-
PDF
- Split View
-
Views
-
Cite
Cite
Milos Kesek, Ablation procedures in Sweden during 2007: results from the Swedish Catheter Ablation Registry, EP Europace, Volume 11, Issue 2, February 2009, Pages 152–154, https://doi.org/10.1093/europace/eun298
Close - Share Icon Share
Abstract
Catheter ablation research is reported extensively. Much less is known about the clinical practice in the field. Study databases and surveys target selected populations. A general registry is needed to evaluate the actual results of routine catheter ablation. We present statistics from the Swedish Catheter Ablation Registry.
The registry is a nation-wide database collecting data from all the eight centres serving the country’s population of 9.18 million inhabitants. During each ablation procedure, the data are entered into a local database. On demand, the data are transferred to the central data management facility. The central SQL-database presently covers 7018 ablations performed in 5885 patients during 2004–07. In 2007, 2314 ablation procedures [521 for atrial fibrillation (AF)] were performed (252 ablations per million inhabitants and 57 AF procedures per million inhabitants). Mean procedure and fluoroscopy times ranked from 75 and 12 min, respectively, for atrioventricular junction ablation to 224 and 43 min, respectively, for AF ablation. The incidence of complications during 2007 was 1.8%. One death after a procedure for AF was reported, due to a cerebrovascular embolus.
The report presents prospective-gathered annual data from a nation-wide ablation register with voluntary participation. Several major complications have been reported, but the overall complication rate was low.
Introduction
Catheter ablation of arrhythmias is reported extensively in the scientific context. Much less is known about the clinical practice in the field. General conclusions about results and complications are often based on extrapolations from scientific study databases. Such efforts, however, reflect results from selected centres in limited populations and extrapolations may be affected by bias. There is therefore a need to evaluate data from procedures in routine populations. A few nation-wide registries collect such information. 1 An extrapolation of results among countries is subject to additional distortion due to differences in methods and indications, caused by differing local traditions and national health policies. This report reflects the current ablation practice in Sweden and offers a comparison with other published data.
Methods
Ablations are presently performed in eight Swedish public hospitals. Seven of the ablation centres are located in university hospitals, while one centre is situated in a large secondary hospital with complete cardiological and cardiothoracic services. The analysis is based on information collected in the Swedish Catheter Ablation Registry (see Appendix). In 2007, all the centres prospectively recorded data from individual procedures. The registry contains data from all the ablations performed in the country. The percentages of reported procedure and fluoroscopy times are low for three of the ablation substrates, because the major local database system presently does not collect the parameters in these groups. The annual data were analysed using the R statistical package, version 2.4.1 (R Foundation for Statistical Computing 2006).
Results
In 2007, 2314 ablation procedures were carried out. On average, 289 procedures per centre were performed (range 60–714). Five centres had annual rates exceeding 200 procedures per centre. The three most frequently targeted ablation substrates were atrioventricular nodal re-entry tachycardia (AVNRT, 25% of the annual volume), atrial fibrillation (AF, 23%, the procedures being performed in seven of the centres), and accessory pathway (AP, 19%) ( Figure 1 ). The patient demographics, procedure, and fluoroscopy times were collated ( Table 1 ). Primary success rates in ablations of AVNRT, AP, cavotricuspid isthmus-dependent atrial flutter (AFL), and ectopic atrial tachycardia/atrial macro-re- entry were noted ( Table 2 ).
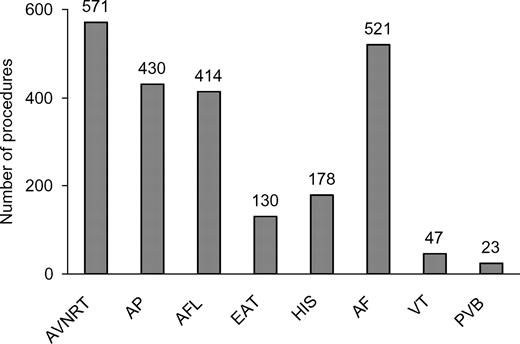
Number of ablations targeting the different substrates in Sweden, 2007. AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL); HIS, atrioventricular nodal ablation; AF, atrial fibrillation; VT, ventricular tachycardia; PVB, premature ventricular beats.
