-
PDF
- Split View
-
Views
-
Cite
Cite
Satoshi Yanagisawa, Ken Miki, Nobuyuki Yasuda, Toshihisa Hirai, Noriyuki Suzuki, Toshikazu Tanaka, The prognostic value of treadmill exercise testing in very elderly patients: heart rate recovery as a predictor of mortality in octogenarians, EP Europace, Volume 13, Issue 1, January 2011, Pages 114–120, https://doi.org/10.1093/europace/euq422
Close - Share Icon Share
Abstract
Several treadmill exercise testing prognostic parameters have been identified in various populations. However, despite the widespread use of treadmill exercise testing, the prognostic value in very elderly patients has not been well characterized. The aim of this study was to assess the results of treadmill exercise testing in octogenarians, and to examine various parameters in order to identify a prognostic marker of mortality.
This study included 97 consecutive octogenarians (age, 81.1 ± 1.8 years; 66% male) who were referred for treadmill exercise testing. During the follow-up period (2.6 ± 1.6 years), all-cause death occurred in 20 patients (21%). Univariate Cox proportional hazard regression analysis showed that abnormal heart rate recovery (HRR) (defined as a decreased heart rate of ≤18 beats per minute after peak exercise) [hazard ratio (HR), 2.82; 95% confidence interval (CI), 1.06–7.47; P = 0.037] and ischaemic ST-segment change (HR, 2.56; 95% CI, 1.01–6.46; P = 0.047) were significantly associated with all-cause mortality. After adjusting for age and sex, multivariate Cox proportional hazard analysis showed that abnormal HRR was the only independent predictor of all-cause death (HR, 2.86; 95% CI, 1.01–8.11; P = 0.048).
Attenuated HRR is a significant prognostic marker for all-cause death among octogenarians. The results may provide helpful support for risk stratification in clinical practice.
Introduction
Cardiovascular disease is a common condition affecting elderly patients because these patients have a greater risk of arteriosclerosis. The proportion of elderly patients enrolling for medical examinations is relatively high. To ensure primary prevention and avoid adverse outcomes, it is important to detect cardiovascular disease at an early stage. Among several examinations, including echocardiography and nuclear imaging, that have been established for risk stratifying in routine practice, the treadmill exercise test has historically been considered as a potentially useful modality for coronary disease during the first stage of screening.1 It is simple to administer, inexpensive, and safe. Although the sensitivity and specificity have been reported to be variable, ST-segment change in electrocardiogram leads are the most common manifestations of exercise-induced myocardial ischaemia. Moreover, there have been several studies that have focused on other parameters for their prognostic value in the exercise test. Chronotropic incompetence, abnormal heart rate recovery (HRR), and delayed systolic blood pressure (SBP) response have variously been demonstrated to be useful prognostic parameters.2–5
However, it is surprising that few reports have discussed the applicability of the exercise test for the elderly population. Goroya et al.6 reported that exercise capacity is a predictor of mortality and cardiovascular events, but that ST-segment change was found to be a non-significant predictor in elderly patients. Another study found that poor exercise capacity and a decreased HRR were independently associated with mortality in subgroups distinguished as young–old adults and oldest adults.7 These studies focused mostly on elderly patients over 65 years of age. We sometimes get the opportunity to evaluate the utility of the treadmill test examination in very elderly patients, particularly those over 80 years of age; however, the applicability of the exercise test in this population is unclear. Despite ageing society and widespread use of treadmill exercise testing, the prognostic value in very elderly patients has not been well characterized. Thus, we conducted the present study to assess the results of treadmill exercise testing in octogenarians, and to identify a prognostic marker of mortality by examining various parameters from the exercise test.
Methods
Study population
We retrospectively reviewed consecutive patients aged 80 years or over who were referred to our institution for the treadmill exercise test during the period from January 2004 to December 2008. All the patients were candidates for the evaluation of suspected or known heart disease and risk stratification. Patients were excluded if they had previously had an implanted pacemaker or a history of left bundle-branch block. We also excluded those patients with symptoms of heart failure (New York Heart Association III–IV) and atrial fibrillation. The study protocol was approved by our institutional review board.
Data collection
Clinical records, including cardiovascular risk factors, medical history, comorbidities, demographic data, and previous cardiac procedures, were retrospectively reviewed. Patients were defined as having a prior coronary artery disease if they had a history of myocardial infarction, angiographically documented angina pectoris, or a history of coronary artery bypass grafting. Left ventricular function was evaluated by transthoracic echocardiography, and the left ventricular ejection fraction was calculated using the M-mode Teichholz method or the area–length method.
Exercise testing
Symptom-limited treadmill exercise testing (with a modified Bruce protocol) was performed according to the standard method.8 The exercise test was terminated if patients could achieve up to 85% of the maximum predicted heart rate or if they experienced limiting symptoms that prevented them from continuing the exercise.9 Target heart rate was defined as 85% of the age-predicted heart rate as assessed by the equation: 220 − age. After the peak workload, the exercise testing was stopped and the patients were asked to immediately lie down on a bed. There was no cool-down period in which patients are typically asked to walk slowly after peak exercise. The patients remained in the supine position for at least 3 min. If their symptoms and electrographic change persisted, the resting period was prolonged. Vital signs were monitored continuously throughout the examination.
An ischaemic ST-segment response was defined as horizontal or a down-sloping ST-segment depression of >1 mm occurring 80 ms after the J point. For the evaluation of functional capacity, metabolic equivalents (METs) were estimated (1 MET = 3.5 mL/kg per min of oxygen consumption) on the basis of the protocol and the total time elapsed in the final stage.10 Heart rate recovery is defined as the difference between the heart rate at peak exercise and that at 1 min after exercise. The cut-off value for abnormal HRR was considered to be ≤18beats/min, which is consistent with that found in most previous studies performed under similar conditions.11,12 The chronotropic response was evaluated as the percentage of heart rate reserve at peak exercise, and failure to reach 80% was defined as an impaired chronotropic response.3 Impaired functional capacity was expressed in terms of the peak exercise workload for each sex, and the specific values were 4.0 METs or less for men and 3.2 METs or less for women.7 A delay in the decline in SBP after exercise was expressed as the ratio of SBP at 3 min to SBP at 1 min after peak exercise—a ratio of more than >1.0 was considered to be abnormal.5 The cut-off for defining high resting heart rate was 79beats/min.13 Administration of beta-blockers, calcium channel antagonists, and other antiarrhythmic medications was continued during the study.
