3.06 | 5.14§ | 0.23 |
| CRTb | 10.80|| | 0.35 | 11.06|| | 2.89 | 4.15§ | 14.82# | 0.01 | 11.99|| | 1.46 |
| Shocksc | 0.08 | 0.88 | 1.35 | 0.65 | 0.15 | 0.09 | 0.02 | 0.97 | 2.47 |
| Diabetes | 17.23# | 9.86§ | 10.14§ | 9.72§ | 0.93 | 11.77§ | 6.79 | 14.97|| | 5.17§ |
| Type D personality | 10.70|| | 33.72# | 15.67# | 34.08# | 122.96# | 35.76# | 9.07|| | 45.16# | 152.47# |
| Psychotropics | 13.70# | 22.49# | 12.08§ | 8.98§ | 38.02# | 21.77# | 27.59# | 12.55§ | 26.23# |
| ACE-inhibitors | 0.08 | 1.79 | 0.32 | 0.44 | 4.34§ | 0.28 | 3.13 | 0.14 | 0.19 |
| Amiodarone | 1.99 | 2.32 | 0.06 | 0.05 | 0.20 | 0.97 | 0.45 | 0.89 | 1.22 |
| Beta-blockers | 0.26 | 0.08 | 2.76 | 0.27 | 0.41 | 0.07 | 0.17 | 4.32§ | 0.23 |
| Digoxin | 0.30 | 1.80 | 0.15 | 0.00 | 0.58 | 0.58 | 1.48 | 2.61 | 2.30 |
| Diuretics | 22.38# | 10.70|| | 11.55|| | 1.75 | 0.23 | 9.57|| | 4.30§ | 10.94|| | 1.13 |
| Statins | 0.12 | 1.80 | 0.19 | 1.30 | 0.00 | 0.00 | 0.36 | 0.70 | 0.17 |
| . | PF . | SF . | RP . | RE . | MH . | VT . | BP . | GH . | Anxiety . |
|---|---|---|---|---|---|---|---|---|---|
| . | F . | F . | F . | F . | F . | F . | F . | F . | F . |
| Time | 3.07 | 1.03 | 5.14§ | 4.66§ | 11.36§ | 0.64 | 2.61 | 2.75 | 2.42 |
| Gender | 7.14§ | 0.73 | 1.50 | 0.88 | 0.25 | 4.88§ | 2.65 | 0.20 | 2.67 |
| Age | 1.46 | 8.12§ | 2.32 | 7.74§ | 3.10 | 8.39§ | 1.10 | 14.12|| | 7.85§ |
| Marital status (yes) | 0.12 | 0.11 | 0.15 | 1.58 | 0.00 | 1.64 | 0.86 | 0.60 | 0.00 |
| Smoking | 3.44 | 3.45 | 2.28 | 3.30 | 3.31 | 7.08§ | 2.05 | 4.06§ | 3.91§ |
| Education (low) | 10.71|| | 1.92 | 9.82# | 17.84# | 12.67|| | 13.04|| | 5.31§ | 2.58 | 18.81# |
| Working status (yes) | 16.28# | 14.88# | 13.54|| | 19.76# | 0.01 | 5.05§ | 2.84 | 12.69|| | 10.14|| |
| Site of implantation | 0.93 | 4.56§ | 0.38 | 1.41 | 5.08§ | 4.55§ | 0.38 | 0.91 | 1.93 |
| Indication | 0.10 | 0.00 | 0.01 | 0.00 | 0.11 | 0.53 | 0.20 | 0.38 | 0.46 |
| CADa | 1.36 | 0.66 | 2.01 | 0.43 | 0.38 | 0.06 | 3.06 | 5.14§ | 0.23 |
| CRTb | 10.80|| | 0.35 | 11.06|| | 2.89 | 4.15§ | 14.82# | 0.01 | 11.99|| | 1.46 |
| Shocksc | 0.08 | 0.88 | 1.35 | 0.65 | 0.15 | 0.09 | 0.02 | 0.97 | 2.47 |
| Diabetes | 17.23# | 9.86§ | 10.14§ | 9.72§ | 0.93 | 11.77§ | 6.79 | 14.97|| | 5.17§ |
| Type D personality | 10.70|| | 33.72# | 15.67# | 34.08# | 122.96# | 35.76# | 9.07|| | 45.16# | 152.47# |
| Psychotropics | 13.70# | 22.49# | 12.08§ | 8.98§ | 38.02# | 21.77# | 27.59# | 12.55§ | 26.23# |
| ACE-inhibitors | 0.08 | 1.79 | 0.32 | 0.44 | 4.34§ | 0.28 | 3.13 | 0.14 | 0.19 |
| Amiodarone | 1.99 | 2.32 | 0.06 | 0.05 | 0.20 | 0.97 | 0.45 | 0.89 | 1.22 |
| Beta-blockers | 0.26 | 0.08 | 2.76 | 0.27 | 0.41 | 0.07 | 0.17 | 4.32§ | 0.23 |
| Digoxin | 0.30 | 1.80 | 0.15 | 0.00 | 0.58 | 0.58 | 1.48 | 2.61 | 2.30 |
