-
PDF
- Split View
-
Views
-
Cite
Cite
J Sonck, D Munhoz, T Mizukami, A Tajima, K Sakai, T Storozhenko, S Biscaglia, F Rivero, T Engstrom, L Van Nunen, W Fearon, S Fournier, A M Leone, B De Bruyne, C Collet, The PPG Global Study Team, Impact of the pullback pressure gradient (PPG) on PCI planning and decision-making, European Heart Journal, Volume 45, Issue Supplement_1, October 2024, ehae666.1399, https://doi.org/10.1093/eurheartj/ehae666.1399
Close - Share Icon Share
Abstract
Coronary physiology using a distal measurement of fractional flow reserve (FFR) informs about the severity of coronary artery disease (CAD) and, when used for clinical decision-making about revascularisation, is associated with improved outcomes in patients considered for PCI. A second dimension of coronary physiology is available by performing a pullback maneuver, which aids in assessing the presence and location of focal pressure gradients. Yet, the impact of intracoronary physiology guidance with FFR pullbacks on real-time physician decision-making during PCI is not fully known.
This prospective study was performed at 25 sites and enrolled patients with at least one epicardial lesion with FFR ≤ 0.80 planned to be treated by PCI. A standardized physiological assessment with FFR pullbacks and Pullback Pressure Gradient (PPG) calculation was performed. Treatment plans were recorded for each lesion based on angiography alone and following FFR pullbacks. The goal of this study was to assess the procedural impact of physiology guidance in stable patients scheduled for PCI.
Overall, 993 patients (1044 vessels) underwent complete physiological assessment with FFR and PPG. Decision-making during PCI changed in 47.5% (443/1044) after FFR pullbacks. Decision-making during PCI changed in 32.4% (289/890) after FFR pullbacks. PPG use changed revascularisation decisions in 13.9% (138/993) from PCI to CABG (5%; 50/993), from PCI to CABG in 5% (50/993) and to medical management in 8.9% ( 88/993). The frequency of decision changes was significantly higher in patients with diffuse CAD compared to focal cases (24.8% vs. 44.2%, p < 0.001). Among the subset of 855 patients (involving 880 vessels) who underwent PCI, operators modified decision-making regarding stent length in 22.1% of cases (197 out of 880), with these alterations being more prevalent in patients with diffuse CAD (57.2% vs. 46.3%, p = 0.002). Suboptimal Post-PCI result (FFR < 0.88) was more frequent in cases in which PCI strategy was not adapted based on PPG (55.5% vs. 45.6%, p= 0.016) Importantly, there was no significant change in the overall number of stents per patient after FFR pullbacks.
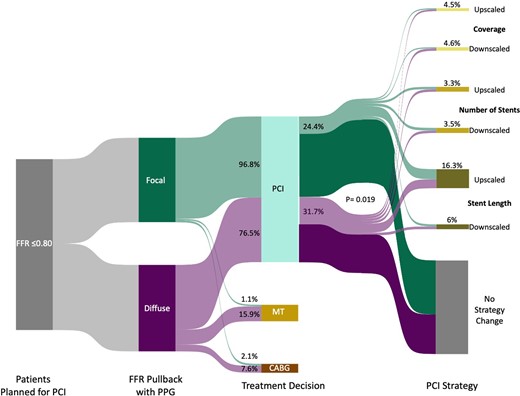
PCI strategy change based on PPG
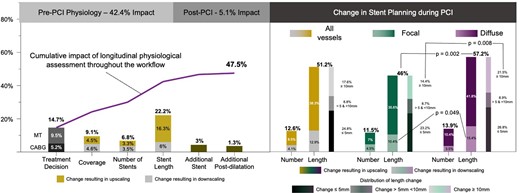
Cumulative change of PCI strategy
Author notes
Funding Acknowledgements: Type of funding sources: Private grant(s) and/or Sponsorship. Main funding source(s): The study was sponsored by the Cardiovascular Research Institute (CRI) Aalst with an unrestricted grant from Abbott Vascular.