Prognosis
All-cause mortality was evaluated during the follow-up period. The causes of death and related factors were ascertained by reviewing the hospital and medical records.
Statistical analysis
Continuous variables were expressed as means ± standard deviation, and categorical variables as numbers and proportions. Continuous variables were compared between groups using Student's t-test. Categorical variables were compared using the χ2 test or Fisher's exact test. The prognostic value of each factor was first evaluated by univariate Cox proportional-hazard regression analysis. The factors with P-values of <0.10 in the univariate analysis were entered into a multivariate Cox proportional-hazard model using a forward stepwise method to identify the independent predictors for all-cause mortality. The proportional-hazards assumption was confirmed by inspecting the log [−log (survival function) curves]. To determine the correlation between two variables, we used the Pearson correlation coefficient. The association of predictor with mortality was assessed by the Kaplan–Meier method, and differences between the curves were compared using log-rank analysis. A P-value of <0.05 was considered statistically significant.
Results
A total of 97 patients (66% men) who met the inclusion criteria were included in the study. The baseline characteristics and exercise results in this cohort are summarized in Table 1. The mean age of the cohort was 81.1 ± 1.8 years. Fifty-nine patients had prior coronary artery disease, and the details of angina pectoris, myocardial infarction, and coronary artery bypass grafting were recorded for 36, 23, and 10 patients, respectively. Three patients had a history of heart failure, and the mean ejection fraction determined using echocardiography was 63.1 ± 8.4%. Calcium channel antagonists were administered to half of these patients, whereas few patients received beta-blockers. Four patients had previously undergone systematic cardiac rehabilitation. On exercise testing, mean METs was estimated as 7.3 ± 2.4, and nine patients had impaired functional capacity. Ischaemic ST-segment change was observed in 14 patients. Chronotropic incompetence, abnormal HRR, and delayed SBP response were found in 47, 35, and 37 patients, respectively. There were no complications during the exercise protocol in this study.
| Number of patients | 97 |
| Baseline characteristics | |
| Age, years | 81.1 ± 1.8 |
| Male sex | 64 (66%) |
| BMI, kg/m2 | 22.1 ± 3.1 |
| Present smoking | 20 (21%) |
| Hypertension | 47 (48%) |
| Diabetes | 31 (32%) |
| Hyperlipidaemia | 22 (23%) |
| Prior coronary artery disease | 59 (61%) |
| Angina pectoris | 36 (37%) |
| Myocardial infarction | 23 (24%) |
| CABG | 10 (10%) |
| History of heart failure | 3 (3%) |
| Medication | |
| Aspirin | 62 (64%) |
| Statin | 45 (46%) |
| ACEI/ARB | 28 (29%) |
| Beta-blocker use | 5 (5%) |
| Ca blocker use | 50 (52%) |
| LVEF, % | 63.1 ± 8.4 |
| LVEF <50% | 9 (9%) |
| Exercise results | |
| Exercise time, min | 4.9 ± 2.0 |
| Metabolic equivalents, METs | 7.3 ± 2.4 |
| SBP at rest, mmHg | 150.3 ± 22.7 |
| SBP at rest >140 mmHg | 69 (71%) |
| Heart rate at rest, beats/min | 70.5 ± 11.7 |
| Heart rate at rest >79beats/min | 21 (22%) |
| Peak SBP, mmHg | 187.7 ± 29.4 |
| Peak heart rate, beats/min | 125.6 ± 19.0 |
| Ischaemic ST-segment changes | 14 (14%) |
| Chronotropic incompetence | 47 (48%) |
| HRR, beats/min | 22.3 ± 10.6 |
| Abnormal HRR | 35 (36%) |
| Delayed SBP response | 37 (38%) |
| Impaired functional capacity | 9 (9%) |
| Reached target heart rate | 62 (64%) |
| Number of patients | 97 |
| Baseline characteristics | |
| Age, years | 81.1 ± 1.8 |
| Male sex | 64 (66%) |
| BMI, kg/m2 | 22.1 ± 3.1 |
| Present smoking | 20 (21%) |
| Hypertension | 47 (48%) |
| Diabetes | 31 (32%) |
| Hyperlipidaemia | 22 (23%) |
| Prior coronary artery disease | 59 (61%) |
| Angina pectoris | 36 (37%) |
| Myocardial infarction | 23 (24%) |
| CABG | 10 (10%) |
| History of heart failure | 3 (3%) |
| Medication | |
| Aspirin | 62 (64%) |
| Statin | 45 (46%) |
| ACEI/ARB | 28 (29%) |
| Beta-blocker use | 5 (5%) |
| Ca blocker use | 50 (52%) |
| LVEF, % | 63.1 ± 8.4 |
| LVEF <50% | 9 (9%) |
| Exercise results | |
| Exercise time, min | 4.9 ± 2.0 |
| Metabolic equivalents, METs | 7.3 ± 2.4 |
| SBP at rest, mmHg | 150.3 ± 22.7 |
| SBP at rest >140 mmHg | 69 (71%) |
| Heart rate at rest, beats/min | 70.5 ± 11.7 |
| Heart rate at rest >79beats/min | 21 (22%) |
| Peak SBP, mmHg | 187.7 ± 29.4 |
| Peak heart rate, beats/min | 125.6 ± 19.0 |
| Ischaemic ST-segment changes | 14 (14%) |
| Chronotropic incompetence | 47 (48%) |
| HRR, beats/min | 22.3 ± 10.6 |
| Abnormal HRR | 35 (36%) |
| Delayed SBP response | 37 (38%) |
| Impaired functional capacity | 9 (9%) |
| Reached target heart rate | 62 (64%) |
Continuous variable are shown as mean ± SD, and categorical variables are shown as number (%). BMI, body mass index; CABG, coronary artery bypass grafting; ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin-receptor blockers; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure; HRR, heart rate recovery.
