-
PDF
- Split View
-
Views
-
Cite
Cite
Kakhaber Etsadashvili, Florian Hintringer, Markus Stühlinger, Wolfgang Dichtl, Karin Spuller, Herwig Antretter, Herbert Hangler, Otmar Pachinger, Franz Xaver Roithinger, Thomas Berger, Long-term results of high vs. normal impedance ventricular leads on actual (Real-Life) pacemaker generator longevity, EP Europace, Volume 11, Issue 2, February 2009, Pages 200–205, https://doi.org/10.1093/europace/eun328
Close - Share Icon Share
Abstract
The long-term effects of high impedance vs. standard impedance pacing leads on actual generator longevity were studied.
In 40 patients (21 females, age 73 ± 13 years) with standard dual-chamber pacemaker indication, bipolar standard impedance ventricular leads and high-impedance leads were implanted in a randomized fashion. Identical pacemaker generators and atrial pacing leads were implanted in all patients. Patients were observed during a mean follow-up of 89.8 ± 8.8 months before pacemaker replacement. Initially, the patients who received the high-impedance leads had a lower current drain as compared with standard pacing impedance leads, and the estimated pacemaker longevity was significantly prolonged, too. But this pattern disappeared after 6 years of follow-up, and finally the actual pacemaker generators’ replacement time was 86.7 ± 6.8 months in standard impedance lead group vs. 91.2 ± 10.3 months in high-impedance lead group ( P = 0.17).
Implantation of high pacing impedance leads for ventricular stimulation does not result in a benefit with respect to pacemaker longevity as compared with standard impedance leads.
Introduction
Parameters such as battery capacity, electronic circuit current drain, programmed output, and pacing system impedance determine pacemaker generator longevity. 1–7 The energy consumption of a pacing system strongly depends on the electronic consumption of the device itself and on the stimulation current. In the course of reducing the pacemaker’s size and the implementation of more sophisticated algorithms, continuous efforts have been made to minimize energy consumption. As determined by Ohm’s law ( I = V / R ), the use of high-impedance leads reduce current drain 8 and therefore decrease the amount of electrical current delivered during each pacing pulse. This effect of high-impedance leads will be even more pronounced at high output levels. The pacing impedance at the lead to tissue interface is increased by downsizing the lead tip surface area, resulting in an increased current density. While previous studies suggested that these electrical characteristics provide an enhancement of pacemaker longevity, high-impedance leads were considered as the ‘best choice’. 1–7
In all of these studies, pacemaker longevity was estimated by a pacemaker algorithm, but none of them checked the real-life pacemaker longevity with respect to actual generator replacement time.
Therefore, the aim of this prospective randomized study was to evaluate the impact of high pacing impedance leads on the pacemaker generators’ actual replacement time during long-term follow-up.
Patients and methods
Forty patients were studied with a standard pacemaker indication 9 ( Table 1 ). To exclude the influence of different pacemakers and atrial leads, identical dual-chamber devices (Medtronic Kappa KDR 401, Medtronic Inc., Minneapolis, MN, USA) were implanted, using standard implantation techniques, and all patients received identical active-fixation atrial leads (CapSure Fix ® , model 5068, bipolar, Medtronic Inc.). Leads were inserted through either the right or the left subclavian vein.
