-
PDF
- Split View
-
Views
-
Cite
Cite
Suzanne R Avis, Stephen T Vernon, Emil Hagström, Gemma A Figtree, Coronary artery disease in the absence of traditional risk factors: a call for action, European Heart Journal, Volume 42, Issue 37, 1 October 2021, Pages 3822–3824, https://doi.org/10.1093/eurheartj/ehab474
Close - Share Icon Share
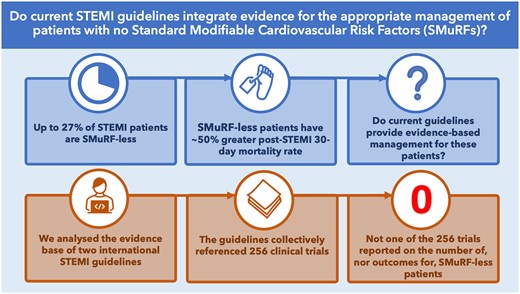
We examined the 256 clinical trials underpinning the two current international ST-elevation myocardial infarction (ST EMI) management guidelines to ascertain the proportion of trials that reported patients with no standard modifiable risk factors as a separate group.
The key role of hypertension, hypercholesterolaemia, diabetes mellitus, and smoking in causing coronary artery disease (CAD) has been well-recognized at a population level and has been the target of highly effective primary and secondary prevention strategies for over 50 years. However, a substantial, and increasing, proportion of patients presenting with life-threatening acute coronary syndrome (ACS) have none of these standard modifiable cardiovascular risk factors (SMuRFs).1 , 2 A meta-analysis of 14 clinical trials utilizing individual patient level data for 122 458 patients reported that 17% of coronary heart disease patients had no SMuRFs,3 a proportion similar to the 15% we recently reported in 62 048 ST-elevation myocardial infarction (STEMI) patients in the SWEDEHEART Registry.4 We have observed the proportion to be increasing in two separate Australian STEMI cohorts from ∼14% to as high as 27% over 10 years.5 , 6 Whilst this remains a relatively small proportion of the ‘pie’, the global burden of CAD makes their absolute number substantial, estimated conservatively to impact 29.6 million, and to account for 1.4 million deaths per annum.7 Despite this, SMuRF-less CAD patients appear to be an invisible group in current clinical trials and guidelines, with little known about their outcomes or the best approach to their management and secondary prevention strategies. Our recent finding that SMuRF-less STEMI patients have an almost 50% higher 30-day mortality rate than their counterparts with SMuRFs highlights the importance of establishing evidence for their management.4
We sought to ascertain the extent to which current international guidelines for the management of STEMI integrate evidence for the appropriate clinical management of STEMI patients who have developed coronary atherosclerosis despite no SMuRFs. We assessed both the European Society of Cardiology (ESC) and the American College of Cardiology/American Heart Association (ACC/AHA) guidelines, to determine the proportion of trials underpinning the guideline recommendations that reported the number or percentage of participants with no SMuRFs.8 , 9
Combined, the ESC and ACC/AHA STEMI guidelines reference a total of 1133 studies, with 256 of these being clinical trials. For each of these 256 trials, we assessed for the reporting of number/percentage of participants with each of the SMuRFs (hypertension, smoking, hypercholesterolaemia, and diabetes mellitus). We next assessed if the number/percentage of participants with none of these risk factors was reported. As shown in Table 1, diabetes mellitus (86%) and hypertension (86%) were the most commonly reported risk factors in these trials, followed by smoking (72%) and hypercholesterolaemia (58%). It is important to acknowledge that the number/proportion of patients with no risk factors cannot be derived even if the number of patients with each of the four SMuRFs is reported, as many patients will have more than one risk factor. In contrast to the reporting of each of the individual risk factors, not one study of the 256 clinical trials explicitly reported the proportion of patients with no risk factors. A single trial from Sabatine et al. 10 reported the proportion of participants that had ‘any’ risk factor, and therefore, the proportion of those who had no risk factors could be derived. Not surprisingly given our findings, no study reported any trial outcome specifically for this group either in primary or secondary analyses (Graphical abstract) .
