-
PDF
- Split View
-
Views
-
Cite
Cite
M Gegenava, T Gegenava, Prognostic significance of pulmonary hypertension in patients with connective tissue disorders: review and meta-analysis, European Heart Journal, Volume 44, Issue Supplement_2, November 2023, ehad655.2766, https://doi.org/10.1093/eurheartj/ehad655.2766
Close - Share Icon Share
Abstract
Pulmonary hypertension (PH) is a frequent complication of connective tissue disorders (CTD) with major impact on prognosis of the disease, especially in patients with systemic sclerosis (SSc). Recently suggested new classification based on the hemodynamic assessment of PH and currently available pharmacologic treatment can be associated with improved survival, therefore underlining the group of the patients with PH and most affected survival function is crucial.
Objectives of our study were to perform systemic review and meta-analysis of published literature evaluating survival function in patients with SSc and Systemic lupus erythematosus (SLE) with and without PH, also to compare PH-associated survival function in between patients with SSc, systemic lupus erythematosus (SLE), other connective tissue disorders (CTD) and conditions characterized with PH.
Literature search strategies, inclusion and exclusion criteria, outcome measurements, and statistical methods were analyzed according to an established protocol of the cochrane collaboration steps and meta-analysis of observational studies in epidemiology recommendations (MOOSE). Case control studies evaluating PH-associated survival function in SSc (including interstitial lung disease -ILD) and SLE patients and also studies comparing survival function among SSc, various CTD entities and conditions associated with PH were included in the analysis.
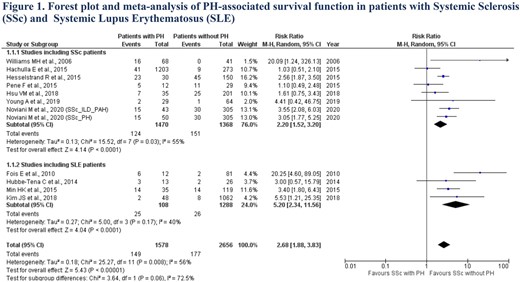
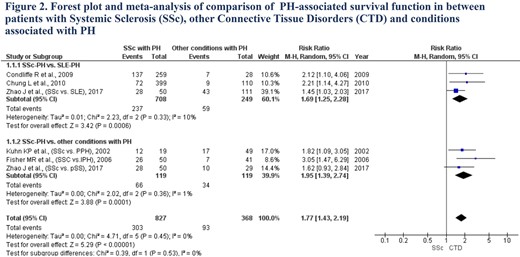
A total of 2114 papers were collected according to our searching criteria, of those 7 studies including 1470 SSc patients with PH and 1368 SSc patients without PH, also 4 studies including 108 SLE patients with PH and 1288 SLE patients without PH and evaluated survival function were selected. We also performed meta-analysis of 6 studies (including 777 SSc, 249 SLE, 41 idiopathic PH (IPH), 49 primary PH (PPH) and 29 primary Sjogren’s syndrome (pSS) patients) comparing PH-associated survival function in different subgroups. The mean pooled follow-up was 5.4 years (5.4±4.4 year). We observed that SSc patients with PH showed worst survival as compared to SSc patients without PH [RR (95 %CI) 2.20 (1.52 to 3.20); p<0.00001] (Figure1). Same pattern was observed in patients with SLE [RR (95 %CI) 5.20 (2.34 to 11.56); p<0.00001] (Figure 1). Overall, SSc patients with PH were characterized with lower survival function as compared to other reasons of PH including SLE [RR (95 %CI) 1.77 (1.43 to 2.19); p<0.00001] (Figure 2).
Author notes
Funding Acknowledgements: None.



