-
PDF
- Split View
-
Views
-
Cite
Cite
Vineet Wadehra, Alfred E. Buxton, Antonios P. Antoniadis, James W. McCready, Calum J. Redpath, Oliver R. Segal, Edward Rowland, Martin D. Lowe, Pier D. Lambiase, Anthony W.C. Chow, The use of a novel nitinol guidewire to facilitate transseptal puncture and left atrial catheterization for catheter ablation procedures, EP Europace, Volume 13, Issue 10, October 2011, Pages 1401–1405, https://doi.org/10.1093/europace/eur155
Close - Share Icon Share
Abstract
An increasing number of transseptal punctures (TSPs) are performed worldwide for atrial ablations. Transseptal punctures can be complex and can be associated with potentially life threatening complications. The purpose of the study was to evaluate the safety and efficacy of a novel transseptal guidewire (TSGW) designed to facilitate TSPs.
Transseptal punctures were performed using a SafeSept™ TSGW passed through a standard TSP apparatus. Transseptal punctures were performed by standard technique with additional use of a TSGW allowing probing of the interatrial septum without needle exposure and penetration of the fossa into the left atrium (LA). Transseptal puncture using the TSGW was performed in 210 patients. Left atrial access was achieved successfully in 205 of 210 patients (97.6%) and in 96.3% of patients undergoing repeat TSP. Left atrial access was achieved with the first pass in 81.2% (mean 1.4 ± 0.9 passes, range 1–6) using the TSGW. No serious complications were attributable to the use of the TSGW, even in cases of failed TSP.
The TSGW is associated with a high success rate for TSP and may be a useful alternative to transoesophageal or intracardiac echocardiogram-guided TSP.
Introduction
Percutaneous transseptal puncture (TSP) was first performed in the 1950s to allow direct access to the left cardiac chambers by making a passage through the fossa ovalis from the right atrium.1 The procedure was developed to perform haemodynamic studies of the left heart and subsequently modified for percutaneous balloon mitral valvotomy. In recent years, most TSPs are performed by electrophysiologists for catheter ablation of atrial fibrillation (AF).2 The increasing success and expansion of catheter ablation therapy for AF has resulted in an increasing number of TSPs performed worldwide.3 This will inevitably lead to TSPs being performed in lower volume centres with cases of varying complexity.
Complications are reported to occur in up to 6% of patients undergoing TSP.2,4 These include potentially life-threatening complications such as cardiac and aortic root perforations, tamponade, and arterial thrombo-embolism. Complications predominantly arise as a result of the relatively small target area for puncture on the interatrial septum that can be <0.5 cm2 and the marked anatomical variations between patients. Various strategies have been implemented to improve the safety of the procedure, including land-marking key anatomical positions with diagnostic electrophysiology catheters5 and right atrial angiography, particularly in patients suspected of having unusual anatomy.6 In addition to conventional fluoroscopy, imaging modalities such as transoesophageal echocardiography (TEE) or intracardiac echocardiography (ICE) provide direct visual guidance during TSP to improve safety.7,8 However, many centres do not have the expertise nor imaging tools available that require additional resources and cost.
Significant proportions of AF patients, especially those with persistent AF, require more than one ablation procedure and consequently multiple TSPs may be required.9 It is also recognized that repeat TSP is associated with higher risk of adverse events and increased failure rates.10–12
We describe our initial experience of using a novel transseptal guidewire (TSGW) to aid TSP. This wire has been designed to improve TSP success rates, with particular focus on improving safety, especially in previously failed or difficult cases.
Methods
From June 2008 to May 2010, TSPs using a custom-designed TSGW (SafeSept™, Pressure Products Inc., San Pedro, CA, USA) were evaluated at The Heart Hospital, University College Hospital NHS Foundation Trust, London, UK and at Brown University, Providence, RI, USA.
Transseptal puncture using transseptal guidewire
In patients undergoing AF ablation, TEE was performed to exclude the presence of left atrial thrombus and to look for patent foramina ovale. If the septum was intact, TSP was performed with the TSGW and standard transseptal equipment using a modified Brockenbrough approach described below.
