-
PDF
- Split View
-
Views
-
Cite
Cite
Haran Burri, Chan-il Park, Marc Zimmermann, Pascale Gentil-Baron, Carine Stettler, Henri Sunthorn, Giulia Domenichini, Dipen Shah, Utility of the surface electrocardiogram for confirming right ventricular septal pacing: validation using electroanatomical mapping, EP Europace, Volume 13, Issue 1, January 2011, Pages 82–86, https://doi.org/10.1093/europace/euq332
Close - Share Icon Share
Abstract
When targeting the interventricular septum during pacemaker implantation, the lead may inadvertently be positioned on the anterior wall due to imprecise fluoroscopic landmarks. Surface electrocardiogram (ECG) criteria of the paced QRS complex (e.g. negativity in lead I) have been proposed to confirm a septal position, but these criteria have not been properly validated. Our aim was to investigate whether the paced QRS complex may be used to confirm septal lead position.
Anatomical reconstruction of the right ventricle was performed using a NavX® system in 31 patients (70 ± 11 years, 26 males) to validate pacing sites. Surface 12-lead ECGs were analysed by digital callipers and compared while pacing from a para-Hissian position, from the mid-septum, and from the anterior free wall.
Duration of the QRS complex was not significantly shorter when pacing from the mid-septum compared with the other sites. QRS axis was significantly less vertical during mid-septal pacing (18 ± 51°) compared with para-Hissian (38 ± 37°, P = 0.028) and anterior (53 ± 55°, P = 0.003) pacing, and QRS transition was intermediate (4.8 ± 1.3 vs. 3.8 ± 1.3, P < 0.001, and vs. 5.4 ± 0.9, P = 0.045, respectively), although no cut-offs could reliably distinguish sites. A negative QRS or the presence of a q-wave in lead I tended to be more frequent with anterior than with mid-septal pacing (9/31 vs. 3/31, P = 0.2 and 8/31 vs. 1/31, P = 1.0, respectively).
No single ECG criterion could reliably distinguish pacing the mid-septum from the anterior wall. In particular, a negative QRS complex in lead I is an inaccurate criterion for validating septal pacing.
Introduction
For decades, ventricular pacing has been performed from the apex of the right ventricle (RV), because of ease of implantation and lead stability at this site. Conventional RV apical pacing, because of dyssynchronous left ventricular contraction, may have detrimental effects on cardiac structure and pump function.1,2 Randomized trials have reported that RV apical pacing increases incidence of heart failure and atrial fibrillation.3,4 These observations have led to an interest in alternative right ventricular pacing sites,5 such as the right ventricular outflow tract (RVOT) and the mid-septum, to promote more physiological ventricular activation. However, targeting the septum may be technically challenging as it is mainly based on fluoroscopy, without reliable landmarks in patients with variable chamber size and cardiac orientation. In the single study validating lead position using echocardiography, Ng et al.6 showed that despite using oblique fluoroscopic views for placing the lead on the septum, the final position was heterogeneous, with the lead being sometimes positioned on the anterior free wall or in the anterior outflow tract. This is most probably due to tendency of the lead to fall forward as it is withdrawn from the pulmonary artery during implantation with a standard manually curved stylet. Pacing from an anterior site should be avoided as it may result in adverse effects such as reduced left ventricular systolic function6 or cardiac tamponnade,7 and may also carry a risk of damage to the left anterior descending artery.8
Surface electrocardiogram (ECG) criteria of the paced QRS complex (e.g. a negative QRS complex in lead I) have been proposed to confirm an RVOT septal position.5,9–11 However, the ECG criteria in these studies have not been properly validated, as actual lead position was not confirmed by any imaging technique other than per-procedural fluoroscopy or a simple chest X-ray. Also, it is unknown whether these criteria apply to a mid-septal pacing site, which is lower and more rightward than the RVOT septum.
The aim of our study was to identify ECG criteria during RV pacing that confirm a mid-septal position and differentiate this site from the anterior free wall, using electroanatomical mapping to validate pacing sites.