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 20 | 20 | NS |
| Age (years) | 68 ± 17 | 65 ± 14 | NS |
| Female | 10 (50%) | 11 (55%) | NS |
| Follow-up (months) | 55.2 ± 31.2 | 55.2 ± 30.0 | NS |
| Indication for pacing | |||
| AV-block | 3 | 3 | NS |
| Sinus node disease | 17 | 17 | NS |
| Coronary heart disease | 2 (10%) | 3 (15%) | NS |
| Valvular heart disease | 1 (5%) | 2 (10%) | NS |
| Diabetes mellitus | 1 (5%) | 5 (25%) | P < 0.05 |
| Hypertension | 11 (55%) | 7 (35%) | NS |
| Ejection fraction (%) | 54 ± 12 | 52 ± 10 | NS |
| ASVS (%) | 3.5 ± 7.8 | 1.4 ± 4.2 | NS |
| ASVP (%) | 37.6 ± 43.5 | 39.9 ± 79.5 | NS |
| APVS (%) | 0.4 ± 1.1 | 0.5 ± 1.3 | NS |
| APVP (%) | 58.6 ± 40.7 | 57.4 ± 29.8 | NS |
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 20 | 20 | NS |
| Age (years) | 68 ± 17 | 65 ± 14 | NS |
| Female | 10 (50%) | 11 (55%) | NS |
| Follow-up (months) | 55.2 ± 31.2 | 55.2 ± 30.0 | NS |
| Indication for pacing | |||
| AV-block | 3 | 3 | NS |
| Sinus node disease | 17 | 17 | NS |
| Coronary heart disease | 2 (10%) | 3 (15%) | NS |
| Valvular heart disease | 1 (5%) | 2 (10%) | NS |
| Diabetes mellitus | 1 (5%) | 5 (25%) | P < 0.05 |
| Hypertension | 11 (55%) | 7 (35%) | NS |
| Ejection fraction (%) | 54 ± 12 | 52 ± 10 | NS |
| ASVS (%) | 3.5 ± 7.8 | 1.4 ± 4.2 | NS |
| ASVP (%) | 37.6 ± 43.5 | 39.9 ± 79.5 | NS |
| APVS (%) | 0.4 ± 1.1 | 0.5 ± 1.3 | NS |
| APVP (%) | 58.6 ± 40.7 | 57.4 ± 29.8 | NS |
Values are mean ± SD.
ASVS, percentage of atrial sensed/ventricular sensed events; ASVP, percentage of atrial sensed/ventricular paced events; APVS, percentage of atrial paced/ventricular sensed events; APVP, percentage of atrial paced/ventricular paced events.
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 20 | 20 | NS |
| Age (years) | 68 ± 17 | 65 ± 14 | NS |
| Female | 10 (50%) | 11 (55%) | NS |
| Follow-up (months) | 55.2 ± 31.2 | 55.2 ± 30.0 | NS |
| Indication for pacing | |||
| AV-block | 3 | 3 | NS |
| Sinus node disease | 17 | 17 | NS |
| Coronary heart disease | 2 (10%) | 3 (15%) | NS |
| Valvular heart disease | 1 (5%) | 2 (10%) | NS |
| Diabetes mellitus | 1 (5%) | 5 (25%) | P < 0.05 |
| Hypertension | 11 (55%) | 7 (35%) | NS |
| Ejection fraction (%) | 54 ± 12 | 52 ± 10 | NS |
| ASVS (%) | 3.5 ± 7.8 | 1.4 ± 4.2 | NS |
| ASVP (%) | 37.6 ± 43.5 | 39.9 ± 79.5 | NS |
| APVS (%) | 0.4 ± 1.1 | 0.5 ± 1.3 | NS |
| APVP (%) | 58.6 ± 40.7 | 57.4 ± 29.8 | NS |
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 20 | 20 | NS |
| Age (years) | 68 ± 17 | 65 ± 14 | NS |
| Female | 10 (50%) | 11 (55%) | NS |
| Follow-up (months) | 55.2 ± 31.2 | 55.2 ± 30.0 | NS |
| Indication for pacing | |||
| AV-block | 3 | 3 | NS |
| Sinus node disease | 17 | 17 | NS |
| Coronary heart disease | 2 (10%) | 3 (15%) | NS |
| Valvular heart disease | 1 (5%) | 2 (10%) | NS |
| Diabetes mellitus | 1 (5%) | 5 (25%) | P < 0.05 |
| Hypertension | 11 (55%) | 7 (35%) | NS |
| Ejection fraction (%) | 54 ± 12 | 52 ± 10 | NS |
| ASVS (%) | 3.5 ± 7.8 | 1.4 ± 4.2 | NS |
| ASVP (%) | 37.6 ± 43.5 | 39.9 ± 79.5 | NS |
| APVS (%) | 0.4 ± 1.1 | 0.5 ± 1.3 | NS |
| APVP (%) | 58.6 ± 40.7 | 57.4 ± 29.8 | NS |
Values are mean ± SD.