| Number of patients | 97 |
| Baseline characteristics | |
| Age, years | 81.1 ± 1.8 |
| Male sex | 64 (66%) |
| BMI, kg/m2 | 22.1 ± 3.1 |
| Present smoking | 20 (21%) |
| Hypertension | 47 (48%) |
| Diabetes | 31 (32%) |
| Hyperlipidaemia | 22 (23%) |
| Prior coronary artery disease | 59 (61%) |
| Angina pectoris | 36 (37%) |
| Myocardial infarction | 23 (24%) |
| CABG | 10 (10%) |
| History of heart failure | 3 (3%) |
| Medication | |
| Aspirin | 62 (64%) |
| Statin | 45 (46%) |
| ACEI/ARB | 28 (29%) |
| Beta-blocker use | 5 (5%) |
| Ca blocker use | 50 (52%) |
| LVEF, % | 63.1 ± 8.4 |
| LVEF <50% | 9 (9%) |
| Exercise results | |
| Exercise time, min | 4.9 ± 2.0 |
| Metabolic equivalents, METs | 7.3 ± 2.4 |
| SBP at rest, mmHg | 150.3 ± 22.7 |
| SBP at rest >140 mmHg | 69 (71%) |
| Heart rate at rest, beats/min | 70.5 ± 11.7 |
| Heart rate at rest >79beats/min | 21 (22%) |
| Peak SBP, mmHg | 187.7 ± 29.4 |
| Peak heart rate, beats/min | 125.6 ± 19.0 |
| Ischaemic ST-segment changes | 14 (14%) |
| Chronotropic incompetence | 47 (48%) |
| HRR, beats/min | 22.3 ± 10.6 |
| Abnormal HRR | 35 (36%) |
| Delayed SBP response | 37 (38%) |
| Impaired functional capacity | 9 (9%) |
| Reached target heart rate | 62 (64%) |
| Number of patients | 97 |
| Baseline characteristics | |
| Age, years | 81.1 ± 1.8 |
| Male sex | 64 (66%) |
| BMI, kg/m2 | 22.1 ± 3.1 |
| Present smoking | 20 (21%) |
| Hypertension | 47 (48%) |
| Diabetes | 31 (32%) |
| Hyperlipidaemia | 22 (23%) |
| Prior coronary artery disease | 59 (61%) |
| Angina pectoris | 36 (37%) |
| Myocardial infarction | 23 (24%) |
| CABG | 10 (10%) |
| History of heart failure | 3 (3%) |
| Medication | |
| Aspirin | 62 (64%) |
| Statin | 45 (46%) |
| ACEI/ARB | 28 (29%) |
| Beta-blocker use | 5 (5%) |
| Ca blocker use | 50 (52%) |
| LVEF, % | 63.1 ± 8.4 |
| LVEF <50% | 9 (9%) |
| Exercise results | |
| Exercise time, min | 4.9 ± 2.0 |
| Metabolic equivalents, METs | 7.3 ± 2.4 |
| SBP at rest, mmHg | 150.3 ± 22.7 |
| SBP at rest >140 mmHg | 69 (71%) |
| Heart rate at rest, beats/min | 70.5 ± 11.7 |
| Heart rate at rest >79beats/min | 21 (22%) |
| Peak SBP, mmHg | 187.7 ± 29.4 |
| Peak heart rate, beats/min | 125.6 ± 19.0 |
| Ischaemic ST-segment changes | 14 (14%) |
| Chronotropic incompetence | 47 (48%) |
| HRR, beats/min | 22.3 ± 10.6 |
| Abnormal HRR | 35 (36%) |
| Delayed SBP response | 37 (38%) |
| Impaired functional capacity | 9 (9%) |
| Reached target heart rate | 62 (64%) |
Continuous variable are shown as mean ± SD, and categorical variables are shown as number (%). BMI, body mass index; CABG, coronary artery bypass grafting; ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin-receptor blockers; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure; HRR, heart rate recovery.
During the follow-up period (2.6 ± 1.6 years), 20 deaths (21%) occurred and the causes of death were cancer (13 patients), stroke (3 patients), pneumonia (2 patients), and major aortic disease (2 patients). Follow-up data were obtained for 1 year in the case of 86 patients (89%) and for 2 years in the case of 70 patients (72%), and the mortality rates over the 1 and 2 year periods were 4.6 and 11.4%, respectively. Univariate Cox proportional-hazard regression analysis showed that abnormal HRR [hazard ratio (HR), 2.82; 95% confidence interval (CI), 1.06–7.47; P = 0.037] and ischaemic ST-segment change (HR, 2.56; 95% CI, 1.01–6.46; P = 0.047) were significantly associated with all-cause mortality (Table 2). Multivariate analysis showed that abnormal HRR was the only independent predictor of all-cause death (HR, 2.86; 95% CI, 1.01–8.11; P = 0.048) after adjusting for age and sex. The patients were divided into two groups on the basis of their HRR, namely, normal HRR and abnormal HRR groups. The baseline characteristics and exercise results grouped according to HRR are presented in Table 3. The patients with abnormal HRR were more likely to be older than those with normal HRR and were also likely to have a higher resting heart rate, and lower peak heart rate, exercise time, peak systolic pressure, and METs. In addition, chronotropic incompetence, ischaemic ST-segment changes, impaired functional capacity, delayed SBP response, and failure to achieve the target heart rate were significantly more frequent in the abnormal HRR group than in the normal HRR group. With regard to prognosis, the patients with abnormal HRR had higher mortality than those with normal HRR (40 vs. 10%, P = 0.001). We also compared using event-free Kaplan–Meier curves for all-cause death, and confirmed that patients with abnormal HRR had significantly decreased event-free survival compared with those patients with normal HRR for all-cause death (P = 0.03; Figure 1).