| . | Mean age (years) . | Men (%) . | Mean procedure duration (min) . | Based on (% of procedures) . | Mean fluoroscopy time (min) . | Based on (% of procedures) . |
|---|---|---|---|---|---|---|
| AVNRT | 50 ± 17 | 36 | 122 ± 51 | 99 | 16 ± 13 | 99 |
| AP | 38 ± 19 | 65 | 139 ± 64 | 98 | 24 ± 19 | 98 |
| AFL | 59 ± 12 | 79 | 128 ± 53 | 98 | 23 ± 16 | 99 |
| EAT | 51 ± 17 | 48 | 199 ± 72 | 100 | 27 ± 19 | 99 |
| HIS | 70 ± 8 | 58 | 75 ± 40 | 44 | 12 ± 12 | 44 |
| AF | 56 ± 10 | 77 | 224 ± 68 | 98 | 43 ± 20 | 99 |
| VT | 48 ± 19 | 62 | 219 ± 96 | 40 | 42 ± 35 | 40 |
| PVB | 49 ± 12 | 22 | 187 ± 84 | 35 | 32 ± 20 | 35 |
| . | Mean age (years) . | Men (%) . | Mean procedure duration (min) . | Based on (% of procedures) . | Mean fluoroscopy time (min) . | Based on (% of procedures) . |
|---|---|---|---|---|---|---|
| AVNRT | 50 ± 17 | 36 | 122 ± 51 | 99 | 16 ± 13 | 99 |
| AP | 38 ± 19 | 65 | 139 ± 64 | 98 | 24 ± 19 | 98 |
| AFL | 59 ± 12 | 79 | 128 ± 53 | 98 | 23 ± 16 | 99 |
| EAT | 51 ± 17 | 48 | 199 ± 72 | 100 | 27 ± 19 | 99 |
| HIS | 70 ± 8 | 58 | 75 ± 40 | 44 | 12 ± 12 | 44 |
| AF | 56 ± 10 | 77 | 224 ± 68 | 98 | 43 ± 20 | 99 |
| VT | 48 ± 19 | 62 | 219 ± 96 | 40 | 42 ± 35 | 40 |
| PVB | 49 ± 12 | 22 | 187 ± 84 | 35 | 32 ± 20 | 35 |
AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL); HIS, atrioventricular nodal ablation; AF, atrial fibrillation; VT, ventricular tachycardia; PVB, premature ventricular beats.
| . | Mean age (years) . | Men (%) . | Mean procedure duration (min) . | Based on (% of procedures) . | Mean fluoroscopy time (min) . | Based on (% of procedures) . |
|---|---|---|---|---|---|---|
| AVNRT | 50 ± 17 | 36 | 122 ± 51 | 99 | 16 ± 13 | 99 |
| AP | 38 ± 19 | 65 | 139 ± 64 | 98 | 24 ± 19 | 98 |
| AFL | 59 ± 12 | 79 | 128 ± 53 | 98 | 23 ± 16 | 99 |
| EAT | 51 ± 17 | 48 | 199 ± 72 | 100 | 27 ± 19 | 99 |
| HIS | 70 ± 8 | 58 | 75 ± 40 | 44 | 12 ± 12 | 44 |
| AF | 56 ± 10 | 77 | 224 ± 68 | 98 | 43 ± 20 | 99 |
| VT | 48 ± 19 | 62 | 219 ± 96 | 40 | 42 ± 35 | 40 |
| PVB | 49 ± 12 | 22 | 187 ± 84 | 35 | 32 ± 20 | 35 |
| . | Mean age (years) . | Men (%) . | Mean procedure duration (min) . | Based on (% of procedures) . | Mean fluoroscopy time (min) . | Based on (% of procedures) . |
|---|---|---|---|---|---|---|
| AVNRT | 50 ± 17 | 36 | 122 ± 51 | 99 | 16 ± 13 | 99 |
| AP | 38 ± 19 | 65 | 139 ± 64 | 98 | 24 ± 19 | 98 |
| AFL | 59 ± 12 | 79 | 128 ± 53 | 98 | 23 ± 16 | 99 |
| EAT | 51 ± 17 | 48 | 199 ± 72 | 100 | 27 ± 19 | 99 |
| HIS | 70 ± 8 | 58 | 75 ± 40 | 44 | 12 ± 12 | 44 |
| AF | 56 ± 10 | 77 | 224 ± 68 | 98 | 43 ± 20 | 99 |
| VT | 48 ± 19 | 62 | 219 ± 96 | 40 | 42 ± 35 | 40 |
| PVB | 49 ± 12 | 22 | 187 ± 84 | 35 | 32 ± 20 | 35 |
AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL); HIS, atrioventricular nodal ablation; AF, atrial fibrillation; VT, ventricular tachycardia; PVB, premature ventricular beats.
