-
PDF
- Split View
-
Views
-
Cite
Cite
Béatrice Brembilla-Perrot, Laurent Groben, Frédéric Chometon, Jean Paul Lethor, Philippe Admant, Jean Louis Cloez, Irina Popescu, Cecile Marchal, Juanico Cedano, Ahmed Abdelaal, Olivier Huttin, Charif Tatar, Nacima Benzaghou, Berivan Azman, Arnaud Terrier De La Chaise, François Marçon, Rapid and low-cost method to prove the nature of no documented tachycardia in children and teenagers without pre-excitation syndrome, EP Europace, Volume 11, Issue 8, August 2009, Pages 1083–1089, https://doi.org/10.1093/europace/eup093
Close - Share Icon Share
Abstract
Symptoms in children are often difficult to interpret. The purpose of this study was to report the results of transoesophageal electrophysiological study (EPS) performed in children complaining of sudden onset tachycardia with normal non-invasive studies.
Eighty-two children and teenagers (mean age 15 ± 3 years) presented with suspected but no documented paroxysmal supraventricular tachycardia (SVT). ECG was normal. Non-invasive studies were negative; 23 children had syncope with tachycardias. They underwent transoesophageal EPS in our out-patient clinic. The mean duration of transoesophageal EPS was 11 ± 5 min. Electrophysiological study was negative in 25 children. AV nodal re-entrant tachycardia could be induced in 37 children, 11 of them associated with syncope. Wolff–Parkinson–White syndrome (WPW) was diagnosed in five children in which atrioventricular re-entrant tachycardia was inducible. Atrioventricular re-entrant tachycardia due to a concealed AP was induced in 14 children. Verapamil-sensitive ventricular tachycardia was induced in one patient.
Factors associated with tachycardia inducibility were an older age (15.5 ± 2 vs. 14 ± 4 years) ( P < 0.05) and the absence of syncope (81 vs. 52%) ( P < 0.05). During a mean follow-up of 3 ± 1 year, no patient with negative EPS developed documented tachycardia. In 17 children with inducible SVT, radiofrequency ablation of the re-entrant circuit was subsequently performed.
Transoesophageal EPS is a fast method for proving the nature of paroxysmal tachycardia in children and teenagers presenting with normal ECG and for demonstrating WPW syndrome not visible on standard ECG. The negative predictive value of transoesophageal EPS for the diagnosis of SVT was 100%.
Assessing the complaints of children is often difficult. In the setting of paroxysmal tachyarrhythmias in children, some of the younger patients complain of palpitations with a sudden onset frequently associated with symptoms, such as chest pain, dyspnoea, vertigo, or dizziness. In that case, paroxysmal supraventricular tachycardia (SVT) can be suspected, but non-invasive studies are frequently negative. Duration of the tachyarrhythmia is often too short in order to be recorded by standard ECG and generally only sinus tachycardia can be recorded after the episode. Furthermore, symptomatic episodes are rarely frequent enough to be recorded during conventional 24 h Holter monitoring. Sensitivity of exercise stress test for induction of arrhythmias is low. 1 Although ECG monitoring through implantable loop recorder can be indicated in children for evaluation of possible SVT, the slight scar resulting from its implantation can be traumatizing in children. Long-term Holter monitoring is difficult to use in children, and annoying at school. Finally, first line use of intracardiac electrophysiological study (EPS), which is the main technique to induce a paroxysmal tachycardia 2 is questionable in the absence of proof of real organic tachycardias in children or teenagers without structural heart disease, in which these tachycardias generally have a spontaneous favourable outcome.
The purpose of this study was to report the feasibility of transoesophageal EPS in out-clinic patients and to report the results of transoesophageal EPS in children complaining of palpitations presenting with normal non-invasive studies.
Population and methods
Study population
Eighty-two children and teenagers aged 7 to 19 years (mean age: 15 ± 3; 40 boys and 42 girls) were consecutively enrolled over a 10-year period for the assessment of potential paroxysmal SVT.