ASVS, percentage of atrial sensed/ventricular sensed events; ASVP, percentage of atrial sensed/ventricular paced events; APVS, percentage of atrial paced/ventricular sensed events; APVP, percentage of atrial paced/ventricular paced events.
Twenty patients were randomly assigned to implantation of a standard impedance ventricular lead (model 1452T, St Jude Medical, St Paul, MN, USA) or a high impedance ventricular lead (CapSure Z ® , model 5034, Medtronic Inc.). The 1452T lead is a steroid-eluting 3.5 mm 2 hemispherical bipolar electrode, coated with titanium nitride. The CapSure Z lead is also a steroid-eluting bipolar electrode with a 1.2 mm 2 microporous platinum coating. Both leads are silicone insulated and have an identical NP35N conductor design.
For an intention-to-treat analysis, all patients were included. To provide comparable pacing conditions, a secondary analysis (per protocol analysis) was performed. For this purpose, only patients with constant programming of the pacing parameters during the complete follow-up period (and did not miss a single follow-up visit) were included. Finally, 10 patients in the standard impedance pacing lead group and 6 patients in the high impedance pacing lead group completed the whole follow-up until elective pacemaker generator replacement in the per protocol population. Twenty-four patients were excluded from secondary analysis due to deviation of pacing conditions [sustained threshold rise of the atrial ( n = 8) or ventricular lead ( n = 3)], death ( n = 7), upgrade to other pacing system ( n = 3), or further follow-up at a referring hospital ( n = 3). Patients’ characteristics were similar in both groups ( Tables 1 and 2 ). Follow-up was performed within 2 days after implantation procedure and after 3, 9, 27 and 39 months, then once a year until 60 months and afterwards twice a year. At each visit, parameters such as pacing lead impedance, pulse duration, pacing thresholds, voltage thresholds, number of paced and sensed events, and the P- and R-wave amplitudes were assessed. Furthermore, during follow-up period estimated mean, minimum, and maximum generator longevity was calculated by a pacemaker algorithm.
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 10 | 6 | NS |
| Age (years) | 72 ± 13 | 74 ± 11 | NS |
| Female | 6 (60%) | 3 (50%) | NS |
| Follow-up (months) | 86.7 ± 6.8 | 92.8 ± 10.3 | NS |
| Indication for pacing | |||
| AV-block | 1 | 1 | NS |
| Sinus node disease | 9 | 5 | NS |
| Coronary heart disease | 0 | 0 | NS |
| Valvular heart disease | 0 | 0 | NS |
| Diabetes mellitus | 0 | 1 | NS |
| Hypertension | 5 (50%) | 2 (33%) | NS |
| Ejection fraction (%) | 52 ± 13 | 50 ± 8 | NS |
| ASVS (%) | 3.2 ± 7.3 | 1.6 ± 4.5 | NS |
| ASVP (%) | 36.8 ± 42.3 | 38.3 ± 69.3 | NS |
| APVS (%) | 0.6 ± 1.3 | 0.5 ± 1.1 | NS |
| APVP (%) | 57.8 ± 43.4 | 58.6 ± 26.4 | NS |
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 10 | 6 | NS |
| Age (years) | 72 ± 13 | 74 ± 11 | NS |
| Female | 6 (60%) | 3 (50%) | NS |
| Follow-up (months) | 86.7 ± 6.8 | 92.8 ± 10.3 | NS |
| Indication for pacing | |||
| AV-block | 1 | 1 | NS |
| Sinus node disease | 9 | 5 | NS |
| Coronary heart disease | 0 | 0 | NS |
| Valvular heart disease | 0 | 0 | NS |
| Diabetes mellitus | 0 | 1 | NS |
| Hypertension | 5 (50%) | 2 (33%) | NS |
| Ejection fraction (%) | 52 ± 13 | 50 ± 8 | NS |
| ASVS (%) | 3.2 ± 7.3 | 1.6 ± 4.5 | NS |
| ASVP (%) | 36.8 ± 42.3 | 38.3 ± 69.3 | NS |
| APVS (%) | 0.6 ± 1.3 | 0.5 ± 1.1 | NS |
| APVP (%) | 57.8 ± 43.4 | 58.6 ± 26.4 | NS |
Values are mean ± SD.