Methods
Patient population
A total of 31 consecutive patients from two centres in Geneva (University Hospital and La Tour Hospital), who were scheduled to undergo radiofrequency ablation of isthmus-dependent atrial flutter, were prospectively enrolled in the study. Patient demographics are shown in Table 1.
| . | All patients (n = 31) . |
|---|---|
| Age (years) | 70 ± 11 |
| Male/Female | 26/5 |
| Underlying heart disease | |
| Ischaemic | 9 |
| Dilated cardiomyopathy | 2 |
| Significant valve dysfunction | 4 |
| None | 16 |
| LVEF (%) | 52 ± 4 |
| Intrinsic QRS (ms) | 108 ± 22 |
| . | All patients (n = 31) . |
|---|---|
| Age (years) | 70 ± 11 |
| Male/Female | 26/5 |
| Underlying heart disease | |
| Ischaemic | 9 |
| Dilated cardiomyopathy | 2 |
| Significant valve dysfunction | 4 |
| None | 16 |
| LVEF (%) | 52 ± 4 |
| Intrinsic QRS (ms) | 108 ± 22 |
LVEF, left ventricular ejection fraction. Data expressed as mean ± SD.
| . | All patients (n = 31) . |
|---|---|
| Age (years) | 70 ± 11 |
| Male/Female | 26/5 |
| Underlying heart disease | |
| Ischaemic | 9 |
| Dilated cardiomyopathy | 2 |
| Significant valve dysfunction | 4 |
| None | 16 |
| LVEF (%) | 52 ± 4 |
| Intrinsic QRS (ms) | 108 ± 22 |
| . | All patients (n = 31) . |
|---|---|
| Age (years) | 70 ± 11 |
| Male/Female | 26/5 |
| Underlying heart disease | |
| Ischaemic | 9 |
| Dilated cardiomyopathy | 2 |
| Significant valve dysfunction | 4 |
| None | 16 |
| LVEF (%) | 52 ± 4 |
| Intrinsic QRS (ms) | 108 ± 22 |
LVEF, left ventricular ejection fraction. Data expressed as mean ± SD.
All patients gave informed consent to participate in the study, which was approved by the Institutional Ethics Committee.
Mapping protocol
Patients were studied in a fasting and sedated state. Two catheters were introduced percutaneously through the right femoral vein. A 6-French quadripolar diagnostic catheter (Bard Electrophysiology, Lowell, MA, USA) was advanced to the right atrium and an irrigated-tip 3.5 mm ablation catheter (ThermoCool F curve, Biosense Webster, Diamond Bar, CA, USA or Therapy Cool Path FL curve, St Jude Medical, St Paul, MN, USA) was used for performing cavo-tricuspid isthmus ablation. After obtaining bidirectional block of the cavo-tricuspid isthmus, anatomical reconstruction of the RV was performed using the EnSite NavX® system (St Jude Medical). The quadripolar diagnostic catheter was used as the reference and positioned in a stable position in the right atrium (rather than in the ventricle, so as to avoid displacement when manipulating the mapping catheter), with creation of a ‘shadow’ to monitor displacement. The ablation catheter was manoeuvred in the entire RV for geometrical reconstruction. The plane of the pulmonary valve was defined by advancing the mapping catheter in the RVOT until no discrete bipolar electrograms were recorded in the distal electrode, and the tricuspid valve was defined by equal amplitudes of atrial and ventricular electrograms. The His bundle was annotated at the onset of mapping, and its location checked at the end of the pacing protocol, in order to verify the absence of reference shift during the study (in addition to verifying the shadow of the quadripolar reference catheter).
After geometrical reconstruction of the RV, pace-mapping of three sites was performed (Figure 1): para-Hissian (about 1 cm into the ventricle from the His), the mid-septum (at the centre of the septum in the right oblique anterior view, roughly halfway along the line drawn between the His and the apex, and caudal to the level of the His), and the RV anterior free wall (close to the anteroseptal sulcus, where pacing leads are often inadvertently placed). Anatomical tagging was performed at each site and the ventricle was paced at 80 bpm for 10–20 captured beats, during which a 12-lead digital ECG was continuously recorded using the Bard® electrophysiology bay (Figure 2).