Twenty-three children complained of dizziness and at least one episode of syncope associated with tachycardias.
No tachycardia could be documented. The number of tachycardia events ranged from 1 to 10 episodes. A sportive activity or stress preceding the onset of symptoms was noted in 19 children. Sports in school had been contraindicated by their teacher in 12 children. Fifteen children, mainly girls, were considered as anxious or hysteric and had been treated with anxiolytic drugs. Ten children were treated with beta-blockers.
The ECG in sinus rhythm was normal and did not show pre-excitation syndrome.
Twenty-four hour Holter monitoring recorded in all children as well as exercise testing, performed in children with exercise or stress-related symptoms were negative.
Echocardiogram was normal in all children.
These children and teenagers were directly referred to our centre either by their adult or paediatric cardiologist after completion of non-invasive studies.
Methods
Children were in a fasting state for at least 3 h prior to undergoing transoesophageal EPS and were not sedated. All drugs were discontinued before EPS. A lidocaine patch was applied on the skin before gaining venous access for isoproterenol infusion. In the first period of the study, younger children were given pre-medication with 25 mg p.o. of hydroxyzine before EPS; later, pre-medication was abandoned because the tolerance to EPS was unchanged by the drug.
Informed and written consent was obtained from children and their parents.
The EPS was performed by transoesophageal route in our out-patient clinic, in the presence of the children's parents when the child was <11 years old. The study was performed in an electrophysiology laboratory equipped with adequate life-saving material and in the presence of qualified medical staff, after clear explanations of the technique. Patients were informed of the possibility of chest pain due to pacing current of more than 12–15 mA.
Oesophageal catheter (Fiab catheter, Ela Medical, France) was passed through the oral cavity and optimal oesophageal position was determined by the best recording site of oesophageal atrial activity. Oral cavity anaesthesia was only necessary in one child due to a too important nausea reflex and this child was not authorized to drink or eat for 1 h after the procedure.
Our protocol was previously reported. 2
Surface electrocardiograms and oesophageal electrogram were simultaneously recorded on paper at speeds of 25 or 100 mm/s (Bard system). Cardiac stimulation was performed with a biphasic stimulator (Micropace, Bard, France) used for intracardiac study. Pulses of 10 ms duration were used; output varied from 8 to 18 mA (mean 11 ± 2 mA).
Incremental atrial pacing was performed until type I second degree atrioventricular block occurred. Programmed atrial stimulation at a basic cycle length of 600 and 400 ms with the introduction of one and two extrastimuli was performed. When a SVT was induced, the protocol was stopped. In the absence of tachycardia induction, isoproterenol (0.02–1 µg min −1 ) was infused then to increase the sinus rate to at least 130 bpm and the pacing protocol was repeated.
Arterial blood pressure was continuously monitored during the study by an external sphygmomanometer (Baxter, Japan).
All children and teenagers were allowed to leave the hospital after EPS and were authorized to drink and eat immediately after the study except one boy in whom oral cavity anaesthesia was performed.
In children with syncope and negative study, head-up tilt testing without provocative drugs was performed in a second time. After 20 min in supine position, the electric table was moved to an upright position for 40 min or until syncope occurred. The incline angle in upright position was 80°. The ECG was continuously monitored and arterial blood pressure was measured by an external sphygmomanometer.
Follow-up
The mean follow-up ranged from 6 months to 5 years (mean 3 ± 1 year). In patients with inducible tachycardia and accessory pathway (AP), beta-blockers were generally prescribed, until radiofrequency ablation was discussed in case of tachycardia recurrence.
Measurements and definitions
Sustained supraventricular tachyarrhythmia was defined as a tachycardia lasting 1 min or longer.