ASVS, percentage of atrial sensed/ventricular sensed events; ASVP, percentage of atrial sensed/ventricular paced events; APVS, percentage of atrial paced/ventricular sensed events; APVP, percentage of atrial paced/ventricular paced events.
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 10 | 6 | NS |
| Age (years) | 72 ± 13 | 74 ± 11 | NS |
| Female | 6 (60%) | 3 (50%) | NS |
| Follow-up (months) | 86.7 ± 6.8 | 92.8 ± 10.3 | NS |
| Indication for pacing | |||
| AV-block | 1 | 1 | NS |
| Sinus node disease | 9 | 5 | NS |
| Coronary heart disease | 0 | 0 | NS |
| Valvular heart disease | 0 | 0 | NS |
| Diabetes mellitus | 0 | 1 | NS |
| Hypertension | 5 (50%) | 2 (33%) | NS |
| Ejection fraction (%) | 52 ± 13 | 50 ± 8 | NS |
| ASVS (%) | 3.2 ± 7.3 | 1.6 ± 4.5 | NS |
| ASVP (%) | 36.8 ± 42.3 | 38.3 ± 69.3 | NS |
| APVS (%) | 0.6 ± 1.3 | 0.5 ± 1.1 | NS |
| APVP (%) | 57.8 ± 43.4 | 58.6 ± 26.4 | NS |
| Ventricular lead . | Patient population . | ||
|---|---|---|---|
| . | Standard impedance . | High impedance . | Significance . |
| Number of patients | 10 | 6 | NS |
| Age (years) | 72 ± 13 | 74 ± 11 | NS |
| Female | 6 (60%) | 3 (50%) | NS |
| Follow-up (months) | 86.7 ± 6.8 | 92.8 ± 10.3 | NS |
| Indication for pacing | |||
| AV-block | 1 | 1 | NS |
| Sinus node disease | 9 | 5 | NS |
| Coronary heart disease | 0 | 0 | NS |
| Valvular heart disease | 0 | 0 | NS |
| Diabetes mellitus | 0 | 1 | NS |
| Hypertension | 5 (50%) | 2 (33%) | NS |
| Ejection fraction (%) | 52 ± 13 | 50 ± 8 | NS |
| ASVS (%) | 3.2 ± 7.3 | 1.6 ± 4.5 | NS |
| ASVP (%) | 36.8 ± 42.3 | 38.3 ± 69.3 | NS |
| APVS (%) | 0.6 ± 1.3 | 0.5 ± 1.1 | NS |
| APVP (%) | 57.8 ± 43.4 | 58.6 ± 26.4 | NS |
Values are mean ± SD.
ASVS, percentage of atrial sensed/ventricular sensed events; ASVP, percentage of atrial sensed/ventricular paced events; APVS, percentage of atrial paced/ventricular sensed events; APVP, percentage of atrial paced/ventricular paced events.
All pacemakers were programmed at a minimum three-fold safety pacing margin and a 2.5-fold sensing margin. To exclude post-operative elevation of pacing thresholds, the evaluation started 3 months after pacemaker implantation. All parameters were acquired non-invasively through pacemaker telemetry using the Medtronic 9790C programmer. The study was approved by the local ethics committee, and written informed consent was obtained from all patients prior to enrolment.
Statistical methods
All data are presented as mean values ± SD. Statistical analysis was performed on an intention-to-treat basis (including all randomized patients). A secondary analysis was performed in the per protocol population (patients with stable threshold, followed until generator replacement). Student’s t -test was used to compare data for primary and for secondary analysis. A P -value of <0.05 was considered statistically significant.
