
Cover image
Quadricuspid mitral valve: a rare phenotype associated with hypertrophic cardiomyopathy
Marissa L. Kauss1, William Miranda2, Lawrence J. Sinak2, and Hector I. Michelena2*
1Department of Cardiovascular Anesthesia, Mayo Clinic, 200 First Street SW, Rochester, MN, 55905, USA; and Department of Cardiovascular Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN, 55905, USA
* Corresponding author. Tel: +1 507266 1376, Fax: +1 507538 6915, Email: [email protected]
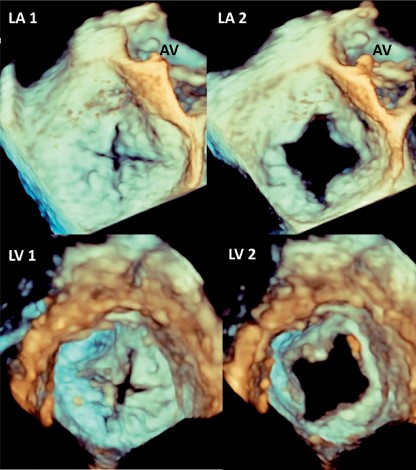
A 63-year-old man with hypertrophic obstructive cardiomyopathy (HOCM) and progressive dyspnoea presented for surgical evaluation. Transthoracic echocardiography showed asymmetric septal hypertrophy, peak dynamic left ventricular outflow tract gradient of 100 mmHg, systolic anterior motion of the mitral apparatus (SAM), and severe mitral regurgitation. Pre-surgical cine balanced steady state free precession MRI showed SAM and centrally-directed mitral regurgitation [Panel MR1 (double arrows), Supplementary material online, Video S1], as well as abnormal papillary muscle structure (see Supplementary material online, Video S2) with likely four separate papillary muscles, and a square-like appearing mitral opening in diastole (Panel MR2, Supplementary material online, Video S2). Pre-bypass 3D intraoperative transoesophageal echocardiography demonstrated a quadricuspid mitral valve [Panels LA1 (atrial systolic view), LA2 (atrial diastolic view), LV1 (ventricle systolic view), LV2 (ventricle diastolic view), Supplementary material online, Video S3 and S4]. All four leaflets were of relatively equal dimension and fully mobile without prolapse. Residual regurgitation after myectomy was mild-moderate with unchanged central jet, and no valvular intervention was required.
Although the presence of deep clefts could explain the findings, the papillary muscle anatomy suggests that four independent leaflets (one small anterior, one small posterior, and two commissural leaflets) may be present in this patient. As we have previously reported in trileaflet-appearing mitral valves associated with HOCM, the regurgitation jet was atypical (not posterior), and most of it resolved after myectomy. This highlights the importance of immediate post-bypass mitral regurgitation assessment after septal myectomy, before considering further interventions. Intra-operative 3D transoesophageal echocardiography and cardiac MRI were instrumental in identification of these abnormalities.
Supplementary material is available at European Heart Journal online.