| Diuretics | 22.38# | 10.70|| | 11.55|| | 1.75 | 0.23 | 9.57|| | 4.30§ | 10.94|| | 1.13 |
| Statins | 0.12 | 1.80 | 0.19 | 1.30 | 0.00 | 0.00 | 0.36 | 0.70 | 0.17 |
PF, Physical Functioning; SF, Social Functioning; RP, Role Physical Functioning; RE, Role Emotional Functioning; MH, Mental Health; VT, Vitality; BP, Bodily Pain; GH, General Health.
aCoronary artery disease.
bCardiac resynchronization therapy.
cBoth appropriate and inappropriate shocks received between implantation and 12 months follow-up.
§P < 0.05; ||P < 0.01; #P < 0.001.
In secondary analyses, we examined the influence of appropriate and inappropriate shocks on anxiety separately. Only appropriate shocks (F(1,696) = 5.46, P= 0.02) but not inappropriate shocks (F(1,696) = 2.16, P= 0.14) were associated with anxiety. The predictive value of the other variables did not change (results not shown).
Quality of life
Multivariate analysis of variance for repeated measures showed significantly different scores on the PF (F(1,716) = 8.31, P= 0.004) and the VT (F(1,716) = 9.36, P= 0.002) domains for women and men. At baseline, women reported significantly poorer QoL compared with men on only two of the eight domains; PF (49.41 ± 28.90 vs. 58.54 ± 26.54; t(716) = 3.58, P< 0.001) and VT (48.91 ± 21.57 vs. 56.29 ± 22.72; t(716)= 3.47, P= 0.001). At 12 months, women still reported poorer QoL on the VT domain (55.96 ± 22.97 vs. 60.10 ± 21.98; t(716) = 1.98, P= 0.048). No statistically significant differences were found on the other 6 QoL domains at baseline and 7 QoL domains at 12 months, indicating that women and men with an ICD do not substantially differ in experienced QoL. Gender exerted a stable effect on outcome, as indicated by a non-significant time by sex interaction (F(1,716) = 1.12, P= 0.35). Quality of life improved over time as indicated by a significant main effect (F(1,716) = 23.54, P< 0.001).
In adjusted analysis, the significant differences in PF (F(1,696) = 7.14, P= 0.008) and VT (F(1,696) = 4.88, P= 0.028) between women and men remained as observed in univariate analysis. Age, lower education, working status, diabetes, CRT, Type D personality, use of psychotropic medication, and diuretics were associated with four or more domains of QoL (Table 2). The main results did not change when adding NYHA class as a covariate to the first model. However, NYHA class was associated with QoL (>4 domains).
In secondary analyses, we examined the influence of appropriate and inappropriate shock on QoL. Secondary analyses revealed that appropriate shocks were only associated with the GH domain of the SF-36 (F(1,696) = 4.46, P= 0.03), but not to the other domains; inappropriate shocks were not related to any domain. The independent associations of the other variables with QoL domains did not change (results not shown).