Results
The two patient groups did not differ with respect to atrial and ventricular lead performance as well as lead-related complications. They did also show no significant differences in the number of atrial and ventricular paced and sensed events, atrial and ventricular sensing properties and pacing properties (pacing output and impulse duration) in the intention-to-treat as well as in the per protocol analysis ( Tables 1 and 2 , Figure 1 ). At the 27 month follow-up, battery measurements revealed no significant differences between both groups with respect to battery voltage, battery current, and battery impedance. However, after a 39 month follow-up period, the standard impedance lead group displayed a significantly higher battery current as compared with the high-impedance lead group (20.6 ± 1.9 vs. 18.9 ± 1.1 μA; P < 0.05) and the extrapolated generator longevity was significantly longer in the high-impedance lead group (107.3 ± 8.4 vs. 97.6 ± 9.0 months; P < 0.05) 4 in the per protocol population ( Figure 2 , Table 3 ). However, in the intention-to-treat population, these differences between normal and high-impedance lead groups in battery current (20.1±1.6 vs. 21.7 ± 7.7 µA; P = ns) and extrapolated generator longevity (75.2 ± 9.9 vs. 74.1 ± 14.1 months; P = ns) were not statistically significant.
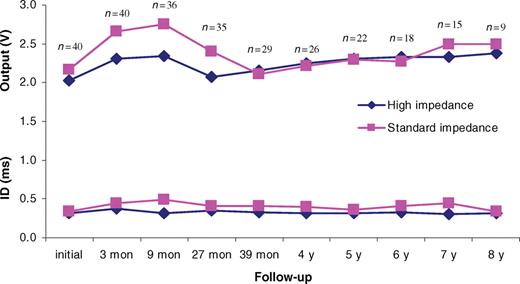
Ventricular pacing output and impulse duration (ID) (intention-to-treat population; * P < 0.05; n = number of patients).
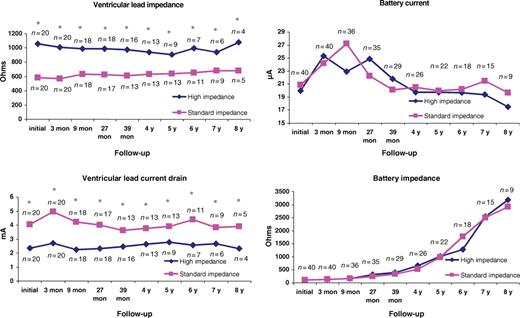
Ventricular lead impedance, ventricular lead current drain, battery current and battery impedance during the follow-up period (Intention-to-treat population; * P < 0.05; n = number of patients).
Calculated and actual generator longevity during the follow-up period of eight years
| Follow-up . | Estimated pacemaker longevity (mean) . | Actual longevity . | ||
|---|---|---|---|---|
| . | 39 months . | 6 year . | 8 year . | . |
| High impedance | 97.4 ± 7.8 | 30.6 ± 6.2 | 12.3 ± 0.3 | 91.2 ± 10.3 |
| Standard impedance | 88.7 ± 8.2 | 22.9 ± 9.6 | 11.3 ± 2.1 | 86.7 ± 6.8 |
| Difference (months) | 8.7 | 7.7 | 1.0 | 4.5 |
| Number of patients (high/standard lead group) | 24 (12/12) | 16 (6/10) | 6 (3/3) | 16 (6/10) |
| P -value | <0.05 | <0.05 | ns | ns |
| Follow-up . | Estimated pacemaker longevity (mean) . | Actual longevity . | ||
|---|---|---|---|---|
| . | 39 months . | 6 year . | 8 year . | . |
| High impedance | 97.4 ± 7.8 | 30.6 ± 6.2 | 12.3 ± 0.3 | 91.2 ± 10.3 |
| Standard impedance | 88.7 ± 8.2 | 22.9 ± 9.6 | 11.3 ± 2.1 | 86.7 ± 6.8 |
| Difference (months) | 8.7 | 7.7 | 1.0 | 4.5 |
| Number of patients (high/standard lead group) | 24 (12/12) | 16 (6/10) | 6 (3/3) | 16 (6/10) |
| P -value | <0.05 | <0.05 | ns | ns |
Values are mean ± SD.