Transseptal guidewire
The TSGW is a 0.014 inch nitinol wire with a sharp distal tip and preformed ‘J’ shape. This was introduced through the inner lumen of a standard Brockenbrough transseptal needle to penetrate the interatrial septum into the left atrium (LA). The guidewire is then advanced straightened, through the standard transseptal needle using an introducer. The outer needle and sheath giving the sharpened tip direction and a column support required to cross the septum. On crossing the septum, the wire immediately returns to its preformed ‘J’ shape. This design feature renders the tip atraumatic, reducing the risk of potential injury or perforation of the LA.
Transseptal puncture technique
A quadripolar or decapolar catheter was inserted into the coronary sinus via a femoral sheath. A standard transseptal sheath (Agilis NXT/SL0/SL1, St Jude Medical Inc., St Paul, MN, USA; Channel sheath, Bard electrophysiology, Lowell, MA, USA) was advanced to the superior vena cava from the femoral vein using an over-the-wire technique and a Brockenbrough transseptal needle (BRK or BRK1, St Jude Medical Inc., St Paul, MN, USA) introduced and advanced to just proximal to the sheath tip. The sheath and un-exposed needle were slowly pulled down from the superior vena cava with the sheath and needle in a 4–6 o'clock orientation in the left anterior oblique projection under fluoroscopic guidance until the sheath dropped into the fossa ovalis. A TSGW (SafeSept™, Pressure Products Inc., San Pedro, CA, USA) was then inserted into the Brockenbrough needle and advanced to the unexposed tip. The position of the sheath assembly was examined in the right anterior oblique projection to ensure it lies centrally on the interatrial septum posterior to the coronary sinus catheter and anterior to the posterior heart border. The TSGW was then advanced onto the septum and through into the LA. If the wire is pushed in an incorrect position outside the fossa ovalis, crumpling and resistance is encountered, and an attempt using a different orientation is required, thus acting as a probing wire. If passage through the septum into the LA is achieved, the guidewire passes effortlessly without resistance in its pre-formed ‘J’ shape through the left atrial chamber, usually into the left superior pulmonary vein (Figure 1A). The radio-opaque platinum proximal shaft of the guidewire provides fluoroscopic confirmation of the position of the TSGW. The stiffer proximal portion of the TSGW provides tracking and additional support for the passage of the rest of the TSP apparatus. The needle and then the dilator and sheath are then passed into the LA using an over-the-wire technique (Figure 1B). If penetration fails with the TSGW, further attempts in a different orientation are then needed and may require a further pass of the transseptal apparatus from the superior vena cava. For double transseptal access, the second TSP is performed in a similar manner using the same TSGW and Brockenbrough needle with a second transseptal sheath. Following successful transseptal access to the LA, a bolus of intravenous weight-adjusted heparin (100 IU/kg) is administered and doses given later to keep the activated clotting times above 300 s throughout the procedure.
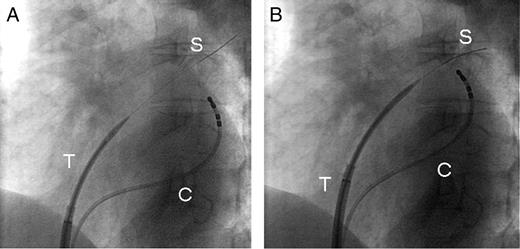
(A) This is a fluoroscopic image showing the transseptal sheath positioned on the fossa ovalis in a 30° left anterior oblique position without advancing the needle. The SafeSept™ wire is seen penetrating the interatrial septum and the TSGW is then passed into the left superior pulmonary vein. (B) The dilator portion of the sheath is then advanced over the TSGW, later followed by the outer transseptal sheath. S represents the TSGW (SafeSept™), T the transseptal sheath, and C the quadrapolar coronary sinus catheter used for land-marking.
Results
Between June 2008 and May 2010, TSP using the SafeSept™ TSGW was evaluated in 210 consecutive unselected patients. Baseline characteristics of the study population are summarized in Table 1. The majority of cases were performed for AF/atrial tachycardia ablation. Left atrial diameter was enlarged at 43 ± 7 mm. Successful LA access using the TSGW was achieved in 205 patients (97.6%). One hundred and thirty patients (61.9%) underwent TSP for the first time and 80 patients (38.1%) had previously undergone TSP. There was no difference in the success rates between these groups (Table 2). Left atrial access was achieved with the first pass in 81.2% (mean 1.4 ± 0.9 passes, range 1–6) using the TSGW. In successful cases, the mean number of passes required to achieve LA access was 1.4 ± 0.9 for patients undergoing TSP for the first time and 1.3 ± 0.8 for those having previously undergone TSP.