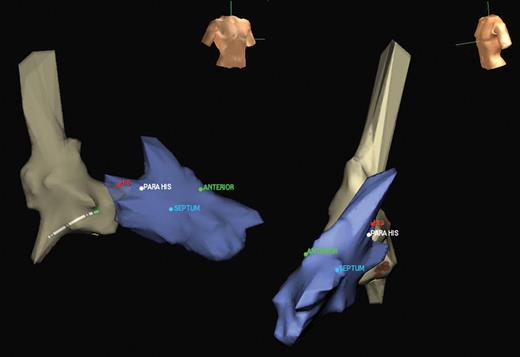
Illustration of anatomical reconstruction of the right ventricle (shown here with the right atrium) and tagging of pacing sites (para-Hissian, mid-septal, and anterior).
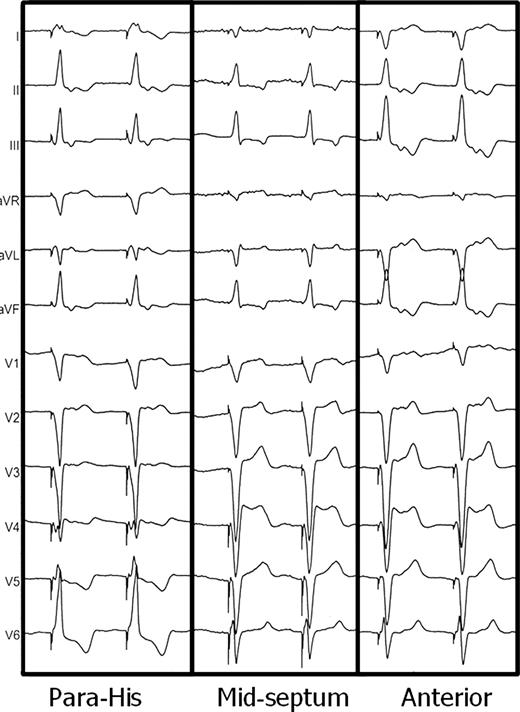
Example of QRS morphology from different pacing sites. Note greater negativity in lead I when pacing from the anterior free wall compared with from the mid-septum.
Electrocardiogram analysis
The 12-lead ECG derived from each pacing site was analysed off-line using the digital callipers of the Bard® electrophysiology bay. The following parameters were analysed: The measurements were performed by a single observer (C.-I.P.) and verified by a second investigator (H.B.).
QRS duration
Amplitudes of Q, R, and S waves in all limb leads. The net QRS amplitude in each lead was calculated as R−(Q + S), and was used to define whether the QRS was positive or negative in that lead, and for calculation of the QRS axis.
QRS axis calculated using net QRS amplitudes in leads I and aVF with the following formula that we conceived: axis = 57.3*ATAN(AVF/I). The value was manually adjusted for axes of +90° or −90° in case of a perfectly isoelectric QRS complex in lead I (as the formula yields an error for lead I = 0), and corrected by adding 180° to the result if the QRS was negative in lead I. A visually estimated QRS axis was also noted to serve as a control.
Presence of a q-wave or a negative QRS in lead I (which has previously been attributed to septal pacing9,12)
Presence of QRS notching in the limb leads (pacing of free wall sites has been reported to result in notching in the inferior leads9,12)
QRS transition in the precordial leads (a transition at or later than V4 has been shown to distinguish RVOT free wall sites from an RVOT septal site12). Transition was defined as the lead with R > (Q + S) amplitude.
Statistical analysis
Statistical analyses were performed using SPSS software (SPSS, Inc., Chicago, IL, USA). Continuous data were analysed using paired Student's t-tests. Fisher's exact test was used for evaluating dichotomous variables. Bland–Altmann analysis was performed to evaluate agreement between calculated and visually estimated QRS axes. Continuous values are expressed as mean ± SD. A P-value of <0.05 was considered statistically significant.