| Variable . | Rates or mean value . | Hazard ratio (95% CI) . | P-value . | |
|---|---|---|---|---|
| . | Non survival (n = 20) . | Survival (n = 77) . | . | . |
| Age, years | 81.5 ± 2.4 | 81.0 ± 1.6 | 1.11 (0.89–1.39) | 0.345 |
| Male sex | 70% | 65% | 1.35 (0.52–3.54) | 0.536 |
| BMI, kg/m2 | 21.8 ± 3.8 | 22.2 ± 2.9 | 0.90 (0.77–1.05) | 0.184 |
| Hypertension | 45% | 49% | 0.50 (0.20–1.24) | 0.136 |
| Diabetes | 25% | 34% | 0.45 (0.16–1.25) | 0.127 |
| Prior coronary artery disease | 65% | 60% | 0.90 (0.36–2.26) | 0.823 |
| History of heart failure | 5% | 3% | 0.82 (0.11–6.18) | 0.845 |
| Beta blocker use | 5% | 5% | 0.63 (0.08–4.77) | 0.658 |
| Ca blocker use | 55% | 51% | 1.06 (0.44–2.57) | 0.891 |
| LVEF, % | 62.0 ± 11.2 | 63.4 ± 7.6 | 0.98 (0.94–1.03) | 0.406 |
| LVEF <50% | 20% | 6% | 2.44 (0.81–7.33) | 0.111 |
| Metabolic equivalents, METs | 7.1 ± 2.3 | 7.4 ± 2.5 | 1.00 (0.82–1.21) | 0.988 |
| SBP at rest, mmHg | 147.5 ± 24.4 | 151.0 ± 22.3 | 0.99 (0.97–1.02) | 0.546 |
| SBP at rest >140mmHg | 60% | 74% | 0.53 (0.22–1.30) | 0.163 |
| Heart rate at rest, beat/min | 73.6 ± 12.1 | 69.5 ± 11.4 | 1.01 (0.98–1.02) | 0.399 |
| Heart rate at rest >79beat/min | 40% | 17% | 1.82 (0.74–4.48) | 0.194 |
| Peak heart rate, beats/min | 124.9 ± 21.0 | 125.8 ± 18.6 | 1.00 (0.98–1.02) | 0.862 |
| Ischaemic ST-segment changes | 35% | 9% | 2.56 (1.01–6.46) | 0.047a |
| Chronotropic incompetence | 50% | 48% | 0.93 (0.39–2.24) | 0.871 |
| Abnormal HRR | 70% | 27% | 2.82 (1.06–7.47) | 0.037a |
| Delayed SBP response | 45% | 36% | 1.59 (0.65–3.88) | 0.306 |
| Impaired functional capacity | 10% | 9% | 1.04 (0.24–4.51) | 0.956 |
| Reached target heart rate | 65% | 64% | 1.24 (0.49–3.13) | 0.644 |
| Variable . | Rates or mean value . | Hazard ratio (95% CI) . | P-value . | |
|---|---|---|---|---|
| . | Non survival (n = 20) . | Survival (n = 77) . | . | . |
| Age, years | 81.5 ± 2.4 | 81.0 ± 1.6 | 1.11 (0.89–1.39) | 0.345 |
| Male sex | 70% | 65% | 1.35 (0.52–3.54) | 0.536 |
| BMI, kg/m2 | 21.8 ± 3.8 | 22.2 ± 2.9 | 0.90 (0.77–1.05) | 0.184 |
| Hypertension | 45% | 49% | 0.50 (0.20–1.24) | 0.136 |
| Diabetes | 25% | 34% | 0.45 (0.16–1.25) | 0.127 |
| Prior coronary artery disease | 65% | 60% | 0.90 (0.36–2.26) | 0.823 |
| History of heart failure | 5% | 3% | 0.82 (0.11–6.18) | 0.845 |
| Beta blocker use | 5% | 5% | 0.63 (0.08–4.77) | 0.658 |
| Ca blocker use | 55% | 51% | 1.06 (0.44–2.57) | 0.891 |
| LVEF, % | 62.0 ± 11.2 | 63.4 ± 7.6 | 0.98 (0.94–1.03) | 0.406 |
| LVEF <50% | 20% | 6% | 2.44 (0.81–7.33) | 0.111 |
| Metabolic equivalents, METs | 7.1 ± 2.3 | 7.4 ± 2.5 | 1.00 (0.82–1.21) | 0.988 |
| SBP at rest, mmHg | 147.5 ± 24.4 | 151.0 ± 22.3 | 0.99 (0.97–1.02) | 0.546 |
| SBP at rest >140mmHg | 60% | 74% | 0.53 (0.22–1.30) | 0.163 |
| Heart rate at rest, beat/min | 73.6 ± 12.1 | 69.5 ± 11.4 | 1.01 (0.98–1.02) | 0.399 |
| Heart rate at rest >79beat/min | 40% | 17% | 1.82 (0.74–4.48) | 0.194 |
| Peak heart rate, beats/min | 124.9 ± 21.0 | 125.8 ± 18.6 | 1.00 (0.98–1.02) | 0.862 |
| Ischaemic ST-segment changes | 35% | 9% | 2.56 (1.01–6.46) | 0.047a |
| Chronotropic incompetence | 50% | 48% | 0.93 (0.39–2.24) | 0.871 |
| Abnormal HRR | 70% | 27% | 2.82 (1.06–7.47) | 0.037a |
| Delayed SBP response | 45% | 36% | 1.59 (0.65–3.88) | 0.306 |
| Impaired functional capacity | 10% | 9% | 1.04 (0.24–4.51) | 0.956 |
| Reached target heart rate | 65% | 64% | 1.24 (0.49–3.13) | 0.644 |
Continuous variable are shown as mean ± SD, and categorical variables are shown as percent. CI, confidence interval; BMI, body mass index; Ca, calcium; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure; HRR, heart rate recovery.
aVariables included into multivariate models.