| Age (years) | |
| Mean | 60.2 ± 11.9 |
| Range | 19.4–84 |
| Sex (male : female), n (%) | 142 (67.6%) : 68 (32.4%) |
| Mean left atrial diameter (mm) | 43 ± 7 |
| Indications for TSP, n (%) | |
| Paroxysmal AF | 86 (41.0%) |
| Persistent AF | 78 (37.1%) |
| Left atrial tachycardia/flutter | 27 (12.9%) |
| Accessory pathway | 15 (7.1%) |
| Ventricular tachycardia | 4 (1.9%) |
| Age (years) | |
| Mean | 60.2 ± 11.9 |
| Range | 19.4–84 |
| Sex (male : female), n (%) | 142 (67.6%) : 68 (32.4%) |
| Mean left atrial diameter (mm) | 43 ± 7 |
| Indications for TSP, n (%) | |
| Paroxysmal AF | 86 (41.0%) |
| Persistent AF | 78 (37.1%) |
| Left atrial tachycardia/flutter | 27 (12.9%) |
| Accessory pathway | 15 (7.1%) |
| Ventricular tachycardia | 4 (1.9%) |
AF, atrial fibrillation; TSP, transseptal puncture.
| Age (years) | |
| Mean | 60.2 ± 11.9 |
| Range | 19.4–84 |
| Sex (male : female), n (%) | 142 (67.6%) : 68 (32.4%) |
| Mean left atrial diameter (mm) | 43 ± 7 |
| Indications for TSP, n (%) | |
| Paroxysmal AF | 86 (41.0%) |
| Persistent AF | 78 (37.1%) |
| Left atrial tachycardia/flutter | 27 (12.9%) |
| Accessory pathway | 15 (7.1%) |
| Ventricular tachycardia | 4 (1.9%) |
| Age (years) | |
| Mean | 60.2 ± 11.9 |
| Range | 19.4–84 |
| Sex (male : female), n (%) | 142 (67.6%) : 68 (32.4%) |
| Mean left atrial diameter (mm) | 43 ± 7 |
| Indications for TSP, n (%) | |
| Paroxysmal AF | 86 (41.0%) |
| Persistent AF | 78 (37.1%) |
| Left atrial tachycardia/flutter | 27 (12.9%) |
| Accessory pathway | 15 (7.1%) |
| Ventricular tachycardia | 4 (1.9%) |
AF, atrial fibrillation; TSP, transseptal puncture.
| . | Patients without previous history of TSP . | Patients with previous history of TSP . |
|---|---|---|
| Number of patients, n | 130 | 80 |
| Successful LA access obtained with TSGW (%) | 98.4 | 96.3 |
| First pass success with TSGW (%) | 82.2 | 79.7 |
| Number of passes with TSGW required for LA access (mean ± standard deviation) | 1.4 ± 0.9 | 1.3 ± 0.8 |
| . | Patients without previous history of TSP . | Patients with previous history of TSP . |
|---|---|---|
| Number of patients, n | 130 | 80 |
| Successful LA access obtained with TSGW (%) | 98.4 | 96.3 |
| First pass success with TSGW (%) | 82.2 | 79.7 |
| Number of passes with TSGW required for LA access (mean ± standard deviation) | 1.4 ± 0.9 | 1.3 ± 0.8 |
LA, left atrium; TSGW, transseptal guidewire; TSP, transseptal puncture.
| . | Patients without previous history of TSP . | Patients with previous history of TSP . |
|---|---|---|
| Number of patients, n | 130 | 80 |
| Successful LA access obtained with TSGW (%) | 98.4 | 96.3 |
| First pass success with TSGW (%) | 82.2 | 79.7 |
| Number of passes with TSGW required for LA access (mean ± standard deviation) | 1.4 ± 0.9 | 1.3 ± 0.8 |
| . | Patients without previous history of TSP . | Patients with previous history of TSP . |
|---|---|---|
| Number of patients, n | 130 | 80 |
| Successful LA access obtained with TSGW (%) | 98.4 | 96.3 |
| First pass success with TSGW (%) | 82.2 | 79.7 |
| Number of passes with TSGW required for LA access (mean ± standard deviation) | 1.4 ± 0.9 | 1.3 ± 0.8 |
LA, left atrium; TSGW, transseptal guidewire; TSP, transseptal puncture.