Relative influence of gender, New York Heart Association functional class III/IV, implantable cardioverter–defibrillator shocks, and Type D personality on outcomes
In Figure 1, the effect sizes are displayed for the magnitude of the influence of gender, NYHA class, shocks, and Type D personality on anxiety at baseline and at 12 months. As indicated by Cohen's effect size index, the influence of gender on anxiety, both at baseline and 12 months follow-up, was small with effect sizes of 0.22 and 0.14, respectively. Small effect sizes were also found for the influence of NYHA class and ICD shocks (appropriate and inappropriate) on anxiety at both time points. A large effect size for Type D personality was found. Furthermore, the results show that the relative influence of gender is less than that of NYHA class, ICD shocks, and personality in particular in relation to 12-month anxiety outcomes. For QoL, the effect sizes for gender were also small, while the influence of NYHA class and Type D personality on QoL was moderate to large both at baseline and at 12 months follow-up (Figure 2).
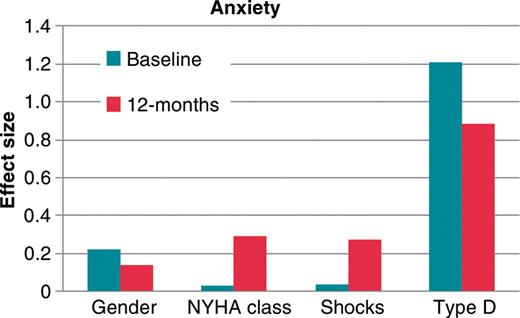
Effect sizes (Cohen's d) for the magnitude of the influence of gender, New York Heart Association class III/IV, implantable cardioverter–defibrillator shocks, and Type D personality on anxiety at baseline and at 12 months.
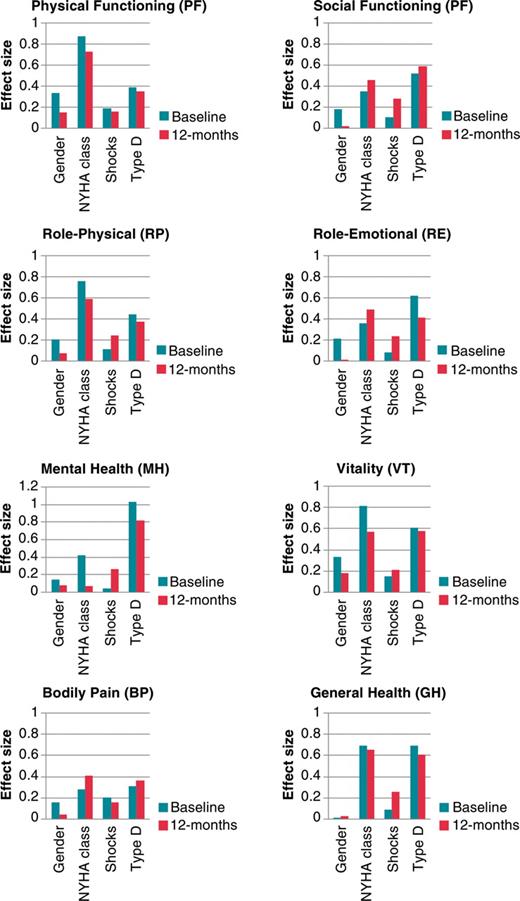
Effect sizes (Cohen's d) for the magnitude of the influence of gender, New York Heart Association class III/IV, implantable cardioverter–defibrillator shocks, and Type D personality on quality of life at baseline and at 12 months.
Discussion
In the current study, women experienced more anxiety compared with men, but after statistical adjustment for potential confounders the influence of gender on anxiety was no longer significant. Women only reported poorer QoL on two of the eight SF-36 subscales, that is, PF and VT, with this gender difference remaining after adjusting for potential confounders. Our findings showed that the relative influence of gender on anxiety and QoL is less than that of NYHA class and Type D personality.