| Variable . | Rates or mean value . | Hazard ratio (95% CI) . | P-value . | |
|---|---|---|---|---|
| . | Non survival (n = 20) . | Survival (n = 77) . | . | . |
| Age, years | 81.5 ± 2.4 | 81.0 ± 1.6 | 1.11 (0.89–1.39) | 0.345 |
| Male sex | 70% | 65% | 1.35 (0.52–3.54) | 0.536 |
| BMI, kg/m2 | 21.8 ± 3.8 | 22.2 ± 2.9 | 0.90 (0.77–1.05) | 0.184 |
| Hypertension | 45% | 49% | 0.50 (0.20–1.24) | 0.136 |
| Diabetes | 25% | 34% | 0.45 (0.16–1.25) | 0.127 |
| Prior coronary artery disease | 65% | 60% | 0.90 (0.36–2.26) | 0.823 |
| History of heart failure | 5% | 3% | 0.82 (0.11–6.18) | 0.845 |
| Beta blocker use | 5% | 5% | 0.63 (0.08–4.77) | 0.658 |
| Ca blocker use | 55% | 51% | 1.06 (0.44–2.57) | 0.891 |
| LVEF, % | 62.0 ± 11.2 | 63.4 ± 7.6 | 0.98 (0.94–1.03) | 0.406 |
| LVEF <50% | 20% | 6% | 2.44 (0.81–7.33) | 0.111 |
| Metabolic equivalents, METs | 7.1 ± 2.3 | 7.4 ± 2.5 | 1.00 (0.82–1.21) | 0.988 |
| SBP at rest, mmHg | 147.5 ± 24.4 | 151.0 ± 22.3 | 0.99 (0.97–1.02) | 0.546 |
| SBP at rest >140mmHg | 60% | 74% | 0.53 (0.22–1.30) | 0.163 |
| Heart rate at rest, beat/min | 73.6 ± 12.1 | 69.5 ± 11.4 | 1.01 (0.98–1.02) | 0.399 |
| Heart rate at rest >79beat/min | 40% | 17% | 1.82 (0.74–4.48) | 0.194 |
| Peak heart rate, beats/min | 124.9 ± 21.0 | 125.8 ± 18.6 | 1.00 (0.98–1.02) | 0.862 |
| Ischaemic ST-segment changes | 35% | 9% | 2.56 (1.01–6.46) | 0.047a |
| Chronotropic incompetence | 50% | 48% | 0.93 (0.39–2.24) | 0.871 |
| Abnormal HRR | 70% | 27% | 2.82 (1.06–7.47) | 0.037a |
| Delayed SBP response | 45% | 36% | 1.59 (0.65–3.88) | 0.306 |
| Impaired functional capacity | 10% | 9% | 1.04 (0.24–4.51) | 0.956 |
| Reached target heart rate | 65% | 64% | 1.24 (0.49–3.13) | 0.644 |
| Variable . | Rates or mean value . | Hazard ratio (95% CI) . | P-value . | |
|---|---|---|---|---|
| . | Non survival (n = 20) . | Survival (n = 77) . | . | . |
| Age, years | 81.5 ± 2.4 | 81.0 ± 1.6 | 1.11 (0.89–1.39) | 0.345 |
| Male sex | 70% | 65% | 1.35 (0.52–3.54) | 0.536 |
| BMI, kg/m2 | 21.8 ± 3.8 | 22.2 ± 2.9 | 0.90 (0.77–1.05) | 0.184 |
| Hypertension | 45% | 49% | 0.50 (0.20–1.24) | 0.136 |
| Diabetes | 25% | 34% | 0.45 (0.16–1.25) | 0.127 |
| Prior coronary artery disease | 65% | 60% | 0.90 (0.36–2.26) | 0.823 |
| History of heart failure | 5% | 3% | 0.82 (0.11–6.18) | 0.845 |
| Beta blocker use | 5% | 5% | 0.63 (0.08–4.77) | 0.658 |
| Ca blocker use | 55% | 51% | 1.06 (0.44–2.57) | 0.891 |
| LVEF, % | 62.0 ± 11.2 | 63.4 ± 7.6 | 0.98 (0.94–1.03) | 0.406 |
| LVEF <50% | 20% | 6% | 2.44 (0.81–7.33) | 0.111 |
| Metabolic equivalents, METs | 7.1 ± 2.3 | 7.4 ± 2.5 | 1.00 (0.82–1.21) | 0.988 |
| SBP at rest, mmHg | 147.5 ± 24.4 | 151.0 ± 22.3 | 0.99 (0.97–1.02) | 0.546 |
| SBP at rest >140mmHg | 60% | 74% | 0.53 (0.22–1.30) | 0.163 |
| Heart rate at rest, beat/min | 73.6 ± 12.1 | 69.5 ± 11.4 | 1.01 (0.98–1.02) | 0.399 |
| Heart rate at rest >79beat/min | 40% | 17% | 1.82 (0.74–4.48) | 0.194 |
| Peak heart rate, beats/min | 124.9 ± 21.0 | 125.8 ± 18.6 | 1.00 (0.98–1.02) | 0.862 |
| Ischaemic ST-segment changes | 35% | 9% | 2.56 (1.01–6.46) | 0.047a |
| Chronotropic incompetence | 50% | 48% | 0.93 (0.39–2.24) | 0.871 |
| Abnormal HRR | 70% | 27% | 2.82 (1.06–7.47) | 0.037a |
| Delayed SBP response | 45% | 36% | 1.59 (0.65–3.88) | 0.306 |
| Impaired functional capacity | 10% | 9% | 1.04 (0.24–4.51) | 0.956 |
| Reached target heart rate | 65% | 64% | 1.24 (0.49–3.13) | 0.644 |
Continuous variable are shown as mean ± SD, and categorical variables are shown as percent. CI, confidence interval; BMI, body mass index; Ca, calcium; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure; HRR, heart rate recovery.
aVariables included into multivariate models.
| Variable . | Normal HRR (HRR > 18beats) . | Abnormal HRR (HRR ≤ 18 beats) . | P-value . |
|---|---|---|---|
| No. of patients | 62 | 35 | |
| Age, years | 80.7 ± 0.9 | 81.8 ± 2.5 | 0.002* |
| Male sex | 43 (69) | 21 (60) | 0.379 |
| BMI, kg/m2 | 22.2 ± 2.8 | 22.0 ± 3.6 | 0.55 |
| Present smoking | 14 (23) | 6 (17) | 0.525 |
| Hypertension | 28 (45) | 19 (54) | 0.406 |
| Diabetes | 18 (29) | 13 (37) | 0.498 |