| . | Primary success (% of procedures) . | Based on (% of procedures) . |
|---|---|---|
| AVNRT | 96 | 100 |
| AP | 89 | 99 |
| AFL | 87 | 50 |
| EAT | 71 | 98 |
| . | Primary success (% of procedures) . | Based on (% of procedures) . |
|---|---|---|
| AVNRT | 96 | 100 |
| AP | 89 | 99 |
| AFL | 87 | 50 |
| EAT | 71 | 98 |
AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL).
| . | Primary success (% of procedures) . | Based on (% of procedures) . |
|---|---|---|
| AVNRT | 96 | 100 |
| AP | 89 | 99 |
| AFL | 87 | 50 |
| EAT | 71 | 98 |
| . | Primary success (% of procedures) . | Based on (% of procedures) . |
|---|---|---|
| AVNRT | 96 | 100 |
| AP | 89 | 99 |
| AFL | 87 | 50 |
| EAT | 71 | 98 |
AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL).
The rates are reported in the subgroups with a verifiable ablation endpoint (non-inducibility, absence of AP, and bi- directional isthmus conduction block). Forty-one complications (periprocedural, as well as late) have been reported ( Table 3 ). The overall complication rate was 1.8% (2.9% for AF procedures and 1.4% for the other procedure types). One death occurred, due to a cerebrovascular embolus, in a 55-year-old man with paroxysmal AF. A 68-year-old man had damage to the aortic valve, which was detected late after a left-sided atrioventricular nodal ablation by retrograde catheterization.
Number of complications and the complication rate for the different substrates
| . | AVNRT . | AP . | AFL . | EAT . | HIS . | AF . | VT . | PVB . | Total . |
|---|---|---|---|---|---|---|---|---|---|
| AV block, requiring pacemaker | 1 | 1 | 2 | ||||||
| AV block, temporary | 5 | 1 | 6 | ||||||
| Pericardial effusion | 1 | 2 | 2 | 5 | |||||
| Tamponade | 1 | 1 | 1 | 3 | |||||
| Pneumothorax | 1 | 1 | |||||||
| Bleeding requiring therapy | 2 | 1 | 1 | 1 | 1 | 9 | 1 | 16 | |
| Valve damage | 1 | 1 | |||||||
| Pulmonary embolus | 1 | 1 | |||||||
| Cerebral embolus | 1 | 1 | |||||||
| Pseudoaneurysm | 1 | 1 | 1 | 2 | 5 | ||||
| Total | 10 | 5 | 3 | 2 | 3 | 15 | 3 | 0 | 41 |
| Complication rate (%) | 1.8 | 1.2 | 0.7 | 1.5 | 1.7 | 2.9 | 6.4 | 0 | 1.8 |
| . | AVNRT . | AP . | AFL . | EAT . | HIS . | AF . | VT . | PVB . | Total . |
|---|---|---|---|---|---|---|---|---|---|
| AV block, requiring pacemaker | 1 | 1 | 2 | ||||||
| AV block, temporary | 5 | 1 | 6 | ||||||
| Pericardial effusion | 1 | 2 | 2 | 5 | |||||
| Tamponade | 1 | 1 | 1 | 3 | |||||
| Pneumothorax | 1 | 1 | |||||||
| Bleeding requiring therapy | 2 | 1 | 1 | 1 | 1 | 9 | 1 | 16 | |
| Valve damage | 1 | 1 | |||||||
| Pulmonary embolus | 1 | 1 | |||||||
| Cerebral embolus | 1 | 1 | |||||||
| Pseudoaneurysm | 1 | 1 | 1 | 2 | 5 | ||||
| Total | 10 | 5 | 3 | 2 | 3 | 15 | 3 | 0 | 41 |
| Complication rate (%) | 1.8 | 1.2 | 0.7 | 1.5 | 1.7 | 2.9 | 6.4 | 0 | 1.8 |
AV, atrioventricular; AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL); HIS, atrioventricular nodal ablation; AF, atrial fibrillation; VT, ventricular tachycardia; PVB, premature ventricular beats.