When tachycardia was induced, the atrial electrocardiogram was recorded in order to determine the exact nature of the induced arrhythmia. In the case of provoked paroxysmal SVT which could be reproducibly induced and stopped by atrial stimulation, we have used previously reported criteria to determine the nature of the arrhythmia, including measurement of ventriculoatrial interval and morphology of atrial activity in leads D1, D3, and V1: 3 , 4 atrial activity was inside the ventriculogram and not visible in these leads but only on the oesophageal electrogram when AV nodal re-entrant tachycardia (AVNRT) was induced; when atrial activity followed the ventriculogram, the negativity of P wave in lead D3 indicated a junctional tachycardia; the negativity of P wave in D1, and/or a P wave occurring after the atrial oesophageal electrogram were in favour of a re-entrant tachycardia via a concealed left AP. 4 When P wave was positive in D1 and P wave in V1 occurred before oesophageal atrial activity, possible mechanisms included atypical AV node re-entrant tachycardia or a re-entry through a concealed septal or right AP. Paroxysmal SVT was induced several times to provoke a functional bundle branch block and to note changes in VA interval at this time.
Head-up tilt testing was considered positive either if syncope was induced by tilting or a decrease in systolic blood pressure below 90 mmHg associated with symptoms of impending syncope 5 , 6 were recorded.
Statistical analysis
Data were expressed as the mean ± standard deviation. Statistical analysis used the Student's t paired test for quantitative data and the χ 2 test for discrete variables and ordinal tests. A P -value < 0.05 was considered as significant.
Results
Feasibility of transoesophageal study
Electrophysiological study was performed in all children but one with syncope, excluded from the study. The mean duration of EPS was 11 ± 5 min. The total procedure time including explanations given to the patient and his family members before and after the study was 30 ± 12 min. Radiation was not used. Mean output used to pace left atrium ranged from 8 to 18 mA (mean 11 ± 2 mA) with an impulse duration of 10 ms.
The main difficulty was represented by nauseous reflex, nausea, or vomiting induced by the oesophageal probe which frequently occurred in the youngest children. Chest pain was rarely noted, as well as anxiety at the beginning of the study secondary to the feeling of pacing.
Results of electrophysiological study
Electrophysiological study remained negative in 25 children, 12 boys, 13 girls aged 7–19 years (mean 15.5 ± 2) and symptoms were attributed to sinus tachycardia generally induced by isoproterenol infusion reproducing symptoms described during clinical tachycardia.
AV nodal re-entrant tachycardia was induced in 37 children, 15 boys and 22 girls mean age 16 ± 2; 11 of them had syncope ( Figure 1 ). Atrioventricular re-entrant tachycardia (AVRT) was induced in control state in 19 children and only after isoproterenol infusion in 18 children.
Wolff–Parkinson–White (WPW) syndrome related to a left lateral AP was identified in five children during atrial pacing and an AVRT was induced by programmed stimulation ( Figure 2 ), in control state in four of them and after isoproterenol in remaining one. This was the case with three boys and two girls aged 13–18 years (mean 16 ± 2). The maximal atrial stimulation rate conducted through the AP ranged from 80 up to 160 bpm (mean 120 ± 37 bpm) in control state and from 100 to 260 bpm after isoproterenol infusion (mean 136 ± 90 bpm). Atrioventricular re-entrant tachycardia through a concealed AP was induced in 14 other children, 9 boys and 5 girls (mean age 15 ± 3.5); there was no anterograde conduction over the AP and none of these children had syncope. Isoproterenol infusion was required to induce AVRT in only two children.
Verapamil-sensitive ventricular tachycardia was induced after isoproterenol infusion in one 16-year-old boy ( Figure 3 ).
Atrial fibrillation was also induced in four children with inducible AVNRT or AVRT, but was considered without clinical significance.