The results of this study are in line with previous research showing that women may report higher anxiety levels compared with men but that these differences may be attributed to other factors and therefore not hold when adjusting for potential confounders.25,46 In this study, a difference between gender was only observed in univariate but not in multivariate analysis. The univariate difference could be explained by the generally younger age of women in this sample. Previous studies have shown that younger ICD patients tend to experience more psychological difficulties than older patients.21 Another explanation could be that women in this sample were more likely not to have a partner. Women are more likely to seek social support from their network when dealing with stressful situations.27 Therefore, women may be more likely to suffer from ICD-related distress in the absence of appropriate support. Our findings on QoL are in line with previous research showing that there are gender differences on some but not all domains of the SF-36 after controlling for potential confounders.30,34 Taken together, based on previous research and our findings, it seems that women and men overall tend to adapt almost equally well post-ICD implantation. Shocks in general were not associated with the outcomes, but differentiating between appropriate and inappropriate shocks appropriate shocks were associated with anxiety and the GH domain of the SF-36. These findings are in line with previous studies reporting mixed findings on the effect of shocks on patient-centred outcomes.14,37
Studies in other cardiac populations have also focused on gender differences and psychological distress. For example in one study, women experienced greater negative mood state and perceived less control over their health compared with men. However, no gender differences were found on the QoL-associated domains.47 Among patients post-myocardial infarction women were more likely to report poor QoL compared with men.48 In patients with coronary heart disease and comorbid depression, women were more likely to be anxious compared with men.49 Based on these findings, it seems that gender differences may vary across the different cardiac diseases and that the underlying disease is of importance when examining gender differences. In the current study, we also found that symptomatic heart failure (NYHA class III–IV) had a larger influence on both anxiety and QoL than gender.
Few previous studies have included potential mediators, such as somatosensory amplification (i.e. being more aware of bodily sensations and perceiving normal somatic sensations as more intense),29,46 that may explain gender disparities in outcome.29,46 The influence of the patient's pre-implantation psychological profile has to date also not been taken into account when focusing on gender disparities, while the patient's personality rather than gender may explain individual differences in patient-reported outcomes.2,25 In this study, we found Type D personality to be a strong and independent determinant of both anxiety and QoL, which was expected.32,50 Besides these variables future studies should also consider patients’ educational level, working status, comorbidities (e.g. diabetes), and use of (psychotropic) medication. In our sample, these variables were all associated with both anxiety and QoL.
Our findings have some implications for future research. Given the mixed results in the current and previous studies, we believe that it is premature to conclude that gender per se is a predictor for disparities in anxiety and QoL. Hence, before we start developing gender-specific interventions, we should try to elucidate whether these mixed findings are due to methodological issues and if gender disparities are present to search for the mechanisms that may account for these disparities, such as differences in e.g. socio-economic status, pre-implantation psychological profile, somatosensory amplification, etc.
The limitations of the study must also be acknowledged. First, anxiety was assessed with a standardized self-report measure rather than a clinical diagnostic interview. Hence, we are only able to draw conclusions with respect to the influence of gender on symptoms of anxiety and not a clinical diagnosis of anxiety. Secondly, information on symptomatic heart failure, as assessed with NYHA functional class, was not available for all patients, and was therefore only included in secondary analysis leading to a smaller number of patients included in this analysis (n= 592). Thirdly, due to the use of different measures for depression in the two samples that were combined in this study, we were not able to examine potential gender differences in depression. Fourthly, we used a generic rather than a disease-specific measure of QoL, which may have been less sensitive to tap differences between gender if present. Fifthly, due to a relatively high dropout rate and missing data we could only include 718 (66.5%) of the patients in analyses. However, the excluded patient did not differ systematically on any of the study variables as compared with included patients. Hence, we assume that this limitation had no significant bearing on our findings. This study also has several strengths. These include the prospective study design, the use of a real-world population rather than a selected sample, and the relatively large sample size, increasing the chance that the study was sufficiently powered to find possible differences between men and women if present, and also enabling us to control statistically for potential demographic, clinical, and psychological confounders that may impinge on the relationship between gender and the outcomes examined.
Conclusion
Our findings indicate that women and men tend to adapt equally well to living with an ICD and that the patient's personality and the presence of symptomatic heart failure may have a larger influence on anxiety and QoL than gender and ICD shocks. Large-scale studies are warranted to replicate these findings focusing also on gender-specific aspects, such as somatosensory amplification, that might serve to explain gender disparities in patient-reported outcomes.
Conflict of interest: none declared.
Funding
This work was supported by a VENI (451-05-001) grant to S.S.P. and a VICI grant (453-04-004) to Dr Johan Denollet from the Netherlands Organisation for Scientific Research (NWO), and a VIDI grant (91710393) grant no. 300020002 to S.S.P. from the Netherlands Organisation for Health Research and Development (ZonMw), The Hague, The Netherlands.
Acknowledgements
We would like to thank Eefje Postelmans, Hidde Weetink, Agnes Muskens-Heemskerk, Simone Traa, and Belinda de Lange for inclusion of the patients into the study.