Number of complications and the complication rate for the different substrates
| . | AVNRT . | AP . | AFL . | EAT . | HIS . | AF . | VT . | PVB . | Total . |
|---|---|---|---|---|---|---|---|---|---|
| AV block, requiring pacemaker | 1 | 1 | 2 | ||||||
| AV block, temporary | 5 | 1 | 6 | ||||||
| Pericardial effusion | 1 | 2 | 2 | 5 | |||||
| Tamponade | 1 | 1 | 1 | 3 | |||||
| Pneumothorax | 1 | 1 | |||||||
| Bleeding requiring therapy | 2 | 1 | 1 | 1 | 1 | 9 | 1 | 16 | |
| Valve damage | 1 | 1 | |||||||
| Pulmonary embolus | 1 | 1 | |||||||
| Cerebral embolus | 1 | 1 | |||||||
| Pseudoaneurysm | 1 | 1 | 1 | 2 | 5 | ||||
| Total | 10 | 5 | 3 | 2 | 3 | 15 | 3 | 0 | 41 |
| Complication rate (%) | 1.8 | 1.2 | 0.7 | 1.5 | 1.7 | 2.9 | 6.4 | 0 | 1.8 |
| . | AVNRT . | AP . | AFL . | EAT . | HIS . | AF . | VT . | PVB . | Total . |
|---|---|---|---|---|---|---|---|---|---|
| AV block, requiring pacemaker | 1 | 1 | 2 | ||||||
| AV block, temporary | 5 | 1 | 6 | ||||||
| Pericardial effusion | 1 | 2 | 2 | 5 | |||||
| Tamponade | 1 | 1 | 1 | 3 | |||||
| Pneumothorax | 1 | 1 | |||||||
| Bleeding requiring therapy | 2 | 1 | 1 | 1 | 1 | 9 | 1 | 16 | |
| Valve damage | 1 | 1 | |||||||
| Pulmonary embolus | 1 | 1 | |||||||
| Cerebral embolus | 1 | 1 | |||||||
| Pseudoaneurysm | 1 | 1 | 1 | 2 | 5 | ||||
| Total | 10 | 5 | 3 | 2 | 3 | 15 | 3 | 0 | 41 |
| Complication rate (%) | 1.8 | 1.2 | 0.7 | 1.5 | 1.7 | 2.9 | 6.4 | 0 | 1.8 |
AV, atrioventricular; AVNRT, atrioventricular nodal re-entry tachycardia; AP, accessory pathway; AFL, cavotricuspid isthmus-dependent atrial flutter; EAT, ectopic atrial tachycardia/atrial macro-re-entry (other than AFL); HIS, atrioventricular nodal ablation; AF, atrial fibrillation; VT, ventricular tachycardia; PVB, premature ventricular beats.
Discussion
The number of Swedish ablations ( Figure 1 ) corresponds to 252 ablations per million inhabitants and 57 AF procedures per million inhabitants during 2007. This is higher than the Spanish rate of 158 ablations per million inhabitants in 2006 and similar to the Italian rate of 251 ablations per million inhabitants in 2005. 1–3 The latter must, however, be interpreted in view of the fact that a single centre (San Raffaele, Milano, Italy) stood for 38% of the Italian ablation volume that year.