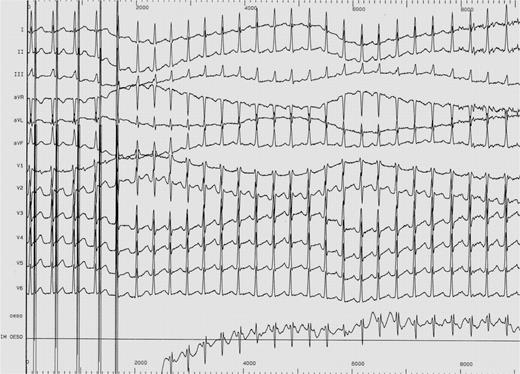
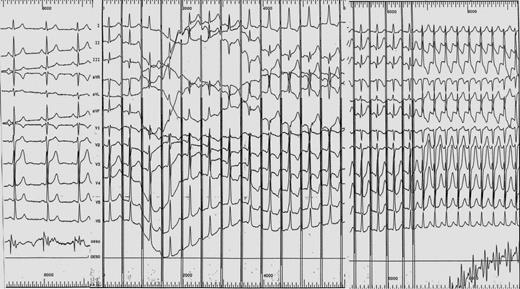
Child with a normal ECG; appearance of a typical Wolff–Parkinson–White syndrome during atrial pacing; induction of AV re-entrant tachycardia.
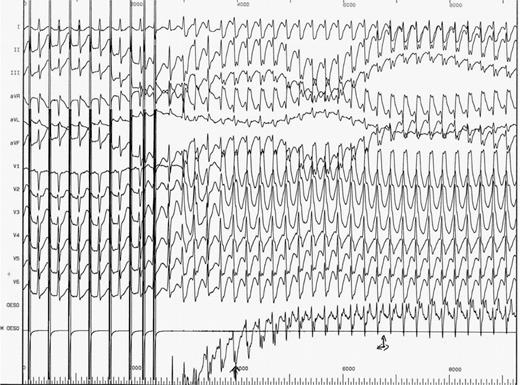
Induction of a wide QRS tachycardia with a right bundle branch block and left atrial deviation morphology; AV dissociation (progressive prolongation of VA interval) in favour of a verapamil-sensitive ventricular tachycardia.
The factors associated with induction of tachycardia were the older age (15.5 ± 2 vs. 14 ± 4 years) ( P < 0.05) and absence of syncope (82 vs. 58%) ( P < 0.05) ( Table 1 ).
| . | Negative study ( n = 25) . | Positive study ( n = 57) . | . |
|---|---|---|---|
| Age (years) | 14 ± 4 | 15.5 ± 2 | P < 0.02 |
| Male sex | 12 (48%) | 28 (49%) | NS |
| Syncope | 12 (48%) | 11 (19%) | P < 0.05 |
| Number of syncope | 4 ± 2 | 3 ± 2 | NS |
| . | Negative study ( n = 25) . | Positive study ( n = 57) . | . |
|---|---|---|---|
| Age (years) | 14 ± 4 | 15.5 ± 2 | P < 0.02 |
| Male sex | 12 (48%) | 28 (49%) | NS |
| Syncope | 12 (48%) | 11 (19%) | P < 0.05 |
| Number of syncope | 4 ± 2 | 3 ± 2 | NS |
| . | Negative study ( n = 25) . | Positive study ( n = 57) . | . |
|---|---|---|---|
| Age (years) | 14 ± 4 | 15.5 ± 2 | P < 0.02 |
| Male sex | 12 (48%) | 28 (49%) | NS |
| Syncope | 12 (48%) | 11 (19%) | P < 0.05 |
| Number of syncope | 4 ± 2 | 3 ± 2 | NS |
| . | Negative study ( n = 25) . | Positive study ( n = 57) . | . |
|---|---|---|---|
| Age (years) | 14 ± 4 | 15.5 ± 2 | P < 0.02 |
| Male sex | 12 (48%) | 28 (49%) | NS |
| Syncope | 12 (48%) | 11 (19%) | P < 0.05 |
| Number of syncope | 4 ± 2 | 3 ± 2 | NS |
Syncope was attributed to AVNRT in 11 of 23 children and teenagers with tachycardia and syncope. They all recognized the symptoms preceding syncope. Syncope was imputable to the rapid heart rate during SVT or to vagal reaction after SVT termination.
