-
PDF
- Split View
-
Views
-
Cite
Cite
Antonio Curnis, Giuseppe Coppola, Marco Racheli, Manuel Cerini, Carlo Pagnoni, Alessandro Lipari, Nicola Berlinghieri, Mohamed A. Metwally, Luca Bontempi, Livio Dei Cas, Jugular pacing lead extraction with laser sheath: a case report, EP Europace, Volume 12, Issue 3, March 2010, Pages 447–448, https://doi.org/10.1093/europace/eup417
Close - Share Icon Share
Abstract
Over the past 20 years, the number of patients with pacemakers (PM) or implantable cardioverter defibrillators has risen markedly; consequently, an increasing number of lead-removal procedures have become necessary. A 64-year-old woman presenting with an infected device pocket and positive bacterial cultures ( Staphylococcus aureus ) was admitted to our department for lead removal; in 1991, she underwent VVI PM implantation for atrioventricular II degree Mobitz 1 block, and a unipolar lead was introduced via the left jugular vein. The procedure was performed in our Electrophysiology Lab with a cardiac surgeon on standby, using an excimer laser system emitting the energy at the tip of a flexible, fibre-optic 12 F sheath, developed by Spectranetics, Inc., Colorado Springs, CO, USA.
Case report
Over the past 20 years, the number of patients with pacemakers (PM) or implantable cardioverter defibrillators has risen markedly; consequently, an increasing number of lead-removal procedures have become necessary. In fact, of the 400 000–500 000 permanent PM leads implanted worldwide each year, around 10% may eventually fail or become infected, making them potential candidates for removal. 1–3 Common indications for removal include infection, vascular access issues, lead interactions, and lead recall from the manufacturer. Manual traction is often effective to remove leads implanted no more than a few months previously. However, leads that were implanted for longer periods of time characteristically develop fibrous attachments to the surrounding structures and require more advanced removal systems such as transvenous extraction (manual or laser) and surgical extraction. 4
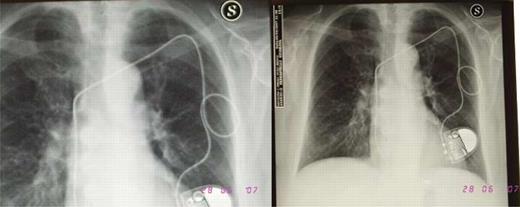
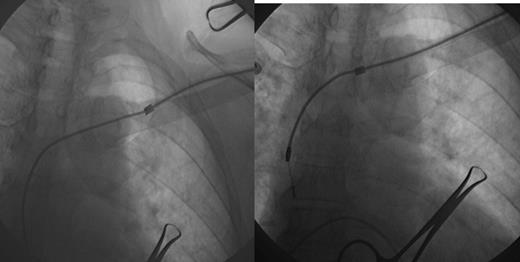
In June 2007, a 64-year-old woman was admitted to our department for lead extraction; in 1991, she underwent VVI PM implantation for atrioventricular II degree Mobitz 1 block, and a unipolar lead was introduced via the left jugular vein ( Figure 1 ). In November 2001, the patient underwent PM replacement, and in June 2006, she underwent pocket revision because of erosion of the generator. One year later, the woman was admitted once again to the hospital presenting signs and symptoms of infection of the device pocket and positive bacterial cultures ( Staphylococcus aureus ). Echocardiographic transthoracic and transoesophageal examinations did not show infection of the intravascular portion; so after 3 weeks of antibiotic therapy (ciprofloxacin), she underwent lead removal following temporary lead stimulation positioning in the right ventricular apex. The procedure was performed under local anaesthesia by our team in our Electrophysiology Lab with a cardiac surgeon on standby. We used an excimer laser system emitting the energy at the tip of a flexible, fibre-optic 12 F sheath, developed by Spectranetics Inc., Colorado Springs, CO, USA. After surgical revision of the pocket, isolation of the lead from fibrosis and positioning of the Spectranetics stylet no. 1 lead removal were performed ( Figure 2 ). We observed 6.5 cm of extensive fibrosis and calcification surrounding the distal part of the lead ( Figure 3 ). We did not observe any signs of pericardial effusion on echocardiography and/or hypotension. The patient was monitored for 12 h in our intensive care unit, and after 3 days, she underwent right VVI PM implantation.

Discussion
This is an experience of jugular pacing lead removal with laser sheath. The jugular vein approach is an old and rare approach for PM lead implantation, so there are few data about laser lead removal from this vein. 5 Laser technology is commonly employed in current lead-removal procedures. Fibrous adhesions are disrupted by a circumferential excimer laser beam applied to the tip of a specialized telescopic sheath which is passed over the lead to be removed. The laser source is a xenon chloride laser with an output of 308 nm, not visible to the human eye. It is a cool cutting laser (50°C) with a very limited absorption depth; two-thirds of the energy is absorbed within 0.06 mm from the tip of the sheath by proteins and lipids instead of water. The clinical significance of these parameters is that the excimer laser is well suited to ablate the fibrosis that usually binds to the leads; the fibrosis can be ablated without damaging the endothelial wall or the insulation of the extracted lead or the insulation of other leads. 6
In our opinion, lead extraction with the laser sheath can be safely performed with high success rates by physicians with implant experience, and major complications can be expected only in <2% of the patients. The time from the implant is the decisive factor in judging the potential efficacy of lead removal with direct traction. If leads have been implanted for more than 6 months, the use of additional extraction tools is necessary when lead removal is considered. 5 , 6
Conflict of interest: none declared.