Transseptal puncture using direct TEE guidance under general anaesthesia was used in 45 patients (21.4%), either because of patient preference or if a previous TSP attempt had been unsuccessful or had resulted in complication. The remaining procedures were performed under local anaesthetic and conscious sedation. Contrast and pressure monitoring were used for the initial five patients, it was deemed unhelpful and unnecessary due to damped pressure waveforms and poor opacification following contrast injection, due to the presence of the wire partially obstructing the needle lumen. Trainees performing TSP under direct supervision were primary operators in 48% of cases and senior operators performed TSP in the remainder of the cases.
Complex transseptal puncture patients
Nineteen patients with a previous history of difficult TSP had successful LA access using the standard techniques with the TSGW. This included nine patients with previously failed conventional TSP, including two patients with TEE guidance under general anaesthesia. The TSGW was also used in a further 13 patients in whom conventional TSP had been unsuccessful but LA access was successfully achieved by the same procedure with introduction of the TSGW. Left atrial access was obtained using the TSGW with the first pass in 10 (76.9%) of these cases.
Unsuccessful transseptal puncture with the transseptal guidewire
In four patients without obvious complex anatomy undergoing TSP, LA access was unsuccessful using the TSGW (Table 3). Of these, the first patient had undergone four previous TSPs during two ablation procedures for persistent AF. Following three failed passes with the TSGW, the procedure was converted to conventional TSP, which was also unsuccessful. The second patient had no prior TSP. In this case, the TSGW crumpled on the septum on the second pass and subsequent contrast injection suggested pericardial staining. On review, the orientation of the sheath was felt to be too anterior on the septum before the TSGW was advanced. The third patient had undergone four prior TSPs during two ablation procedures for paroxysmal AF and LA tachycardia. Despite apparent correct fluoroscopic positioning on the septum, the TSGW failed to cross the fossa ovalis in spite of two separate attempts. Subsequent conversion to conventional TSP by the operator without TSGW resulted in aortic puncture, with no pericardial or haemodynamic sequelae on serial echocardiography. All three cases were abandoned, without need for pericardial drainage or surgical intervention. All three patients subsequently underwent successful TSP using TSGW under TEE guidance. The fourth patient had unsuccessful TSP using a conventional approach without the TSGW followed by unsuccessful attempts using the TSGW. Left atrial access was obtained at the same sitting with a further conventional approach after sheath and needle repositioning. Intracardiac echo guidance was used throughout the case. These procedures were performed by operators experienced at TSP but with limited experience of using the TSGW. All the failed cases occurred within the first 10 procedures for each operator.
| Patient demographic . | Arrhythmia . | LA size (mm) . | Previous TSP . | Description . |
|---|---|---|---|---|
| 65-year-old man | Paroxysmal AF | 44 | 4 | TSGW failed despite three passes followed by unsuccessful TSP using a conventional approach with the Brockenbrough needle |
| 42-year-old man | Paroxysmal AF | 48 | 0 | TSGW crumpled on the initial attempt. Appeared to cross the septum on the second attempt. Pericardial staining was seen. The procedure was abandoned |
| 66-year-old woman | Persistent AF | 62 | 4 | TSGW failed despite three passes of the sheath followed by a further attempt with a conventional approach resulting in aortic puncture |
| 67-year-old woman | Paroxysmal AF | N/A | 1 | One attempt with the Brockenbrough needle was unsuccessful. TSGW was also unsuccessful. Further attempt with the Brockenbrough needle was unsuccessful |
| Patient demographic . | Arrhythmia . | LA size (mm) . | Previous TSP . | Description . |
|---|---|---|---|---|
| 65-year-old man | Paroxysmal AF | 44 | 4 | TSGW failed despite three passes followed by unsuccessful TSP using a conventional approach with the Brockenbrough needle |
| 42-year-old man | Paroxysmal AF | 48 | 0 | TSGW crumpled on the initial attempt. Appeared to cross the septum on the second attempt. Pericardial staining was seen. The procedure was abandoned |
| 66-year-old woman | Persistent AF | 62 | 4 | TSGW failed despite three passes of the sheath followed by a further attempt with a conventional approach resulting in aortic puncture |
| 67-year-old woman | Paroxysmal AF | N/A | 1 | One attempt with the Brockenbrough needle was unsuccessful. TSGW was also unsuccessful. Further attempt with the Brockenbrough needle was unsuccessful |
AF, atrial fibrillation; LA, left atrium; TSGW, transseptal guidewire; TSP, transseptal puncture.