| Hyperlipidaemia | 16 (26) | 6 (17) | 0.328 |
| Prior coronary artery disease | |||
| Angina pectoris | 26 (42) | 10 (29) | 0.274 |
| Myocardial infarction | 16 (26) | 7 (20) | 0.623 |
| CABG | 7 (11) | 3 (9) | 0.672 |
| History of heart failure | 1 (2) | 2 (6) | 0.262 |
| Medication | |||
| Beta blocker use | 3 (5) | 2 (6) | 0.851 |
| Ca blocker use | 33 (57) | 17 (49) | 0.678 |
| LVEF, % | 62.7 ± 7.8 | 63.9 ± 9.4 | 0.478 |
| LVEF <50% | 5 (8) | 4 (11) | 0.583 |
| Exercise results | |||
| Exercise time, min | 5.2 ± 1.8 | 4.3 ± 2.2 | 0.038* |
| Metabolic equivalents, METs | 7.9 ± 2.4 | 6.3 ± 2.2 | 0.001* |
| SBP at rest, mmHg | 148.7 ± 20.6 | 153.1 ± 26.0 | 0.368 |
| SBP at rest >140 mmHg | 44 (71) | 25 (71) | >0.999 |
| Heart rate at rest, beats/min | 67.7 ± 8.9 | 75.4 ± 14.3 | 0.002* |
| Heart rate at rest >79beats/min | 7 (11) | 14 (40) | 0.002* |
| Peak SBP, mmHg | 193.6 ± 30.8 | 177.2 ± 23.8 | 0.008* |
| Peak heart rate, beats/min | 130.7 ± 17.5 | 116.7 ± 23.8 | <0.001* |
| Ischaemic ST-segment changes | 3 (5) | 6 (17) | 0.001* |
| Chronotropic incompetence | 23 (37) | 24 (69) | 0.003* |
| HRR, beats/min | 28.4 ± 7.6 | 11.5 ± 5.3 | <0.001* |
| Delayed SBP response | 18 (29) | 19 (54) | 0.017* |
| Impaired functional capacity | 3 (5) | 6 (17) | 0.045* |
| Reached target heart rate | 45 (73) | 17 (49) | 0.014* |
| All-cause death | 6 (10) | 14 (40) | 0.001* |
| Variable . | Normal HRR (HRR > 18beats) . | Abnormal HRR (HRR ≤ 18 beats) . | P-value . |
|---|---|---|---|
| No. of patients | 62 | 35 | |
| Age, years | 80.7 ± 0.9 | 81.8 ± 2.5 | 0.002* |
| Male sex | 43 (69) | 21 (60) | 0.379 |
| BMI, kg/m2 | 22.2 ± 2.8 | 22.0 ± 3.6 | 0.55 |
| Present smoking | 14 (23) | 6 (17) | 0.525 |
| Hypertension | 28 (45) | 19 (54) | 0.406 |
| Diabetes | 18 (29) | 13 (37) | 0.498 |
| Hyperlipidaemia | 16 (26) | 6 (17) | 0.328 |
| Prior coronary artery disease | |||
| Angina pectoris | 26 (42) | 10 (29) | 0.274 |
| Myocardial infarction | 16 (26) | 7 (20) | 0.623 |
| CABG | 7 (11) | 3 (9) | 0.672 |
| History of heart failure | 1 (2) | 2 (6) | 0.262 |
| Medication | |||
| Beta blocker use | 3 (5) | 2 (6) | 0.851 |
| Ca blocker use | 33 (57) | 17 (49) | 0.678 |
| LVEF, % | 62.7 ± 7.8 | 63.9 ± 9.4 | 0.478 |
| LVEF <50% | 5 (8) | 4 (11) | 0.583 |
| Exercise results | |||
| Exercise time, min | 5.2 ± 1.8 | 4.3 ± 2.2 | 0.038* |
| Metabolic equivalents, METs | 7.9 ± 2.4 | 6.3 ± 2.2 | 0.001* |
| SBP at rest, mmHg | 148.7 ± 20.6 | 153.1 ± 26.0 | 0.368 |
| SBP at rest >140 mmHg | 44 (71) | 25 (71) | >0.999 |
| Heart rate at rest, beats/min | 67.7 ± 8.9 | 75.4 ± 14.3 | 0.002* |
| Heart rate at rest >79beats/min | 7 (11) | 14 (40) | 0.002* |
| Peak SBP, mmHg | 193.6 ± 30.8 | 177.2 ± 23.8 | 0.008* |
| Peak heart rate, beats/min | 130.7 ± 17.5 | 116.7 ± 23.8 | <0.001* |
| Ischaemic ST-segment changes | 3 (5) | 6 (17) | 0.001* |
| Chronotropic incompetence | 23 (37) | 24 (69) | 0.003* |
| HRR, beats/min | 28.4 ± 7.6 | 11.5 ± 5.3 | <0.001* |
| Delayed SBP response | 18 (29) | 19 (54) | 0.017* |
| Impaired functional capacity | 3 (5) | 6 (17) | 0.045* |
| Reached target heart rate | 45 (73) | 17 (49) | 0.014* |
| All-cause death | 6 (10) | 14 (40) | 0.001* |
Continuous variable are shown as mean ± SD, and categorical variables are shown as number (%). HRR, heart rate recovery; BMI, body mass index; CABG, coronary artery bypass grafting; Ca, calcium; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure.
*P < 0.05.
| Variable . | Normal HRR (HRR > 18beats) . | Abnormal HRR (HRR ≤ 18 beats) . | P-value . |
|---|---|---|---|
| No. of patients | 62 | 35 | |
| Age, years | 80.7 ± 0.9 | 81.8 ± 2.5 | 0.002* |
| Male sex | 43 (69) | 21 (60) | 0.379 |
| BMI, kg/m2 | 22.2 ± 2.8 | 22.0 ± 3.6 | 0.55 |
| Present smoking | 14 (23) | 6 (17) | 0.525 |
| Hypertension | 28 (45) | 19 (54) | 0.406 |
| Diabetes | 18 (29) | 13 (37) | 0.498 |
| Hyperlipidaemia | 16 (26) | 6 (17) | 0.328 |
| Prior coronary artery disease | |||
| Angina pectoris | 26 (42) | 10 (29) | 0.274 |
| Myocardial infarction | 16 (26) | 7 (20) | 0.623 |
| CABG | 7 (11) | 3 (9) | 0.672 |
| History of heart failure | 1 (2) | 2 (6) | 0.262 |
