
Cover image
How to diagnose heart failure with preserved ejection fraction: the HFA–PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC)
Burkert Pieske1,2,3,4*, Carsten Tschöpe1,2,5, Rudolf A. de Boer6, Alan G. Fraser7, Stefan D. Anker1,2,5,8, Erwan Donal9, Frank Edelmann1,2, Michael Fu10, Marco Guazzi11,12, Carolyn S.P. Lam13,14, Patrizio Lancellotti15, Vojtech Melenovsky16, Daniel A. Morris1, Eike Nagel 17,18, Elisabeth Pieske-Kraigher1, Piotr Ponikowski19, Scott D. Solomon20, Ramachandran S. Vasan21, Frans H. Rutten 22, Adriaan A. Voors6, Frank Ruschitzka23, Walter J. Paulus24, Petar Seferovic25, and Gerasimos Filippatos26,27
1Department of Internal Medicine and Cardiology, Charité - Universitätsmedizin Berlin, Campus Virchow Klinikum; 2German Center for Cardiovascular Research (DZHK), Berlin, Partner Site, Germany; 3Department of Internal Medicine and Cardiology, German Heart Institute, Berlin, Germany; 4Berlin Institute of Health (BIH), Germany; 5Berlin Institute of Health (BIH) Center for Regenerative Therapies (BCRT), Charite, Berlin, Germany; 6University Medical Centre Groningen, University of Groningen, Department of Cardiology, Groningen, the Netherlands; 7School of Medicine, Cardiff University, Cardiff, UK; 8Department of Cardiology and Pneumology, University Medicine Göttingen (UMG), Germany; 9Cardiology and CIC, IT1414, CHU de Rennes LTSI, Université Rennes-1, INSERM 1099, Rennes, France; 10Section of Cardiology, Department of Medicine, Sahlgrenska University Hosptal/Ostra, Göteborg, Sweden; 11Department of Biomedical Sciences for Health, University of Milan, IRCCS, Milan, Italy; 12Department of Cardiology, IRCCS Policlinico, San Donato Milanese, Milan, Italy, 13National Heart Centre, Singapore & Duke-National University of Singapore; 14University Medical Centre Groningen, The Netherlands; 15Department of Cardiology, Heart Valve Clinic, University of Liège Hospital, GIGA Cardiovascular Sciences, CHU Sart Tilman, Liège, Belgium; 16Institute for Clinical and Experimental Medicine - IKEM, Prague, Czech Republic; 17Institute for Experimental and Translational Cardiovascular Imaging, University Hospital Frankfurt; 18German Centre for Cardiovascular Research (DZHK), Partner Site Frankfurt, Germany; 19Medical University, Clinical Military Hospital, Wroclaw, Poland; 20Cardiovascular Division, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA; 21Section of Preventive Medicine and Epidemiology and Cardiovascular Medicine, Department of Medicine, Boston University School of Medicine, Boston, MA, USA; 22Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands; 23University Heart Centre, University Hospital Zurich, Switzerland; 24Department of Physiology and Amsterdam Cardiovascular Sciences, Amsterdam University Medical Center, The Netherlands; 25University of Belgrade School of Medicine, Belgrade University Medical Center, Serbia; 26Department of Cardiology, National and Kapodistrian University of Athens Medical School; University Hospital “Attikon”, Athens, Greece; and 27University of Cyprus, School of Medicine, Nicosia, Cyprus
* Corresponding author. Tel: +49 30 450 553702, Fax: +49 30 450 7 553702, Email: [email protected]
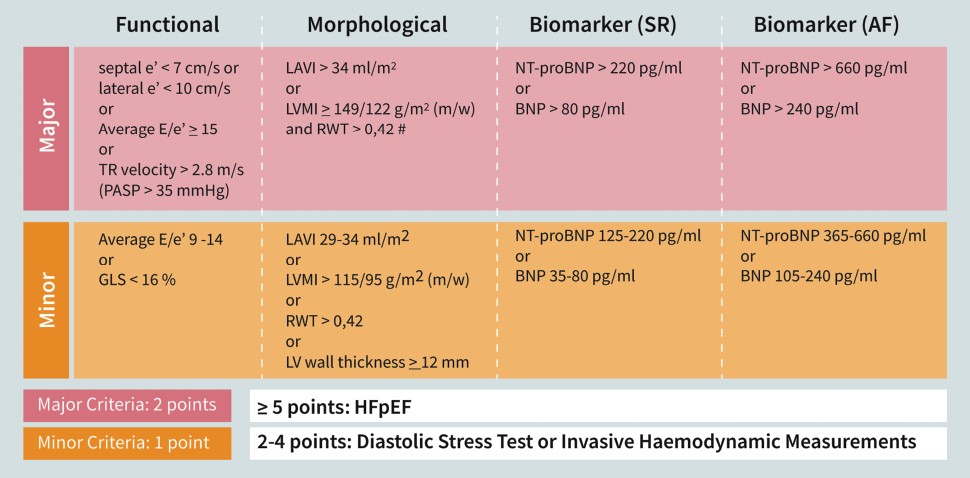
Making a firm diagnosis of chronic heart failure with preserved ejection fraction (HFpEF) remains a challenge. We recommend a new stepwise diagnostic process, the ‘HFA–PEFF diagnostic algorithm’. Step 1 (P=Pre-test assessment) is typically performed in the ambulatory setting and includes assessment for HF symptoms and signs, typical clinical demographics (obesity, hypertension, diabetes mellitus, elderly, atrial fibrillation), and diagnostic laboratory tests, electrocardiogram, and echocardiography. In the absence of overt non-cardiac causes of breathlessness, HFpEF can be suspected if there is a normal left ventricular ejection fraction, no significant heart valve disease or cardiac ischaemia, and at least one typical risk factor. Elevated natriuretic peptides support, but normal levels do not exclude a diagnosis of HFpEF. The second step (E: Echocardiography and Natriuretic Peptide Score) requires comprehensive echocardiography and is typically performed by a cardiologist. Measures include mitral annular early diastolic velocity (e′), left ventricular (LV) filling pressure estimated using E/e′, left atrial volume index, LV mass index, LV relative wall thickness, tricuspid regurgitation velocity, LV global longitudinal systolic strain, and serum natriuretic peptide levels. Major (2 points) and Minor (1 point) criteria were defined from these measures. A score ≥5 points implies definite HFpEF; ≤1 point makes HFpEF unlikely. An intermediate score (2–4 points) implies diagnostic uncertainty, in which case Step 3 (F1: Functional testing) is recommended with echocardiographic or invasive haemodynamic exercise stress tests. Step 4 (F2: Final aetiology) is recommended to establish a possible specific cause of HFpEF or alternative explanations. Further research is needed for a better classification of HFpEF.
Keywords Heart failure • HFpEF • diagnosis • echocardiography • biomarkers • natriuretic peptides • exercise echocardiography
Figure 3 Step 2 (E): Echocardiographic and natriuretic peptide heart failure with preserved ejection fraction workup and scoring system (diagnostic workup).