Among children with syncope and negative EPS, the head-up tilt test was positive in eight of them and syncope was preceded by adrenergic sinus tachycardia.
Cost of the evaluation
It was limited to the cost of the oesophageal catheter which is disposable according to French legislation (150 Euros) and to a consultation (77 Euros). Intracardiac electrophysiologic study requires a short hospitalization of 2 days (1080 Euros × 2) or a 1 day hospitalisation, but the cost of this hospitalization called (‘day hospitalization’) is 2025 Euros in France and can vary between hospitals.
The cost of event recorder, which has no specific price in our hospital, is similar to the cost of oesophageal study; the cost of implantable loop recorder is much expensive than oesophageal study (between 2399 and 2625 Euro).
Management
The children with a negative study were not given medication and were encouraged to continue or practice a sport activity. After a mean follow-up of 3 ± 1 years, no child developed documented tachycardia. Long-term Holter monitoring was used in three teenagers and sinus tachycardia was recorded.
Children with induced SVT were generally treated with small doses of beta-blockers until at least the age of 12 years; then the treatment was stopped. Radiofrequency ablation of the re-entrant circuit was performed successfully in 17 of 18 children several months or years later, 10 with AVNRT and 8 with AVRT. The ablation was unsuccessful in one child. The initial diagnosis was confirmed by intracardiac EPS. Indications for ablation were recurrence of symptoms after discontinuation of drugs, the wish of the child to stop medical treatment or to practice a sport requiring medical certification to compete. Remaining children are free of tachycardia, but 10 of them are under beta-blockers or antiarrhythmic drugs; all of them continue a leisure sportive activity and sports at school.
The negative predictive value of oesophageal EPS was 100%. Children with induced SVT and the boy with induced VT were treated with beta-blockers; in 29 of them, SVT did not recur after interruption of drugs. Therefore, it is difficult to know the exact positive predictive value of the technique for the evaluation of tachycardias.
Discussion
Our study reports a high incidence of inducible tachycardia among children or teenagers complaining of tachycardia with sudden onset. AVNRT was the most frequent tachycardia diagnosed in this population. Identification of the cause of symptoms was considered a key issue for the management of our patients. The mechanism of tachycardia could be understood through oesophageal EPS. The results of our study guided our therapeutic approach: we could discuss either no medical treatment at all in children who had only presented one tachycardia episode with explanation of vagal manoeuvres, or of a medical treatment when tachycardias were recurrent or of catheter ablation in children with bad-tolerated tachycardias aged more than 12 years. In the present study, 18 children or teenagers could benefit from a curative treatment by catheter ablation of the re-entrant circuit after identification of the tachycardia. In children with negative EPS, a common sinus tachycardia was diagnosed and we looked for the most likely mechanisms. Sport activity was encouraged in all children and sport at school was recommended in children with sinus tachycardia. None of them developed documented re-entrant tachycardias.
When a child or teenager complains of tachycardia, especially occurring after stress and when ECG, echocardiogram, Holter monitoring, and exercise testing are normal, the symptoms are generally attributed to sinus tachycardia.
However, paroxysmal SVT is known as a relatively frequent tachycardia with 89 000 new cases per year 7 and 570 000 patients with paroxysmal tachycardia in the USA. The estimated prevalence is 2.25/1000 persons and the incidence 35/100 000 person-years. These values are probably underestimated because some patients possibly have only one episode of tachycardia. 8
When the tachycardia is of relatively short duration, it is difficult to prove its nature. The probability of recording the tachycardia during a 24 h Holter monitoring is low; it is more frequent to record a rapid sinus tachycardia during activity in the youth. Exercise testing has also a low sensitivity for proving the tachycardia's origin. The induction of a SVT is noted in 6% of patients with arrhythmias and its occurrence during exercise is predictive of the recurrence of tachycardia. 1 Therefore, some girls are considered as hysteric. A non-specific treatment with beta-blockers is frequently undertaken.