| Medication | |||
| Beta blocker use | 3 (5) | 2 (6) | 0.851 |
| Ca blocker use | 33 (57) | 17 (49) | 0.678 |
| LVEF, % | 62.7 ± 7.8 | 63.9 ± 9.4 | 0.478 |
| LVEF <50% | 5 (8) | 4 (11) | 0.583 |
| Exercise results | |||
| Exercise time, min | 5.2 ± 1.8 | 4.3 ± 2.2 | 0.038* |
| Metabolic equivalents, METs | 7.9 ± 2.4 | 6.3 ± 2.2 | 0.001* |
| SBP at rest, mmHg | 148.7 ± 20.6 | 153.1 ± 26.0 | 0.368 |
| SBP at rest >140 mmHg | 44 (71) | 25 (71) | >0.999 |
| Heart rate at rest, beats/min | 67.7 ± 8.9 | 75.4 ± 14.3 | 0.002* |
| Heart rate at rest >79beats/min | 7 (11) | 14 (40) | 0.002* |
| Peak SBP, mmHg | 193.6 ± 30.8 | 177.2 ± 23.8 | 0.008* |
| Peak heart rate, beats/min | 130.7 ± 17.5 | 116.7 ± 23.8 | <0.001* |
| Ischaemic ST-segment changes | 3 (5) | 6 (17) | 0.001* |
| Chronotropic incompetence | 23 (37) | 24 (69) | 0.003* |
| HRR, beats/min | 28.4 ± 7.6 | 11.5 ± 5.3 | <0.001* |
| Delayed SBP response | 18 (29) | 19 (54) | 0.017* |
| Impaired functional capacity | 3 (5) | 6 (17) | 0.045* |
| Reached target heart rate | 45 (73) | 17 (49) | 0.014* |
| All-cause death | 6 (10) | 14 (40) | 0.001* |
| Variable . | Normal HRR (HRR > 18beats) . | Abnormal HRR (HRR ≤ 18 beats) . | P-value . |
|---|---|---|---|
| No. of patients | 62 | 35 | |
| Age, years | 80.7 ± 0.9 | 81.8 ± 2.5 | 0.002* |
| Male sex | 43 (69) | 21 (60) | 0.379 |
| BMI, kg/m2 | 22.2 ± 2.8 | 22.0 ± 3.6 | 0.55 |
| Present smoking | 14 (23) | 6 (17) | 0.525 |
| Hypertension | 28 (45) | 19 (54) | 0.406 |
| Diabetes | 18 (29) | 13 (37) | 0.498 |
| Hyperlipidaemia | 16 (26) | 6 (17) | 0.328 |
| Prior coronary artery disease | |||
| Angina pectoris | 26 (42) | 10 (29) | 0.274 |
| Myocardial infarction | 16 (26) | 7 (20) | 0.623 |
| CABG | 7 (11) | 3 (9) | 0.672 |
| History of heart failure | 1 (2) | 2 (6) | 0.262 |
| Medication | |||
| Beta blocker use | 3 (5) | 2 (6) | 0.851 |
| Ca blocker use | 33 (57) | 17 (49) | 0.678 |
| LVEF, % | 62.7 ± 7.8 | 63.9 ± 9.4 | 0.478 |
| LVEF <50% | 5 (8) | 4 (11) | 0.583 |
| Exercise results | |||
| Exercise time, min | 5.2 ± 1.8 | 4.3 ± 2.2 | 0.038* |
| Metabolic equivalents, METs | 7.9 ± 2.4 | 6.3 ± 2.2 | 0.001* |
| SBP at rest, mmHg | 148.7 ± 20.6 | 153.1 ± 26.0 | 0.368 |
| SBP at rest >140 mmHg | 44 (71) | 25 (71) | >0.999 |
| Heart rate at rest, beats/min | 67.7 ± 8.9 | 75.4 ± 14.3 | 0.002* |
| Heart rate at rest >79beats/min | 7 (11) | 14 (40) | 0.002* |
| Peak SBP, mmHg | 193.6 ± 30.8 | 177.2 ± 23.8 | 0.008* |
| Peak heart rate, beats/min | 130.7 ± 17.5 | 116.7 ± 23.8 | <0.001* |
| Ischaemic ST-segment changes | 3 (5) | 6 (17) | 0.001* |
| Chronotropic incompetence | 23 (37) | 24 (69) | 0.003* |
| HRR, beats/min | 28.4 ± 7.6 | 11.5 ± 5.3 | <0.001* |
| Delayed SBP response | 18 (29) | 19 (54) | 0.017* |
| Impaired functional capacity | 3 (5) | 6 (17) | 0.045* |
| Reached target heart rate | 45 (73) | 17 (49) | 0.014* |
| All-cause death | 6 (10) | 14 (40) | 0.001* |
Continuous variable are shown as mean ± SD, and categorical variables are shown as number (%). HRR, heart rate recovery; BMI, body mass index; CABG, coronary artery bypass grafting; Ca, calcium; LVEF, left ventricular ejection fraction; SBP, systolic blood pressure.
*P < 0.05.
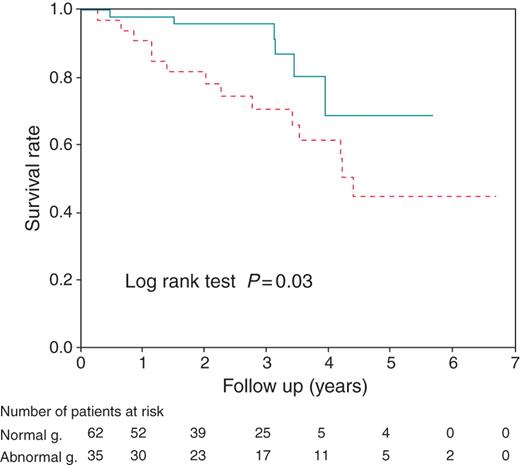
Kaplan–Meier survival curves of cumulative all-cause death survival rates in patients divided into two groups on the basis of their heart rate recovery (HRR), namely, normal and abnormal groups. Continuous line is for patients with HRR > 18beats/min, and dotted line is for patients with HRR ≤ 18beats/min.
Furthermore, we focused on the resting heart rate before exercise workload. We then evaluated the association between resting heart rate and HRR, for which we found a significant correlation (r = −0.395, P < 0.001; Figure 2). The relationship between METs and HRR categorized by survival group and non-survival group is shown in Figure 3 (r = 0.318, P = 0.002). We found that HRR was more likely to predict mortality than exercise functional capacity.
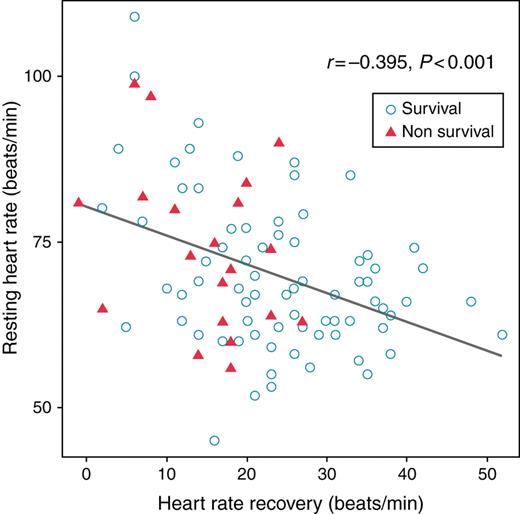
Correlation between resting heart rate and heart rate recovery (HRR) at 1 min after peak exercise.