Calculated and actual generator longevity during the follow-up period of eight years
| Follow-up . | Estimated pacemaker longevity (mean) . | Actual longevity . | ||
|---|---|---|---|---|
| . | 39 months . | 6 year . | 8 year . | . |
| High impedance | 97.4 ± 7.8 | 30.6 ± 6.2 | 12.3 ± 0.3 | 91.2 ± 10.3 |
| Standard impedance | 88.7 ± 8.2 | 22.9 ± 9.6 | 11.3 ± 2.1 | 86.7 ± 6.8 |
| Difference (months) | 8.7 | 7.7 | 1.0 | 4.5 |
| Number of patients (high/standard lead group) | 24 (12/12) | 16 (6/10) | 6 (3/3) | 16 (6/10) |
| P -value | <0.05 | <0.05 | ns | ns |
| Follow-up . | Estimated pacemaker longevity (mean) . | Actual longevity . | ||
|---|---|---|---|---|
| . | 39 months . | 6 year . | 8 year . | . |
| High impedance | 97.4 ± 7.8 | 30.6 ± 6.2 | 12.3 ± 0.3 | 91.2 ± 10.3 |
| Standard impedance | 88.7 ± 8.2 | 22.9 ± 9.6 | 11.3 ± 2.1 | 86.7 ± 6.8 |
| Difference (months) | 8.7 | 7.7 | 1.0 | 4.5 |
| Number of patients (high/standard lead group) | 24 (12/12) | 16 (6/10) | 6 (3/3) | 16 (6/10) |
| P -value | <0.05 | <0.05 | ns | ns |
Values are mean ± SD.
Both in the intention-to-treat as well as in the per protocol population, the high-impedance lead group showed a significantly higher pacing lead impedance as compared with the standard impedance lead group during the complete follow-up period ( Figures 2 and 3 ). Also, the high-impedance lead group displayed a trend to a slight decrease in pacing impedance whereas the standard impedance lead group showed a trend to a slight increase of pacing impedance during the whole follow-up period (although both not statistically significant). The Current drain was significantly lower in the high-impedance leads as compared with the standard impedance lead group. There were no differences in battery impedance between both groups ( Figures 2 and 3 ).
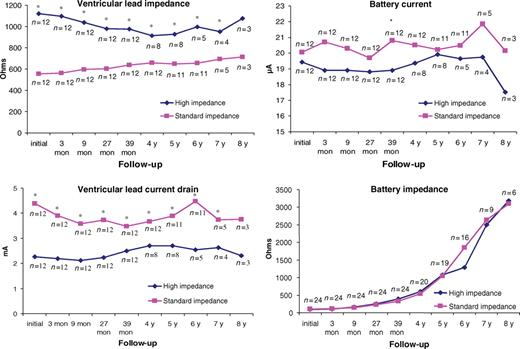
Ventricular lead impedance, ventricular lead current drain, battery current, and battery impedance during the follow-up period (per protocol population; * P < 0.05; n = number of patients).
In the intention-to-treat population, there was not significant difference between both groups with respect to estimated generator longevity during the whole follow-up period. The increase in estimated pacemaker longevity in the high-impedance lead group was significant for the first 6 years of follow-up in the per protocol population. But despite these initially promising results, even in the per protocol population there was finally no difference of actual pacemaker replacement time between the two groups. Pacemaker generators were replaced after 91.2 ± 10.3 months in the high-impedance lead group vs. 86.7 ± 6.8 months in the standard impedance lead group (difference 4.5 months; P = ns) ( Table 3 ).
Discussion
High-impedance pacing leads have been designed to increase pacemaker longevity by reducing current drain. Recently published studies displayed lower pacing threshold, 5 reduction of lead current drain, 1 , 3 and a consecutive increase of estimated generator longevity 4 , 7 using high-impedance leads as compared with standard impedance leads during a follow-up period of 1–3 years.
The present study was designed to prove these data and to determine the effects of high vs. standard impedance leads on actual pacemaker replacement time. Patients were followed until generator replacement, and actual pacemaker longevity was obtained. There were no differences with respect to pacing and sensing properties as well as lead-related complications between both groups. Despite the promising preliminary data, we did not find a significant increase in pacemaker longevity by using high-impedance ventricular leads over a maximum follow-up period of 8 years. Actual pacemaker longevity, calculated from implantation to replacement time due to elective replacement indicator, did not significantly differ between both groups. This result was surprising because, as determined by Ohm’s law ( I = V / R ), the use of high-impedance leads reduces current drain 8 and therefore reduces the amount of electrical current delivered during each pacing pulse.
