-
PDF
- Split View
-
Views
-
Cite
Cite
Yoshihiro Fukumoto, Beta-blocker in preserved left ventricular ejection fraction with elevated serum vitamin A concentrations, European Journal of Preventive Cardiology, Volume 28, Issue 17, December 2021, Pages 1895–1896, https://doi.org/10.1093/eurjpc/zwab009
Close - Share Icon Share
This editorial refers to ‘β-Blocker use and risk of all-cause mortality in patients with coronary heart disease: effect modification by serum vitamin A’ by I. Dhar et al., pp. 1897–1902.
Coronary artery diseases (CADs) are based on coronary atherosclerosis, which begins with endothelial dysfunction and develops with inflammatory responses in the arterial walls. 1,2 In the coronary atherosclerotic progression, various risk factors are involved, such as life-style diseases, type A character, unfavourable food intake, smoking, and low exercise habits.2,3 To prevent major cardiovascular (CV) events in patients with CADs, we have performed diet therapy, exercise training, and optimal medical therapy in daily practice. Myocardial infarction, one of the major CV events, is caused by a coronary obstruction in CADs, which is a leading cause of heart failure.4,5 In patients with a history of myocardial infarction and reduced left ventricular ejection fraction, beta-blockers are recommended to prevent cardiac death.5,6 Actually, it is well known that beta-blockers reduce mortality and morbidity in symptomatic patients with heart failure with reduced ejection fraction (HFrEF),6 in whom beta-blockers should be initiated in clinically stable state, starting at a low dose and gradually up-titrated to the maximum tolerated dose.6 However, beta-blockers do not improve mortality and morbidity in patients with heart failure with preserved ejection fraction (HFpEF).6
Dhar et al.7 have hypothesized that vitamin A status modified the association of beta-blocker use with the risk of all-cause mortality in patients undergoing coronary angiography for suspected CADs in the large prospective study. In this article, among the vast majority with preserved left ventricular systolic function, the use of beta-blockers at discharge was associated with improved survival primarily among patients with elevated vitamin A concentration, even after extensive adjustment for traditional CV disease risk factors, and potential confounders.7 One of the most important findings in the present study was that beta-blockers were effective in preserved left ventricular ejection fraction with high serum levels of vitamin A. Further, most of the enrolled patients in this study had no history of heart failure, suggesting stage B heart failure classification.7 It might be highly possible that there would be a beneficial effect of beta-blocker use on survival, also in stage C HFpEF patients with elevated vitamin A concentrations.
As explained in the current issue,7 vitamin A as retinol is a fat-soluble micronutrient generally obtained from the diet either as pro-vitamin A carotenoids from plant foods or retinyl esters from animal foods and is essential for diverse physiological functions.8 Although vitamin A deficiency is a big problem of high mortality, illness, lung development, and blindness in children,9,10 too much intake of vitamin A (sometimes supplement) may increase cardiovascular risks because vitamin A is fat-soluble.11,12 If patients with elevated vitamin A concentrations take the supplements, we should recommend them to stop. However, it has been also reported that higher serum levels of retinoic acid were associated with a lower risk of mortality in patients with CADs.13 Thus, the association between vitamin A levels and CV mortality is still controversial.
Although angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB), mineral-corticoid receptor antagonists (MRA) have failed to reduce mortality in non-selected patients with HFpEF,6 beta-blockers might be a good therapeutic option in selected HFpEF patients with elevated vitamin A serum levels. Similarly, ACEi, ARB, and MRA might be possibly effective in some specific subgroups of HFpEF patients. Currently, in order to develop order-made medical therapy in CV diseases, beta-blockers seem to be effective in HFpEF patients with high concentrations of vitamin A (Figure 1).
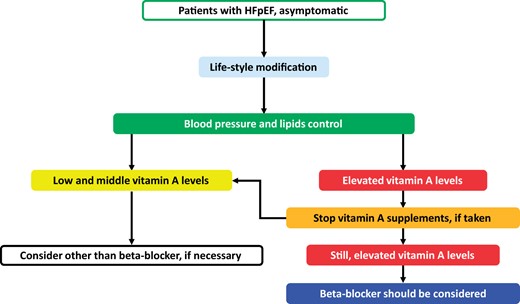
Beneficial beta-blockers in patients with asymptomatic preserved left ventricular ejection fraction. Patients with cardiovascular diseases need life-style modification, including food intake and exercise, and blood pressure and lipid control. If serum levels of vitamin A are elevated, beta-blockers have a beneficial effect on all-cause mortality. HFpEF, heart failure with preserved ejection fraction.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal Preventive Cardiology or of the European Society of Cardiology.




Comments