| Patient demographic . | Arrhythmia . | LA size (mm) . | Previous TSP . | Description . |
|---|---|---|---|---|
| 65-year-old man | Paroxysmal AF | 44 | 4 | TSGW failed despite three passes followed by unsuccessful TSP using a conventional approach with the Brockenbrough needle |
| 42-year-old man | Paroxysmal AF | 48 | 0 | TSGW crumpled on the initial attempt. Appeared to cross the septum on the second attempt. Pericardial staining was seen. The procedure was abandoned |
| 66-year-old woman | Persistent AF | 62 | 4 | TSGW failed despite three passes of the sheath followed by a further attempt with a conventional approach resulting in aortic puncture |
| 67-year-old woman | Paroxysmal AF | N/A | 1 | One attempt with the Brockenbrough needle was unsuccessful. TSGW was also unsuccessful. Further attempt with the Brockenbrough needle was unsuccessful |
| Patient demographic . | Arrhythmia . | LA size (mm) . | Previous TSP . | Description . |
|---|---|---|---|---|
| 65-year-old man | Paroxysmal AF | 44 | 4 | TSGW failed despite three passes followed by unsuccessful TSP using a conventional approach with the Brockenbrough needle |
| 42-year-old man | Paroxysmal AF | 48 | 0 | TSGW crumpled on the initial attempt. Appeared to cross the septum on the second attempt. Pericardial staining was seen. The procedure was abandoned |
| 66-year-old woman | Persistent AF | 62 | 4 | TSGW failed despite three passes of the sheath followed by a further attempt with a conventional approach resulting in aortic puncture |
| 67-year-old woman | Paroxysmal AF | N/A | 1 | One attempt with the Brockenbrough needle was unsuccessful. TSGW was also unsuccessful. Further attempt with the Brockenbrough needle was unsuccessful |
AF, atrial fibrillation; LA, left atrium; TSGW, transseptal guidewire; TSP, transseptal puncture.
A further two patients required the unplanned use of TEE guidance after failure to obtain LA access despite multiple attempts using the TSGW. Transoesophageal echocardiography suggested incorrect positioning of the TSP sheath and TSGW due to unusually distorted and rotated anatomy not appreciated on fluoroscopy, and subsequent imaging-guided TSP using the TSGW was successful in both cases. We did not observe any incidence of aortic root puncture with the TSGW and no complications attributable to the use of the TSGW were observed during the evaluation period.
Finally, the TSGW failed in a complex patient with atrial tachycardia with Mustard circulation for transposition of the great arteries and ventricular septal defect having undergone a ventricular septal defect repair and systemic atrioventricular valve replacement with a mechanical prosthesis. This was done under general anaesthesia, but both conventional and TSGW attempts under TEE guidance were unsuccessful.
Discussion
This is the largest series hitherto evaluating a novel TSGW (SafeSept™) designed to facilitate safe TSP for LA access. In a recent report of 27 clinical cases TSGW was applied with absolute safety and efficacy.13 Our experience in 210 patients indicates that TSP performed using the TSGW appears safe, is associated with a high procedural success rate, and is useful in difficult cases with a previously failed conventional approach. No complications directly attributable to the use of the TSGW were observed during the evaluation period. The five cases that failed using the TSGW were a result of complex anatomy and may not have been achieved conventionally without direct imaging.