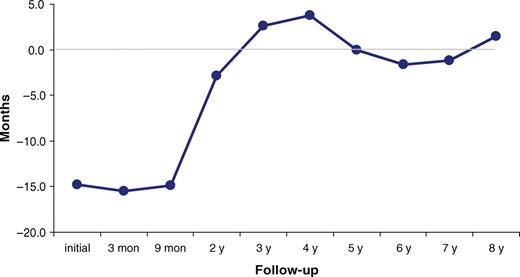
One reason for this finding may be the small number of patients who completed the follow-up in our study. As pacemakers were implanted in patients with a mean age of 73 years at the time of first pacemaker implantation, many of them died within the follow-up period. Starting with 40 patients, only 16 patients completed the 6 years follow-up (10 patients in the standard and 6 patients in the high-impedance lead group). Interestingly, the estimated pacemaker longevity was significantly increased in the high-impedance lead group at the 6 year follow-up. Nevertheless, there was no significant effect on actual replacement time between both groups. Most of the pacemakers were replaced 6–7 years after implantation. These results are in good correlation with a labelled estimated longevity of Kappa KDR 401 ® pacemakers in value of 6.4 years (∼77 months). The number of patients with a pacemaker replacement after that time dramatically decreased (at the 8 years follow-up only three patients remained in each group) and therefore statistical evaluation was not feasible. Another possible explanation for the missing effect of high-impedance leads on the actual pacemaker replacement interval may be an inaccurate calculation of the estimated battery longevity by the pacemaker itself. 10 The accuracy of the pacemaker algorithm for pacemaker longevity estimation is shown as the difference between minimal estimated vs. actual replacement time ( Figure 4 ). During the short-time follow-up after implantation, the pacemaker longevity estimation showed a shorter longevity as compared with actual replacement time. The accuracy of pacemaker longevity estimation increased after 2 years of follow-up with stable accuracy during the subsequent follow-up until pacemaker replacement. Furthermore, in our study, most pacemaker generator replacements took place a few months earlier than the estimated maximum replacement time was calculated because of safety reasons. Therefore, besides inaccurate calculation, earlier pacemaker replacement due to safety reasons may diminish the potential benefits of high-impedance leads.
Despite the fact that high-impedance leads showed a trend to a slight decrease in pacing impedance whereas the standard impedance lead group showed a trend to a slight increase of pacing impedance over the whole follow-up period, the difference between the two groups remained statistically significant.
Given the fact that only one half of the energy consumption of a modern pacemaker is actually due to pacing, whereas the other half is due to sensing as well as due to new auxiliary diagnostic tools (mode switching algorithms, algorithms for minimizing ventricular pacing, and storage of electrograms, etc.); 11 this may be an additional reason why high-impedance leads do not significantly contribute to increase the actual replacement time as compared with standard impedance leads. This underlines the importance of an individual optimization of pacemaker programming (e.g. deactivation of inappropriate diagnostic or therapeutic pacemaker tools).
Study limitations
Besides the use of high-impedance leads, automatic assessment of the pacing threshold shows an impact on pacemaker longevity. Therefore, this algorithm may contribute also to increase pacemaker longevity in patients with standard impedance ventricular pacing leads. 12
Conclusion
Our data suggest that high-impedance leads are as effective as standard impedance leads with respect to pacing and sensing as well as complication rates. Despite previously published data, we did not find a significant increase of actual pacemaker generator longevity in patients with high-impedance pacing leads as compared with standard impedance pacing leads.
Conflict of interest: F.H. has received lecture fees from Medtronic, St. Jude Medical, and Biotronik, and is serving on an advisory board for Boston Scientific. T.B. and M.S. received lecture fees from Biotronik. The other authors declare no conflicts of interest.
Funding
Dr K.E. was supported by a grant form the European Heart Rhythm Association (EHRA Training Fellowship) and by Österreichische National Bank Jubiläumsfond (Jubiläumsfondsprojekt Nr. 11183).