Coronary artery disease risk factors reported in controlled clinical trials referenced in the 2017 European Society of Cardiology and 2013 American College of Cardiology/American Heart Association ST-elevation myocardial infarction management guidelines
| . | Unique to 2017 ESC STEMI guideline . | Unique to 2013 ACC/AHA STEMI guideline . | Common to both ESC 2017 and ACC/AHA 2013 STEMI guidelines . | Total . |
|---|---|---|---|---|
| Clinical trials, n | 109 | 99 | 48 | 256 |
| Trials that reported participants by, n (%) | ||||
| Hypertension | 94 (86) | 82 (83) | 43 (90) | 219 (86) |
| Diabetes mellitus | 96 (88) | 83 (84) | 42 (88) | 221 (86) |
| Tobacco use | 77 (71) | 73 (74) | 34 (71) | 184 (72) |
| Hypercholesterolaemia | 66 (61) | 56 (57) | 26 (54) | 148 (58) |
| No risk factorsa | 0 (N/A) | 0 (N/A) | 0 (N/A) | 0 (N/A) |
| . | Unique to 2017 ESC STEMI guideline . | Unique to 2013 ACC/AHA STEMI guideline . | Common to both ESC 2017 and ACC/AHA 2013 STEMI guidelines . | Total . |
|---|---|---|---|---|
| Clinical trials, n | 109 | 99 | 48 | 256 |
| Trials that reported participants by, n (%) | ||||
| Hypertension | 94 (86) | 82 (83) | 43 (90) | 219 (86) |
| Diabetes mellitus | 96 (88) | 83 (84) | 42 (88) | 221 (86) |
| Tobacco use | 77 (71) | 73 (74) | 34 (71) | 184 (72) |
| Hypercholesterolaemia | 66 (61) | 56 (57) | 26 (54) | 148 (58) |
| No risk factorsa | 0 (N/A) | 0 (N/A) | 0 (N/A) | 0 (N/A) |
ACC/AHA, American College of Cardiology/American Heart Association; ESC, European Society of Cardiology; N/A, not available; STEMI, ST-elevation myocardial infarction.
In one study (Sabatine et al. 10), the proportion of SMuRF-less patients could be calculated from other reported data; however, it was not explicitly reported, nor were any trial outcomes reported separately.
Coronary artery disease risk factors reported in controlled clinical trials referenced in the 2017 European Society of Cardiology and 2013 American College of Cardiology/American Heart Association ST-elevation myocardial infarction management guidelines
| . | Unique to 2017 ESC STEMI guideline . | Unique to 2013 ACC/AHA STEMI guideline . | Common to both ESC 2017 and ACC/AHA 2013 STEMI guidelines . | Total . |
|---|---|---|---|---|
| Clinical trials, n | 109 | 99 | 48 | 256 |
| Trials that reported participants by, n (%) | ||||
| Hypertension | 94 (86) | 82 (83) | 43 (90) | 219 (86) |
| Diabetes mellitus | 96 (88) | 83 (84) | 42 (88) | 221 (86) |
| Tobacco use | 77 (71) | 73 (74) | 34 (71) | 184 (72) |
| Hypercholesterolaemia | 66 (61) | 56 (57) | 26 (54) | 148 (58) |
| No risk factorsa | 0 (N/A) | 0 (N/A) | 0 (N/A) | 0 (N/A) |
| . | Unique to 2017 ESC STEMI guideline . | Unique to 2013 ACC/AHA STEMI guideline . | Common to both ESC 2017 and ACC/AHA 2013 STEMI guidelines . | Total . |
|---|---|---|---|---|
| Clinical trials, n | 109 | 99 | 48 | 256 |
| Trials that reported participants by, n (%) | ||||
| Hypertension | 94 (86) | 82 (83) | 43 (90) | 219 (86) |
| Diabetes mellitus | 96 (88) | 83 (84) | 42 (88) | 221 (86) |
| Tobacco use | 77 (71) | 73 (74) | 34 (71) | 184 (72) |
| Hypercholesterolaemia | 66 (61) | 56 (57) | 26 (54) | 148 (58) |
| No risk factorsa | 0 (N/A) | 0 (N/A) | 0 (N/A) | 0 (N/A) |
ACC/AHA, American College of Cardiology/American Heart Association; ESC, European Society of Cardiology; N/A, not available; STEMI, ST-elevation myocardial infarction.