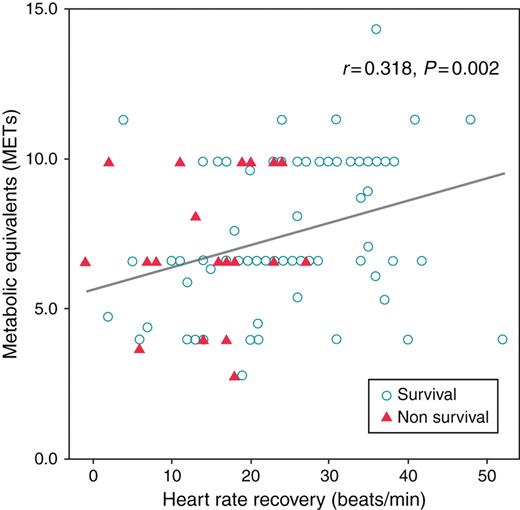
Correlation between exercise functional capacity and heart rate recovery (HRR) at 1 min after peak exercise.
Discussion
Our study demonstrated that abnormal HRR was significantly associated with all-cause death in very elderly patients undergoing the treadmill exercise test. These significant associations between HRR and prognosis persisted even after adjusting for other possible confounders.
Aging itself is associated with a decline in physical activity. Because the main workload in the treadmill test is exercise working and a symptom-limited exercise protocol is usually adopted, elderly patients are less likely to complete the exercise protocol, or to reach the target heart rate sufficiently to enable diagnosis of a negative result or to eliminate prognostic outcome with confidence. We found that 36% of octogenarian patients failed to achieve target heart rate. Contrary to our expectations, mean functional capacity presented as METs is relatively preserved comparing with the previous study of elderly patients.6 There may have been some bias in the physician's decision to refer patients for the treadmill test. In octogenarians, the suitable indication for workload stress examination might be more stringent and precautionary than in young–old patients.
Our identified predictor, abnormal HRR, which is characterized by a decrease in heart rate during the first minutes after treadmill testing, has been shown to be an important predictor of overall mortality in several populations.4,11,12 Abnormal HRR has also been reported to be significantly associated with poor prognosis in elderly patients over 65 years of age.7 Several metabolic factors contribute to HRR, and HRR immediately after peak exercise is primarily associated with vagal reactivation. Reactivation of the parasympathetic nervous system may result in decrease heart rate immediately after exercise, and reduced parasympathetic activity plays a principal role in attenuating the HRR.14 Although the relationship between an abnormal HRR and increased mortality is unclear, the possibility that attenuated HRR is strongly predictive of sudden cardiac death has been reported.15 The findings of this study suggested that most of the all-cause deaths, i.e. non-cardiac-related deaths, were caused by cancer, and there was no death related to coronary heart disease which is surprisingly because almost 60% of the population had coronary artery disease. Although the small sample size and well-preserved ejection fraction in the study population might prevent adverse cardiac outcomes, we hypothesized that in octogenarians, an attenuated HRR manifests not only as a cardiac events but also as a failure of general condition. We also assessed the resting heart rate before exercise testing in this study. Resting heart rate has been proposed as a global index of the autonomic nervous system's influence on the heart, and elevated heart rate might reflect a shift in autonomic balance toward enhanced sympathetic and suppressed vagal tone.16 We demonstrated a significant correlation between HRR and resting heart rate (although the degree of correlation was not strong), and this result also supports the contention that a decrease in vagal tone might cause adverse outcomes in treadmill exercise testing.
Previous studies have also reported that impaired functional capacity is an independent predictor of mortality in elderly subjects.7,17 However, in the present study, we found no significant association between impaired functional capacity and mortality. This result might be explained by the fact that the octogenarians included in this cohort had a relatively well-preserved functional capacity as indicated by examination. Only nine patients presented with impaired functional capacity, and this low number was not sufficient to reveal a significant association. This supposition is supported by the fact that the mean functional capacity as METs was relatively well preserved in the patients examined in this study, as described above.
Surprisingly, the resting heart rate was not significantly associated with all-cause death in this study. High heart rate is associated with an increased mortality rate in elderly patients.13 One explanation for the absence of any association between the resting heart rate and all-cause death is that the resting heart rate in our patients was relatively high, and the small cohort in our study may not have the statistical power to reveal significant associations. Moreover, our study revealed that 59 patients had prior coronary artery disease, but approximately half of the patients had a resting heart rate above 70beats/min, as shown in Figure 2. This finding may be explained by the fact that only five patients in our study received beta-blockers with heart rate-lowering activity. Numerous randomized trials, including trials in elderly patients, have shown the efficacy of beta-blockers in reducing mortality after myocardial infarction, and ACC–AHA guidelines recommend that prompt administration of beta-blockers as secondary therapeutic agents.18–20 However, in daily practice, administration of beta-blockers to elderly patients is not always in accordance with the guidelines. Poor tolerance, hypotension, bradycardia, and co-morbidities that are complicated by beta-blockers may deter physicians from administering beta-blockers to very elderly patients. Further, the mean ejection fraction was relatively preserved in echocardiography in our patient. Therefore, beta-blocker use for octogenarians in our study was relatively low in spite of the high prevalence of prior coronary artery disease, and this trend might be considered to be responsible for the high resting heart rate in our patients.
Although no therapeutic methods have been systematically evaluated for attenuated HRR, cardiac rehabilitation with coronary artery disease could improve the HRR response.21 Unfortunately only few patients in our study underwent systematic cardiac rehabilitation; because of the risk of complications, the physicians may have been reluctant to rehabilitation. Therefore, we could not evaluate the patient response to the exercise training scheme for HRR. Further studies are required to assess the attenuated HRR for improving the outcome in elderly patients.
Study limitations
There are several limitations to our study. First, the study was retrospective, and conducted with a small single-centre cohort. The selection of patients for the exercise examination was left to the discretion of the attending physician. Second, we adopted the cut-off value of abnormal HRR, impaired functional capacity, resting heart rate, and delayed SBP response by referring to other large cohort studies and did not determine the cut-off point directly in the elderly population. Third, the prevalence of cardiovascular drugs use was more likely to be low in our patients despite the presence of coronary artery disease. Although the population of the present study was high age, optimal medical therapy was not adequate for coronary artery disease in this study.
Conclusion
The findings of the present study indicate that attenuated HRR is a significant prognostic marker for all-cause death among octogenarians who are able to perform a treadmill exercise test. Although most subjects were unable to achieve the maximal predicted peak heart rate, the exercise protocol was performed safely and without major complications. Our study findings may provide helpful support for risk stratification in very elderly patients. Further prospective studies examining larger populations and seeking a better resolution of prognostic parameters are needed.
Conflict of interest: none declared.