Results
The results are shown in Table 2, with yields of dichotomous parameters for distinguishing a mid-septal from an anterior pacing site shown in Table 3.
Results of the electrocardiogram parameters from different patient sites in the 31 patients
| Pacing site . | QRS duration (ms) . | QRS axis (°) . | Negative QRS in DI, n (%) . | q in DI, n (%) . | Notch one or more inferior leads, n (%) . | Notch in DI, n (%) . | QRS transition (V lead) . |
|---|---|---|---|---|---|---|---|
| Para-Hissian | 145 ± 23** | 38 ± 37* | 1 (3) | 0 (0) | 6 (19) | 4 (13) | 3.8 ± 1.3** |
| Mid-septum | 157 ± 26 | 18 ± 51 | 3 (10) | 1 (3) | 7 (23) | 9 (29) | 4.8 ± 1.3 |
| Anterior | 155 ± 22 | 53 ± 55* | 9 (29) | 8 (26) | 2 (6)* | 6 (19)* | 5.4 ± 0.9* |
| Pacing site . | QRS duration (ms) . | QRS axis (°) . | Negative QRS in DI, n (%) . | q in DI, n (%) . | Notch one or more inferior leads, n (%) . | Notch in DI, n (%) . | QRS transition (V lead) . |
|---|---|---|---|---|---|---|---|
| Para-Hissian | 145 ± 23** | 38 ± 37* | 1 (3) | 0 (0) | 6 (19) | 4 (13) | 3.8 ± 1.3** |
| Mid-septum | 157 ± 26 | 18 ± 51 | 3 (10) | 1 (3) | 7 (23) | 9 (29) | 4.8 ± 1.3 |
| Anterior | 155 ± 22 | 53 ± 55* | 9 (29) | 8 (26) | 2 (6)* | 6 (19)* | 5.4 ± 0.9* |
*P < 0.05 compared with mid-septum.
**P ≤ 0.001 compared with mid-septum.
Results of the electrocardiogram parameters from different patient sites in the 31 patients
| Pacing site . | QRS duration (ms) . | QRS axis (°) . | Negative QRS in DI, n (%) . | q in DI, n (%) . | Notch one or more inferior leads, n (%) . | Notch in DI, n (%) . | QRS transition (V lead) . |
|---|---|---|---|---|---|---|---|
| Para-Hissian | 145 ± 23** | 38 ± 37* | 1 (3) | 0 (0) | 6 (19) | 4 (13) | 3.8 ± 1.3** |
| Mid-septum | 157 ± 26 | 18 ± 51 | 3 (10) | 1 (3) | 7 (23) | 9 (29) | 4.8 ± 1.3 |
| Anterior | 155 ± 22 | 53 ± 55* | 9 (29) | 8 (26) | 2 (6)* | 6 (19)* | 5.4 ± 0.9* |
| Pacing site . | QRS duration (ms) . | QRS axis (°) . | Negative QRS in DI, n (%) . | q in DI, n (%) . | Notch one or more inferior leads, n (%) . | Notch in DI, n (%) . | QRS transition (V lead) . |
|---|---|---|---|---|---|---|---|
| Para-Hissian | 145 ± 23** | 38 ± 37* | 1 (3) | 0 (0) | 6 (19) | 4 (13) | 3.8 ± 1.3** |
| Mid-septum | 157 ± 26 | 18 ± 51 | 3 (10) | 1 (3) | 7 (23) | 9 (29) | 4.8 ± 1.3 |
| Anterior | 155 ± 22 | 53 ± 55* | 9 (29) | 8 (26) | 2 (6)* | 6 (19)* | 5.4 ± 0.9* |
*P < 0.05 compared with mid-septum.
