-
PDF
- Split View
-
Views
-
Cite
Cite
Raffaele De Caterina, Riccardo Liga, William E Boden, Myocardial revascularization in ischaemic cardiomyopathy: routine practice vs. scientific evidence, European Heart Journal, Volume 43, Issue 5, 1 February 2022, Pages 387–390, https://doi.org/10.1093/eurheartj/ehab680
Close - Share Icon Share
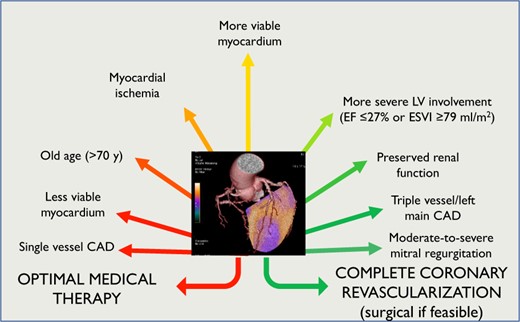
Factors contributing to the decision for coronary revascularization in patients with ischaemic cardiomyopathy. According to existing evidence, coronary artery bypass graft should be considered the revascularization strategy of choice in patients with ischaemic cardiomyopathy, improving prognosis although at prolonged follow-up. However, in patients with unfavourable clinical characteristics and unsuitable coronary anatomy, particularly in the presence of otherwise uncontrolled anginal chest pain, PCI may become a reasonable alternative for symptom control. CAD, coronary artery disease; EF, ejection fraction; ESVI, end-systolic volume index.
Patients with extensive coronary artery disease (CAD) and significant left ventricular (LV) systolic dysfunction [ejection fraction (EF) <35–40%] with or without heart failure (HF)—hereafter referred to as ischaemic cardiomyopathy (ICM)—have an unfavourable prognosis.1 , 2 Current ESC guidelines3 recommend myocardial revascularization in ICM patients with suitable coronary anatomy, using either coronary artery bypass graft (CABG) or percutaneous coronary intervention (PCI). Real-world data indicate that PCI has become the revascularization strategy of choice in ICM, with usage rates now nearly 3-times higher than CABG.4
We will briefly summarize the scientific evidence for revascularization with either CABG or PCI in patients with ICM, the guiding principles to support its continued use, and the disturbing discordance between current clinical practice and scientific evidence.
Rationale and premises of revascularization in ischaemic cardiomyopathy
The principle underlying presumed revascularization benefit in ICM patients is that increased blood supply to ischaemic but viable, ‘hibernating’ myocardial segments would improve symptoms, regional ischaemia, global LV function, and, as a consequence, clinical outcomes. Therefore, it is logical that coronary revascularization for ICM would benefit only those patients with objective evidence of myocardial ischaemia or of hibernating myocardium. ICM patients may or may not have angina. In patients in whom angina persists despite medical therapy (MT), revascularization is an acceptable option. This is, however, only indirectly supported by data in patients without severe LV dysfunction,5 with compelling evidence for symptom improvement largely lacking in ICM patients. In such patients, HF symptoms usually predominate over angina,6 and the disease trajectory—both for symptoms and for outcomes—becomes dominated largely by LV systolic dysfunction and its arrhythmic consequences rather than by ischaemia and the risk of future myocardial infarction (MI).2 In line with these data, best evidence obtained in patients with ICM did not demonstrate improved clinical outcome with therapies directed at the atherosclerotic substrate like statins,7 while contemporary HF medications (i.e. sacubitril-valsartan and sodium-glucose cotransporter 2 inhibitors) do improve outcomes in HF patients at large.
Ischaemia and viability assessment to guide revascularization
Contrasting with the above-detailed rationale, available evidence casts doubt on the utility of ischaemia testing to guide revascularization in ICM patients. Prior observational data derived from perfusion imaging studies do not support an interaction between ischaemic burden and revascularization outcomes (P = 0.469) in patients with extensive myocardial scar (≥10% of the LV myocardium),8 a condition typically encountered in ICM. Such findings have been confirmed by the nuclear sub-study of ‘The Surgical Treatment for Ischaemic Heart Failure’ (STICH) trial, with similar mortality in revascularized patients with or without ischaemia (35% vs. 33%; P = 0.64).9 More recently, in the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial, enrolling largely patients with preserved LV systolic function, there was no signal of benefit or treatment interaction between the severity of ischaemia and improved outcomes with revascularization.5 Notably, in that study, hospitalization for HF was more than two-fold higher among patients randomized to the invasive strategy compared to MT alone [hazard ratio (HR): 2.23, 95% confidence interval (CI): 1.38–3.61].5 A recent sub-analysis of the trial seemed to suggest a possible benefit of coronary revascularization in patients with HF.10 However, the results of that sub-study were largely driven by some positive effects of revascularization in a small subgroup of 28 patients with HF and mild-to-moderately reduced LV EF (35–45%), making the sub-study only hypothesis-generating, and data not generalizable to the larger population of ICM patients.
