-
PDF
- Split View
-
Views
-
Cite
Cite
Fernando Yue Cesena, Metabolic syndrome and premature atherosclerotic cardiovascular disease: insights for the individual and the population, European Journal of Preventive Cardiology, Volume 31, Issue 10, August 2024, Pages 1301–1302, https://doi.org/10.1093/eurjpc/zwae139
Close - Share Icon Share
This editorial refers to ‘Association between cumulative metabolic risk exposure and cardiovascular disease: a nationwide cohort of over 3.6 million young adults’, by H. Lee et al., https://doi.org/10.1093/eurjpc/zwae088.
The association between metabolic syndrome (MetS) and atherosclerotic cardiovascular disease (ASCVD) has been firmly established by several epidemiological studies worldwide.1 These observations have largely focused on middle-aged and older adults. This edition of the European Journal of Preventive Cardiology publishes a robust study by Lee et al.2 from South Korea that extends this knowledge to younger persons.
This retrospective study impresses with its numbers: it included a very large, nationwide-based sample of more than 3 million adults under 40 years, among whom more than 19 000 ASCVD events (myocardial infarction or ischaemic stroke) were recorded after a median follow-up of 7.7 years. At baseline, the participants were categorized into four groups according to the presence or absence of MetS at two points separated by a 2-year interval: MetS-free (no MetS at either assessment), MetS-developed (MetS only at the second examination), MetS-recovered (MetS only at the first moment), and MetS-persistent (MetS at both evaluations). Compared with the MetS-free group, MetS-persistent participants had an almost two-fold increase in incident ASCVD events, whereas Met-developed and MetS-recovered groups had an intermediate incidence rate. Notably, each component of the MetS was independently associated with ASCVD incidence in multivariable analyses, with stronger associations for elevated blood pressure. The authors conclude that cumulative exposure to metabolic factors, especially high blood pressure, increases cardiovascular disease (CVD) incidence in young adults.2
Relevant aspects regarding the characteristics of the study population deserve comments. Firstly, MetS prevalence was low (∼10%)2 compared with many other countries. In the USA, for instance, MetS prevalence among those aged 20–39 years was estimated to be 21% in 2015–16.3 Secondly, the mean total cholesterol plasma level was 4.84 mmol/L (187 mg/dL),2 which is very similar to the median age-standardized total cholesterol concentration in Europe [4.92 mmol/L (190 mg/dL) in females and 4.82 mmol/L (186 mg/dL) in males], although variations between European countries do exist.4 Thirdly, a very high prevalence rate of smoking was observed in the South Korean population (from 30% in the MetS-free to 55% in the MetS-persistent group),2 contrasting to the median rate of 22% in Europe, although there is a large heterogeneity across countries (from 8% in Iceland to 41% in Bosnia and Herzegovina).4
According to the Global Burden of Disease (GBD) study, CVD was the leading cause of death among persons aged 15–49 years in the world and the European Region.5 Premature ASCVD can be catastrophic for families, leading to a loss of workforce productivity and an increased burden on the health system. Since ASCVD is largely preventable, efforts to effectively stratify the risk and thereby implement preventive measures are warranted, even among younger individuals. In particular, ASCVD risk stratification could inform the potential benefits of lipid-lowering therapy, a frequent matter of debate in this age group.
Individuals younger than 40 years are typically considered to be at low risk for an ASCVD event. Indeed, in the study by Lee et al.,2 the ASCVD incidence rate was low, even among the highest risk group (<2 per 1000 person-years in the MetS-persistent category). Young people often perceive their risk as low despite having risk factors. Guidelines recommend the use of 10-year ASCVD risk scores in primary prevention for people aged 40+ years.6 The 2021 ESC Guidelines on CVD prevention in clinical practice established lower 10-year risk thresholds for classifying younger individuals into higher-risk categories, consequently increasing the likelihood of those aged 40–55 years being prescribed a lipid-lowering medication.6 Conversely, clear guidance for risk assessment and management in people younger than 40 years is lacking.