Transseptal puncture is successfully achieved in the majority of patients. However, up to 10% of cases can be complex and may either fail to cross into the LA or are associated with serious complications.2 A substantial number of centres still perform AF ablation under local anaesthesia and sedation, guided entirely by fluoroscopy and pressure monitoring. This approach may not reliably predict the safe zone for TSP or the level of difficulty that may be encountered in all cases. Direct echo guidance remains the gold standard for safety by providing visual guidance to TSP and would be invaluable for patients with rotated or unusual anatomy.8,14,15 However, even within this study, there were two patients in whom a previous conventional approach under direct TEE guidance failed to provide LA access due to resistance encountered at the septum, but LA access was successfully achieved using the TSGW. Patients with previous history of TSP are more likely to have thickened or fibrotic septa due to scarring,10 but this may not always be evident or predictable from TEE. In this study, the TSGW was successfully used without complication in 13 patients in whom a conventional approach failed and in 19 patients with a previous history of difficult or failed TSP. The design of the TSGW with a sharp nitinol tip provides a significantly higher pressure per unit area than a conventional transseptal needle. The profile of the tip allows greater penetration through the septum and the immediate formation of a ‘J' shape prevents injury or trauma to neighbouring cardiac structures once it successfully crosses into the LA. Once the tract has been made, the wire provides a safe over-the-wire approach to advancing the needle tip and sheath into the LA, proving to be particularly effective for fibrous and aneurysmal septa. In all cases of successful LA penetration by the TSGW, the remaining TSP apparatus could be advanced without problems.
The use of a small-calibre TSGW allows the operator to probe the interatrial septum with a degree of safety to find a passage into the LA, rather than probing with a larger-calibre transseptal needle. When the TSGW is not correctly positioned against the thin membranous portion of the fossa ovalis, it deforms by crumpling or is deflected along the septal wall. When this occurs it suggests that the TSP apparatus is in the wrong position or orientation that may occur due to unexpected or atypical anatomy. This requires either a further attempt in a different orientation or the need for direct imaging. This was observed in the patients in whom the TSGW failed to facilitate LA access. Two of these patients had successful TSP using the TSGW when TEE was utilized at the same sitting. Review of the unsuccessful cases using the TSGW suggests that, in all of these patients, TSP failure was due to incorrect positioning of the transseptal apparatus on the interatrial septum rather than a failure of the TSGW per se. Despite this, no serious complication occurred as a result of its use. We suggest that unsuccessful TSP using a TSGW occurs because of anatomical variability and potentially incorrect positioning of the TSP apparatus on the septum. Our experience suggests a change of strategy is often required at this point and that a direct imaging-guided approach may be safer in these instances rather than resorting to pushing with the TSP needle alone where complications may occur.
A major limitation of this study is that it is not a randomized control study comparing the TSGW and standard conventional TSP techniques, but important safety and feasibility data are gathered to test the efficacy of this new technology by experienced operators and trainees in a significant and meaningful numbers of patients.
Comparison with other technologies to assist transseptal puncture
Other technologies used for difficult TSP have been described, including a specially designed radiofrequency needle and generator to facilitate passage into LA16 and direct application of radiofrequency energy to the end of a standard Brockenbrough needle.17 Although these techniques are useful in thick fibrotic septa, if the needle is not positioned in a safe and anatomically correct position, damage to adjacent structures can still occur resulting in potentially serious complications. The TSGW represents an alternative to the radiofrequency needle, with several distinct advantages. The TSGW allows probing of the septum to find the safe region of the fossa ovalis to cross into the LA. Due to its unique design, the wire is unlikely to cause significant trauma if it traverses into an adjacent anatomical structure. Similarly, the wire will typically crumple into the septum rather than penetrate through, if the sheath is adjacent to a thickened structure (e.g. the limbus). In addition, contrast can be administered through the tip of the needle, even when the wire is in situ, and pressure can be recorded (although often damped), though in our experience this was not necessary.
Conclusion
This study of the initial experience using a novel 0.014″ nitinol TSGW for TSP suggests that the technique is safe and has a number of potential advantages over conventional TSP methods. It appears especially valuable in performing TSP in repeat transseptal procedures and in patients with unusual or distorted anatomy. In cases where the TSGW fails to cross into the LA, this is likely to be due to the TSP apparatus being positioned outside the true fossa area and repeated attempts guided by direct imaging are advisable. Further evaluation in a prospective randomized trial is required to fully validate these findings.
Conflict of interest: none declared.
Funding
This work was undertaken at UCLH/UCL, which received a proportion of funding from the UK Department of Health's National Institute for Health Research (NIHR) Biomedical Research Centre's funding scheme.
A.W.C.C. and P.D.L. received research grants from St Jude Medical and Boston Scientific Inc.