In one study (Sabatine et al. 10), the proportion of SMuRF-less patients could be calculated from other reported data; however, it was not explicitly reported, nor were any trial outcomes reported separately.
The invisibility of SMuRFless CAD patients in guidelines or in the clinical trials that the guidelines are derived from means the outcomes and specific challenges regarding secondary prevention for this group have not been adequately addressed. Many of the drugs in our armament for secondary prevention have been developed to target specific risk factors but are frequently applied in guidelines in a manner agnostic to these features. The most obvious examples are the use of statins vs. hypercholesterolaemia, and the angiotensin-converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB) family initially developed to target high blood pressure. It is feasible that the beneficial effects of these agents may be attenuated in those whose atherosclerosis has developed in the absence of high cholesterol or high blood pressure. However, both of these pivotal medication classes are recognized to have potential ‘off target’ benefits—directly on endothelial function and plaque stability in the case of statins, and on redox- and inflammatory-mediated vascular and myocardial pathophysiology in the case of ACEI/ARBs.11 , 12
It is feasible that a proportion of the SMuRF-less CAD group are simply individuals whose atherosclerotic disease progression has been ‘missed’; the remainder are likely to be heterogeneous with regard to underlying biology, and pathways may encompass inflammatory processes, environmental exposures, and interactions with chronic conditions such as chronic kidney disease and autoimmune diseases. There is a growing body of literature regarding emerging risk tools such as polygenic risk scores and multi-omic signatures as well as lipoprotein (a) and C-reactive protein novel markers of risk that may be relevant to SMuRF-less ACS patients; however, these biomarkers are not routinely utilized in primary prevention cardiovascular risk scores.13 , 14 Genome-wide association studies and Mendelian randomization analyses may prove useful in eliciting markers of risk and underlying pathological processes.15
In addition to potentially distinct pathophysiological processes, SMuRF-less CAD patients have specific challenges regarding adherence to secondary prevention guidelines that have been observed in the large SWEDEHEART Registry and the Canadian GRACE cohort.2 , 4 This lower rate of statin, ACEI/ARB, and ß-blocker therapy prescription early post STEMI appears to mediate at least some of the excess mortality in SMuRF-less STEMI patients.4
Despite the tremendous progress that has been made in the evidence-based management of CAD and ACS, our findings demonstrate that current ACS guidelines do not specifically address the management of patients who develop coronary atherosclerosis in the absence of traditional risk factors. Improved visibility of this SMuRF-less CAD population in future trials, especially those trials examining novel risk factors, together with dedicated secondary analyses and meta-analyses using individual patient level data from existing clinical trials may provide important insights to guide clinical pathways and guidelines for these vulnerable patients.
Conflict of interest: G.A.F. reports grants from National Health and Medical Research Council (Australia), personal fees from CSL, and grants from Abbott Diagnostic during the conduct of the study. G.A.F. has a patent to ‘Patent Biomarkers and Oxidative Stress’ awarded USA May 2017 (US9638699B2) licenced, a patent to ‘Use of P2X7R antagonists in cardiovascular disease’ PCT/AU2018/050905 licenced, and a patent to ‘Methods for treatment and prevention of vascular disease’ PCT/AU2015/000548 licenced. E.H. reports grants and personal fees from Amgen and Sanofi and personal fees from Bayer and NovoNordisk, outside the submitted work. S.T.V. has no interests to declare. S.R.A. has no interests to declare.
Data availability
The original data for this study are managed by the Kolling Institute and the University of Sydney and can be made available through contacting the corresponding author and engaging in a formal research application.
References