**P ≤ 0.001 compared with mid-septum.
Diagnostic yield of different electrocardiogram criteria for distinguishing pacing of the mid-septum from the anterior free wall
| . | Sensitivity . | Specificity . | PPV . | NPV . | Accuracy . |
|---|---|---|---|---|---|
| Negative QRS in DI | 0.10 | 0.71 | 0.25 | 0.44 | 0.40 |
| q in DI | 0.03 | 0.74 | 0.11 | 0.43 | 0.39 |
| Notching in DI | 0.29 | 0.81 | 0.60 | 0.53 | 0.55 |
| Notching in one or more inferior leads | 0.23 | 0.94 | 0.78 | 0.55 | 0.58 |
| . | Sensitivity . | Specificity . | PPV . | NPV . | Accuracy . |
|---|---|---|---|---|---|
| Negative QRS in DI | 0.10 | 0.71 | 0.25 | 0.44 | 0.40 |
| q in DI | 0.03 | 0.74 | 0.11 | 0.43 | 0.39 |
| Notching in DI | 0.29 | 0.81 | 0.60 | 0.53 | 0.55 |
| Notching in one or more inferior leads | 0.23 | 0.94 | 0.78 | 0.55 | 0.58 |
PPV, positive predictive value; NPV, negative predictive value; Accuracy refers to: (number of true positives + number of true negatives)/total.
Diagnostic yield of different electrocardiogram criteria for distinguishing pacing of the mid-septum from the anterior free wall
| . | Sensitivity . | Specificity . | PPV . | NPV . | Accuracy . |
|---|---|---|---|---|---|
| Negative QRS in DI | 0.10 | 0.71 | 0.25 | 0.44 | 0.40 |
| q in DI | 0.03 | 0.74 | 0.11 | 0.43 | 0.39 |
| Notching in DI | 0.29 | 0.81 | 0.60 | 0.53 | 0.55 |
| Notching in one or more inferior leads | 0.23 | 0.94 | 0.78 | 0.55 | 0.58 |
| . | Sensitivity . | Specificity . | PPV . | NPV . | Accuracy . |
|---|---|---|---|---|---|
| Negative QRS in DI | 0.10 | 0.71 | 0.25 | 0.44 | 0.40 |
| q in DI | 0.03 | 0.74 | 0.11 | 0.43 | 0.39 |
| Notching in DI | 0.29 | 0.81 | 0.60 | 0.53 | 0.55 |
| Notching in one or more inferior leads | 0.23 | 0.94 | 0.78 | 0.55 | 0.58 |
PPV, positive predictive value; NPV, negative predictive value; Accuracy refers to: (number of true positives + number of true negatives)/total.
QRS duration
The paced QRS duration was significantly longer than during intrinsic rhythm for all sites (P < 0.001 for all comparisons). Pacing from the para-Hissian site yielded shorter QRS duration than from both other sites (P = 0.001).
QRS axis
Even though mid-septal pacing yielded a significantly more leftward calculated axis compared with pacing from the para-Hissian or anterior sites (P = 0.028 and P = 0.003, respectively), values were very variable, ranging from −60° to 117°, and no single cut-off was able to accurately differentiate pacing sites. The 95% limits of agreement between visually estimated and calculated QRS axes were −21° to 26°.
QRS transition
Pacing from the mid-septum yielded QRS transition that was intermediate between pacing from para-Hissian and anterior sites (P < 0.001 and P = 0.045, respectively). However, QRS transition with mid-septal pacing was very variable and no cut-off could accurately distinguish this site from the others. QRS transition at >V4 was present in 21/31 (68%) cases during para-Hissian pacing in 29/31 (94%) of cases during mid-septal pacing (P = 1.0), and in all cases during anterior pacing.
Negative QRS or q-wave in lead I
There were no differences in prevalence of these parameters between groups (P ≥ 0.2 for all comparisons), although a negative QRS complex or the presence of a q-wave in lead I tended to be more frequent with pacing from an anterior site than from the mid-septum.
Notching of the QRS complex in limb leads
We analysed QRS notching in lead I or in any inferior lead. QRS notching was marginally more frequent when pacing from the mid-septum compared with from an anterior site, in lead I or in any inferior lead (P = 0.043 and P = 0.045, respectively).