The absolute number of centres in Sweden, which perform over 200 ablations per year, is comparable with Spain (five vs. seven). The primary success percentages for AVNRT, AP, and AFL in Sweden are slightly lower than the reported Spanish figures (96 vs. 98%, 89 vs. 92%, and 87 vs. 96%). 1 The incidence of complications is low. Among those is, however, one fatality and several other potentially life-threatening conditions. In a worldwide survey of AF ablations, the incidence of periprocedural death was 0.05%. 4 Aortic valve damage has previously been described in 1.9% of ablations done by the retrograde approach. 5
Atrial fibrillation procedures have a higher complication rate than the other procedure types. This finding is similar to other published data. The Spanish Registry for 2006 reported 1.4% complications in all ablations and 5.1% complications in AF procedures. 1 The German Atrial Fibrillation Competence Network reported 2.4% major complications in AF procedures during 2006–07. 6
The validity of the data from the registry depends on the degree of registry coverage and the uniformity of local coding policy. Voluntary participation will limit the reliability, if centres with lower success and higher complication rates do not join the registry. A compulsory registry guarantees a high coverage, but the quality of the data can be questioned. Participation in the Swedish Catheter Ablation Registry is voluntary, but promoted by the public health authorities. The few centres involved have agreed on the basic data registration and the registry has 100% geographical coverage. The information entered in the local databases is used in the generation of the compulsory catheterization report required for the routine patient casebook. This ensures that at least the basic demographical information from each procedure will ultimately be registered in the central database. The uniformity of coding depends on common definitions and the possibility of monitoring the adherence. Common coding definitions are currently being specified. The two local database systems were, however, originally not constructed for a co-ordinated central data collection and the local data must be translated. For procedure and fluoroscopy times, the process is simple. The definition of primary success is more complicated and we only report by procedure types with commonly agreed endpoints. Evaluation of complications is complex. Complications occurring during the intervention will be registered. The coverage of problems appearing at a later stage is, however, uncertain. The complication history is a collection of case reports and the reported rates ( Table 3 ) have somewhat limited reliability. We cannot presently estimate whether the absence of reported late complications signifies uncomplicated intervention or merely lack of follow-up.
Acknowledgements
Technical assistance with database issues was provided by Lars Bergman, Sigma, Göteborg, Sweden. The underlying data is the property of the steering committee of the Swedish Catheter Ablation Registry, presently: Birgitta Johansson, Lennart Bergfeldt (Göteborg); Erik Ljungström (Karlskrona); Anders Jönsson, Håkan Walfridsson (Linköping); Ole Kongstad, Eva Hertevig (Lund); Göran Kennebäck, Jonas Schwieler (Stockholm); Milos Kesek, Steen Jensen (Umeå); Carina Blomström-Lundqvist, Stefan Lönnerholm (Uppsala); Peter Linde, Henrik Almroth (Örebro). The contribution of the individual centres to the registry is gratefully acknowledged.
Conflict of interest: none declared.
Appendix
The Swedish Catheter Ablation Registry is a nation-wide database collecting data from all the eight centres for invasive electrocardiology serving the country’s population of 9.18 million inhabitants. Decisions are taken by a steering committee with representatives from the centres, headed by a registry chairman. The registry is presently funded by the Swedish Association of Local Authorities and Regions, on the base of an annual application. The registry reports in Swedish are available for public download at the registry website ( www.ablationsregistret.se ).
During each investigation, the data are entered on-site into a database. Two types of local databases are presently in use. On demand, the data are transferred to the central data management facility. The central SQL-database presently covers 7018 ablation procedures performed in 5885 patients during 2004–07. The stored information contains demographic data, diagnosis, procedure data such as skin-to-skin and radiation times, catheter data, primary success according to the operator, and complications. For 2007, data from all Swedish catheter ablation procedures are available (however, with varying completeness with respect to individual parameters). The data are de-identified with respect to the centres. All the cases in the database are identifiable. The Swedish health authorities have an intention of opening the registry data from individual centres to the public. Such policy may decrease the willingness to deliver data to a voluntary system and, in case of a compulsory system, result in unreliable data.



