-
PDF
- Split View
-
Views
-
Cite
Cite
A Pons Riverola, S Yun, N Jose, E Hidalgo, M Ruiz, L Alcoberro, S Jimenez, P Moliner, R Ramos, M Ras, J M Verdu, A Garay, M Corbella, C Enjuanes, J Comin-Colet, Bio-Heart Cardiovascular Diseases Research Group, Effect of telemedicine on self-care in heart failure patients: insights from the iCOR randomised controlled trial, European Heart Journal, Volume 44, Issue Supplement_2, November 2023, ehad655.2958, https://doi.org/10.1093/eurheartj/ehad655.2958
Close - Share Icon Share
Abstract
Poor self-care in heart failure (HF) patients is well recognised to lead to a worse prognosis, through an increased risk of readmissions and mortality. In this regard, the integration of eHealth-based telemonitoring and tele-intervention tools into integrated HF-care programmes could help to improve the self-care of these patients. Nevertheless, the current evidence regarding the impact of eHealth solutions on the self-care of HF patients is scarce.
To evaluate the effect of telemedicine (TM) on self-care behaviour in patients with HF after hospital admission compared to usual care (UC).
We designed a post-hoc analysis of the "Insuficiència Cardíaca Optimització Remota" (iCOR) study focussing on self-care. iCOR was a randomised, controlled, single-centre proof-of-concept clinical trial, designed to evaluate the efficacy to adding a eHealth-solution to an existing specialised, comprehensive, multidisciplinary, nurse-based, hospital/primary care integrated HF management programme. Participants were randomised to TM or UC after hospital discharge ("vulnerable-phase") and were followed for 6 months. The primary study endpoint of the current analysis was the delta change of self-care after 6 months of follow-up, assessed using European Heart Failure Self-care Behaviour Scale-12 item (EHFScBS-12 item, lower scores meaning better self-care). To assess the change in self-care between the 2 groups, a repeated-measures ANOVA analysis was performed, adjusted for baseline self-care.
178 patients were analysed (81 TM vs 97 UC). The median age of the patients was 74±11 years, 41% were female and the median ejection fraction was 47±17%. Self-care at baseline had a median score of 21.6±10.5 points.
As shown in Figure 1, there were no differences in baseline values of self-care between the two comparison groups (21.9±11 TM vs 21.5±11 UC, p-value > 0.05). Both groups experienced an improvement in self-care over time (p-value 0.002 for time effect). However, patients in the TM group experienced greater improvement (from 21.9±11 to 14±0.7 mean Delta change = -7.9±11) than in the UC (21.3±10.5 to 19±0.7, mean delta change = -2.2±10.4, p-value <0.001 in inter-groups comparison) (Figure 1). We designed several multivariate linear regression models exploring the determinants of self-care at baseline and the determinants of change in self-care over time. As shown in Table 1, baseline self-care and randomisation arm were the only independent predictors of improvement of self-care over time.
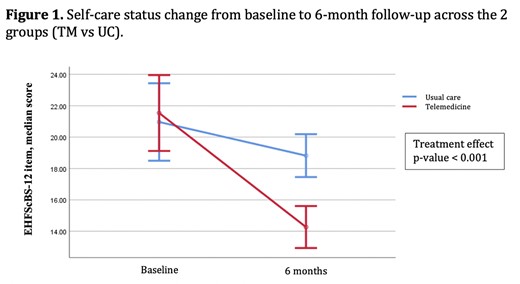
Self-care status change
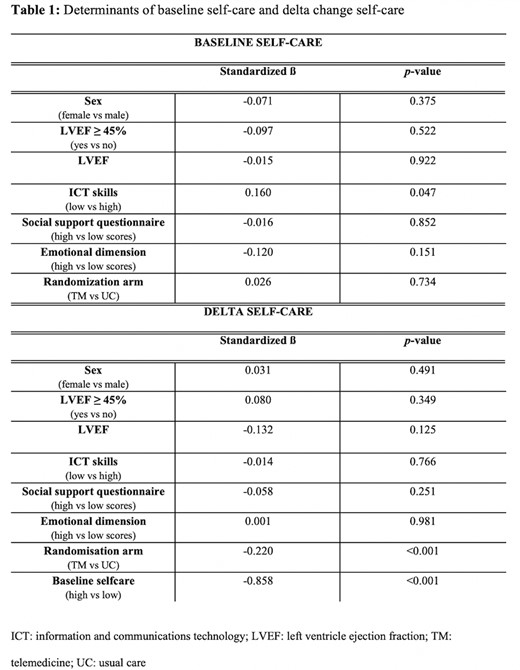
Determinants of self-care
Author notes
Funding Acknowledgements: None.



