-
PDF
- Split View
-
Views
-
Cite
Cite
F Pietrantonio, E Alessi, M Pascucci, M Delli Castelli, R D'Amico, M Ronchetti, Innovation in health care: continuous wireless monitoring to improve management of critically ill atients: LIMS study preliminary results, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.3482, https://doi.org/10.1093/ehjci/ehaa946.3482
Close - Share Icon Share
Abstract
Wireless vital parameter continuous monitoring (WVPCM) is compared to regular nurse monitoring in order to provide data on the clinical and economic impact of critically ill patients (CIPs) in Internal Medicine Units (IMU).
Pilot prospective randomized controlled open-label multi-center study with WIN@Hospital wearable wireless system creating alerts on portable devices (ipad). Experimental Arm: CIPs with MEWS (Modified Early Warning Score) ≥3 and/or NEWS (National Early Warning Score) ≥5 at admission underwent WCPCM over the first 72 h. Active Comparator: CIPs with MEWS ≥3 and/or NEWS ≥5 at admission undergoing regular nurse monitoring.
Primary outcomes: Reduction of major complications (MC) from 15% to 5%. Secondary outcomes: One day reduction in length of stay (LOS); reduced nurse monitoring time; accurate patient stratification and definition of end stage disease.
Preliminary results: Enrolled 145 and evaluable 125 patients (51 M/74 F), mean age 80.5 years, Comorbidity: Cumulative Illness Rating Scale CIRS-CI: 4, CIRS SI: 1.8. About 38% scored a BRASS (Blaylock Risk Assessment Screening Score) ≥20 indicating need for discharge planning requiring step-down care. More than 50% of patients present IIA index >3 indicating high dependency from nursing assistance. Nurses saved a minimum of 49,6 minutes to a maximum of 58,1 minutes on time spent monitoring each patient per day. A trend towards reduction of major complications in the experimental group appears to be seen (31% versus 45%). Decrease in re-admissions (7% versus 11%) and mortality (7.3% versus 23.9%) has been observed. Arrhythmic and ischemic complications detection doubled in the experimental arm. More than 30% of the patients meet the criteria defining end stage disease.
WVPCM, detecting early deterioration in CIPs, may facilitate timely response in at-risk patients, increasing safety and reducing costs.
LIMS preliminary outcomes
| . | Experimental Arm . | Control Arm . |
|---|---|---|
| Major Complications | 29,5% | 43,5% |
| Repeated readmissions after 21 days from discharge | 7,0% | 10,2% |
| LOS (Length of stay) | 11,6 | 10,5 |
| End stage disease defined according to the “surprise question” | 39.6% | 34,0% |
| Deaths | 9,3% | 16,0% |
| Discharge home | 44,2% | 56,0% |
| Transfer to step-down care | 43,9% | 17,4% |
| Impact on nursing activity | Reduction of time spent by the nurse on the detection of vital signs: 49−58 min / day / patient. | |
| . | Experimental Arm . | Control Arm . |
|---|---|---|
| Major Complications | 29,5% | 43,5% |
| Repeated readmissions after 21 days from discharge | 7,0% | 10,2% |
| LOS (Length of stay) | 11,6 | 10,5 |
| End stage disease defined according to the “surprise question” | 39.6% | 34,0% |
| Deaths | 9,3% | 16,0% |
| Discharge home | 44,2% | 56,0% |
| Transfer to step-down care | 43,9% | 17,4% |
| Impact on nursing activity | Reduction of time spent by the nurse on the detection of vital signs: 49−58 min / day / patient. | |
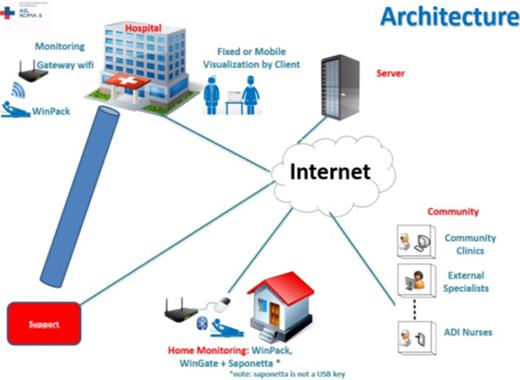
Telemedicine Network
Type of funding source: None
- ischemia
- comorbidity
- critical illness
- internal medicine
- length of stay
- nurses
- patient readmission
- risk assessment
- safety
- telemedicine
- arm
- economics
- mortality
- vital signs
- terminal illness
- stratification
- discharge planning
- transfer technique
- wireless technology
- patient monitoring
- primary outcome measure
- national early warning score (news)
- early warning score