Some strategies for assessing ASCVD risk in young people have been proposed, including the use of long-term or lifetime CVD risk scores,7 or expressing the risk percentile for age and sex,8 similar to what is reported in coronary artery calcification (CAC) examinations. These approaches have the potential to raise risk awareness and increase treatment adherence. However, the thresholds for defining a high-risk status, as well as how to use these methods in clinical decision-making, have not been established. Referring younger persons thought to be at higher risk for CAC evaluation is another attractive strategy. Indeed, CAC score has been linked to cardiovascular events and even mortality in individuals aged <55 years at primary prevention.9 Additionally, the promising role of polygenic risk scores in refining ASCVD risk stratification in young persons is a subject of intense investigation.10
At the population level, it is clear enough that reducing MetS rates is a major contemporary health challenge. A huge progress in decreasing rates of tobacco use and associated deaths was achieved in several parts of the world, although this is still a concern in many low- and middle-income countries.11,12 Blood pressure and LDL cholesterol (LDL-c) levels can be now controlled in the majority of individuals with the available therapeutic armamentarium. Prevalence rates of elevated blood pressure and plasma levels of total cholesterol have declined in Europe over recent decades, driven by more favourable trends in high-income countries.4 In contrast, population rates of obesity and diabetes mellitus are escalating globally.4,13
Mortality rates due to CVD among individuals aged 15–49 years in 1990 were comparable in the world [36.58 (34.89–38.43)] and in Europe [37.46 (36.97–37.98) deaths per 100 000 inhabitants], according to the GBD 2019 study.5 Since then, these rates have declined both globally and in Europe, reflecting improvements in risk factor management, healthcare access, and treatment advancements. However, a detailed analysis reveals that while CVD deaths attributable to high systolic blood pressure, elevated LDL-c, and tobacco use trended downward, those attributable to high plasma glucose and weight excess have increased in recent decades in the world (Figure 1). Similarly, in Europe, CVD deaths attributable to high plasma glucose and high body mass index have decreased to a lesser extent compared with those attributable to other risk factors (Figure 1). Therefore, reducing rates of obesity and diabetes, closely related to MetS, is a major priority that requires global efforts. Campaigns to enhance awareness of the CVD risk associated with MetS, among both the community and healthcare professionals, and programmes to engage the population in a healthy lifestyle and facilitate access to weight loss medications are crucial but probably not enough. Other more energetic interventions involving government choices and regulatory actions, such as taxation and restrictions on advertising unhealthy products, should be strongly considered to increase the chances of success.
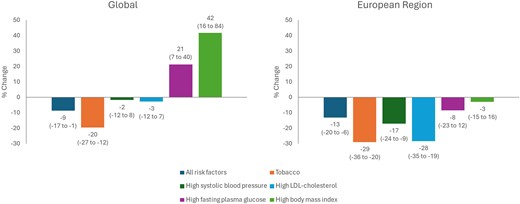
Trends in mortality rates due to cardiovascular disease in young adults. Per cent changes in mortality rates (deaths per 100 000 inhabitants) due to cardiovascular disease attributable to different risk factors in individuals aged 15–49 years from 1990 to 2019 in the world and the European Region (as defined by the World Health Organization). Numbers in parentheses refer to the 95% uncertainty interval. Source: Global Burden of Disease Study 2019.5
In conclusion, the study by Lee et al. reinforces the relevance of the relationship between MetS and ASCVD, with the novelty of clearly demonstrating this association in individuals younger than 40 years. The findings support both individual- and population-level initiatives to control MetS components, mainly focusing on limiting adipose tissue accumulation. Furthermore, clearer guideline recommendations for stratifying ASCVD risk and implement preventive measures in persons younger than 40 years are strongly advisable to improve outcomes in this age group.
References
Author notes
The opinions expressed in this article are not necessarily those of the Editors of the European Journal of Preventive Cardiology or of the European Society of Cardiology.
Conflict of interest: none declared.




Comments