The role of viability testing in the management of patients with ICM also remains ill-defined because available prospective studies have failed to show any prognostic advantage of viability-guided revascularization.11 , 12 In STICH, no significant interaction was found between myocardial viability and benefit from CABG over MT only, relating both to clinical outcomes (P = 0.34 for interaction) and post-revascularization improvements in LV EF (+1.9% with MT vs. +2.5% with CABG; P = NS).12 It has been argued that such an analysis was limited because viability was not assessed with the most accurate imaging modalities available, such as cardiac magnetic resonance imaging or positron emission tomography (PET). To test this more rigorously, the ‘Positron Emission Tomography and Recovery Following Revascularization’ (PARR-2) study randomized 430 ICM patients to either standard care or PET-guided revascularization, where invasive management was mandated only in patients with a significant burden of hibernating myocardium and showed a similar rate for the composite endpoint of cardiac death, MI, or cardiac hospitalization in the two arms [relative risk (RR) 0.82, 95% CI 0.62–1.07; P = 0.15].11 When a post-hoc analysis was restricted to 142 patients in whom management was adherent to PET recommendations, there was a statistically nominal prognostic benefit of PET-guided management over standard care (RR 0.73, 95% CI 0.54–0.99; P = 0.042),11 though the event-rate difference was primarily driven by the softer cardiac rehospitalization endpoint, with no impact of viability-guided management on mortality.
Revascularization strategies in comparison
Demonstration of a role for myocardial revascularization in ICM relies largely on old data and to the early era of CABG surgery, whereby the Coronary Artery Surgery Study registry showed that patients with CAD and severe LV systolic dysfunction (EF ≤35%)—without any systematic assessment of ischaemia or viability—had a poor prognosis if managed only medically (survival rate of 54% at 5 years, but 68% when revascularized with CABG).1 At that time, however, MT in CAD patients, with or without HF, was very limited pharmacologically to just nitrates and beta-blockers. Moreover, the number of patients with reduced (<35%) EF was small (n = 651).1 The long-term results of STICH (median follow-up duration: 9.8 years) provide more contemporary evidence on the prognostic impact of revascularization in ICM patients,2 demonstrating a 16% lower all-cause mortality in the CABG group compared to the MT group (P = 0.02), particularly in patients with three-vessel CAD or severely remodelled LV architecture (end-systolic volume index >78.6 mL/m2 or EF ≤26.7%).13
Because the early increase in periprocedural mortality and stroke observed with CABG is offset by beneficial effects only after about 2 years, many have hypothesized that PCI would offer a better risk-benefit balance in CAD patients with suitable coronary anatomy. As said, current ESC guidelines are thus quite permissive in recommending which revascularization strategy can be used in ICM patients and suggest ‘considering’ PCI as an alternative to CABG ‘when complete revascularization can be expected’.3 However, also because stenting addresses only focal stenoses judged as ‘hemodynamically significant’, whereas CABG uses conduits to bypass both obstructive and the non-obstructive vulnerable plaques that harbour future MIs, PCI is associated with much less ‘complete revascularization’.14 In patients with CAD, the atherosclerotic burden, rather than the number of flow-limiting lesions, is a key prognostic determinant.14 A fundamental difference in outcomes between the two treatment modalities is also supported by a network meta-analysis,15 as well as the recent results of the Swedish Coronary Angiography and Angioplasty Registry, reported in this issue of the Journal, showing that CABG was associated with lower mortality than PCI, translating into an average 0.5 years of additional event-free survival over 10 years.4 While PCI could represent an alternative to CABG in patients with lower anatomic CAD burden (i.e. a low SYNTAX score), as well as in patients ineligible to surgical revascularization (i.e. poor surgical targets or severe comorbidities),14 prospective data supporting this approach in ICM are lacking. Importantly, contemporary trials comparing PCI and CABG did not generally include a control population treated with optimal MT only, leaving significant uncertainty about the most appropriate treatment option in ICM patients. Recent advances in optimal MT, including potent HF and anti-thrombotic regimens, have certainly improved the prognosis of medically-managed patients with ICM. It is tempting to speculate that—if properly tested—outcomes of current optimal MT would be similar to PCI revascularization, as was clearly demonstrated in moderate–high-risk patients predominantly without HF in ISCHEMIA.5 The ongoing REVIVED-BCIS2 trial16 is assessing the incremental role of myocardial revascularization with PCI over contemporary MT in ICM. However, the small study size (700 patients) and the absence of a CABG arm will still not provide definitive answers to the important remaining management questions in such high-risk patients, although the results of the trial might be valuable for the management of selected ICM patients ineligible to CABG.
Conclusions
PCI-based revascularization in ICM patients has a rationale, but not evidentiary proof, in relieving ischaemic symptoms. In the context of studies with extended follow-up, only CABG surgery has evidence of being associated with a prognostic benefit over current optimal MT in ICM patients, and this appears largely independent of the results of ischaemia and viability testing. It is instructive to recount that the great majority of guideline recommendations in ICM patients do not derive from RCT-based evidence, but rather expert opinion/consensus. Thus, despite the prevalent belief in applying the presumed ‘art’ of personalized medicine, current evidence does not support ischaemia and viability testing to guide coronary revascularization in ICM patients. Similarly, no prospective evidence supports the widespread use of PCI-based revascularization in ICM, the impact of which on hard outcomes should be carefully re-evaluated in selected patients ineligible to CABG (Graphical Abstract).
Conflict of interest: none declared.
References