Until the development of event recorder and implantable loop recorder, the main means for identifying a paroxysmal SVT is the EPS; the re-entrant tachycardia is easily induced by programmed stimulation. 2 However, the intracardiac route is an invasive method which is generally indicated only in children or teenagers with repeated documented tachycardias in view of radiofrequency ablation of the arrhythmia. The catheterism is also associated with a risk of complications 9 and radiation exposure. 10 Therefore, another method of atrial programmed stimulation was developed several years ago 3 , 11–13 and was shown as effective as intracardiac route. 14 We previously reported the interest of the technique for evaluating the mechanism of paroxysmal tachycardia in children or teenagers 15 and then to study the relationships between paroxysmal tachycardia and syncope. 16 In the present study, a paroxysmal AVNRT or AVRT was frequently induced. Furthermore, a patent WPW syndrome was identified in five children; the prognosis of these children could be different with a risk of life-threatening arrhythmias; 17 , 18 however, the maximal atrial rate conducted through the AP was lower than the rate conduction through the normal AV system in our group.
The EPS was more frequently negative in children with syncope associated with tachycardia than in those without syncope. However, 11 of 23 children had inducible AVNRT associated with syncope; in 6 of them a fast heart rate during tachycardia explained syncope. In five other children, vagal reaction with decrease of arterial blood pressure and bradycardia was noted after the termination of tachycardia. 16 The relationship between paroxysmal tachycardia and syncope was previously reported by Beder et al.19 and Drago et al . 20 But, more frequently, tachycardia was shown to be related to an adrenergic tachycardia which preceded syncope and symptoms were related to a vasovagal phenomenon. Head up tilt test is clearly recommended in this population to avoid EPS.
Children with syncope and feeling tachycardia could be actually preferentially evaluated by the implantation of a loop recorder. 21 The implantable loop recorder appeared in the study of Yeung et al . 21 to be an excellent method of effecting a ‘cure’ in 44.1% of subjects because symptoms resolved after implantation. In those who remained symptomatic, it was successful in determining cardiac rhythm during symptoms, but the complication rate in children could be higher than that of adults. Children with only tachycardia could now benefit of the technical progress of the new event recorders. However, the child can remain asymptomatic even after a real SVT; the natural follow-up of patients with paroxysmal SVT indicates a natural disappearance in 40% of subjects. 8 This natural favourable evolution can also explain the absence of recurrence of tachycardia in 29 of our children with inducible AVNRT or AVRT after interruption of beta-blockers.
Limits of study . The population of our study was selected by a referring cardiologist and did not represent all children with a feeling of tachycardia. Only those who were highly symptomatic or those with clinical presentation suggestive of paroxysmal tachycardia were addressed for the study. Therefore, the real prevalence of paroxysmal SVT in the youth complaining of tachycardia is probably lower.
In children with negative study, we cannot exclude with certainty a ventricular tachycardia, but this type of tachycardia is rare in children 22 and generally can also be induced by atrial pacing as in one boy in our population. The follow-up did not reveal ventricular tachycardia in the youth with a negative study.
The head-up tilt test was performed after EPS and probably some indications could have been avoided. But in our hospital, it is easier to perform oesophageal study which is less time consuming than tilt test and waiting lists for oesophageal EPS are shorter than for tilt testing.
At least, some teenagers could benefit from the development of newer auto-capture event recorders. Among the last recruited teenagers in our study with a negative oesophageal EPS who still complained of tachycardia, the 3 weeks Holter recording system from Sorin (Spiderflash), however, only recorded sinus tachycardia.
In conclusion, transoesophageal EPS was a fast and low-cost method to prove the nature of paroxysmal tachycardia in children and teenagers with a normal ECG and to prove a WPW syndrome not visible in sinus rhythm. Tachycardia was induced in 69.5% of them. However, in the case of associated syncope, systematic head-up tilt test should be performed before EPS; the feeling of tachycardia can be due to adrenergic sinus tachycardia.
Conflict of interest: none declared.