Discussion
Several studies have evaluated the RVOT or the mid-septum as alternative pacing sites, but results remain unequivocal in terms of benefit compared with apical pacing.13 The discrepancy in findings may in part be explained by heterogeneity of lead position in these studies, and due to the fact that the target position was not confirmed by imaging modalities other than intra-operative fluoroscopy or plain radiography. As previously mentioned, the final lead position may be heterogeneous despite use of oblique fluoroscopic views, with the lead being sometimes positioned on the anterior free wall or in the anterior outflow tract when confirmed by transthoracic echocardiography, instead of on the true septum.6
In order to confirm RVOT septal lead placement, a negative paced QRS complex in lead I, has been proposed.5,9–11 However, evaluation of this criterion for pacing has never been adequately performed. Some studies have used electroanatomical mapping for validating ECG criteria to localize RVOT tachycardia that may serve as a surrogate for RVOT pacing. Dixit et al.12 studied 14 patients using detailed CARTO electroanatomical mapping of the RVOT. The authors found that a negative QRS complex in lead I was observed when pacing from the RVOT anterior free wall or the RVOT anterior septum, whereas the QRS complex was positive or isoelectric when pacing from other RVOT septal sites. In another study, in 52 patients studied using NavX, Zhang et al.14 reported that a QS complex in lead I indicated an anterior site. These studies confirm findings from older reports that used only fluoroscopy for validating RVOT pacing sites.15,16 Our study evaluated for the first time, using electroanatomical mapping, the criterion for mid-septal pacing. A negative QRS complex or the presence of a q-wave in lead I tended to be more frequent when pacing from the anterior wall compared with from the mid-septum (similar to what was reported for the RVOT12,14–16). This may be explained by a more leftward position of the anterior pacing site due to the orientation of the heart, as well as a rightward bulging of the mid-septum. In contrast to the study by Dixit et al.,12 notching of the QRS complex was more frequent when pacing from the septum than from the free wall, possibly due to differences in the myocardial architecture of the RVOT compared with the mid-septum, or perhaps due to a certain degree of subjectivity when defining notching. Narrowing of the QRS complex has also been used previously to map the interventricular septum for pacing.17 However, we found no significant differences in QRS width when pacing from the mid-septum or from the anterior free wall. Indeed, narrowing of the QRS complex, possibly due to capture of the conduction system, was only seen during para-Hissian pacing in our study.
Attaining a true septal lead position for pacemaker implantation is technically challenging. It may require a combination of operator experience, fluoroscopic landmarks in multiple views (that are still limited by anatomical variations), and tools such as modified stylet shapes18 or leads delivered by deflectable catheters such as the Medtronic (Minneapolis, MN, USA) Select Secure system. Randomized trials using Select Secure leads are currently in progress and are evaluating whether the mid-septum or the inflow septum offers advantages over the right ventricular apex, but validation of the final lead position will probably remain an issue in these trials.19
Study limitations
The mid-septum is a relatively large area, and ECG characteristics may have varied according to different septal positions. Bipolar pacing may have led to anodal capture. However, narrow inter-electrode spacing means that this is unlikely to have had a significant impact on ECG morphology. We did not study RVOT sites, as these have been previously studied in detail using electroanatomical mapping.12,14
Conclusions
No single ECG criterion can reliably confirm pacing of the mid-septum and distinguish this site from the anterior free wall, probably due to variations in patient anatomy. In particular, there is a generally held misconception that a negative QRS complex in lead I may confirm septal pacing, and this criterion should no longer be used.
Funding
H.B. was funded in part by a grant from the Fondation de Recherche de l'Hôpital de la Tour. C.S. is funded by a research grant from Medtronic, Switzerland.
Acknowledgements
We wish to thank St Jude Medical (Switzerland) for having lent the Ensite NavX system to the University Hospital of Geneva for the duration of the study. We also wish to thank Eric Lambert, MD and Laurence Rassaby, PhD (both employees of St Jude Medical, Switzerland) for their technical assistance.
Conflict of interest: none declared.



