-
PDF
- Split View
-
Views
-
Cite
Cite
M Giustozzi, RAF and RAF-NOACs studies collaborators , Safety of early anticoagulation in patients treated with urgent reperfusion for acute ischemic stroke related to non-valvular atrial fibrillation, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.2431, https://doi.org/10.1093/ehjci/ehaa946.2431
Close - Share Icon Share
Abstract
The optimal timing for starting anticoagulation after an acute ischemic stroke related to non-valvular atrial fibrillation (AF) remains a challenge, especially in patients treated with systemic thrombolysis or mechanical thrombectomy.
We aimed to assess the rates of early recurrence and major bleeding in patients with acute ischemic stroke and AF treated with thrombolytic therapy and/or thrombectomy who received oral anticoagulants for secondary prevention.
We combined the dataset of the RAF and the RAF-NOACs studies, which were prospective observational studies carried out from January 2012 to March 2014 and April 2014 to June 2016, respectively. We included consecutive patients with acute ischemic stroke and AF treated with either vitamin K antagonists (VKAs) or new oral anticoagulants (NOACs). Primary outcome was the composite of stroke, transient ischemic attack, symptomatic systemic embolism, symptomatic cerebral bleeding, and major extracerebral bleeding within 90 days from the inclusion.
A total of 2,159 patients were included in the RAF and RAF-NOACs trials, of which 564 patients (26%) were treated with urgent reperfusion therapy. After acute stroke, 505 (90%) patients treated with reperfusion and 1,287 out of the 1,595 (81%) patients not treated with reperfusion started oral anticoagulation. Timing of starting oral anticoagulation was similar in reperfusion-treated and untreated patients (13.5±23.3 vs 12.3±18.3 days, respectively, p=0.287). At 90 days, the composite rate of recurrence and major bleeding occurred in 37 (7%) of patients treated with reperfusion treatment and in 139 (9%) of untreated patients (p=0.127). Twenty-four (4%) reperfusion-treated patients and 82 (5%) untreated patients had early recurrence while major bleeding occurred in 13 (2%) treated and in 64 (4%) untreated patients, respectively. Seven patients in the untreated group experienced both an ischemic and hemorrhagic event. Figure 1 shows the risk of early recurrence and major bleeding over time in patients treated and not treated with reperfusion treatments. The use of NOACs was associated with a favorable rate of the primary outcome compared to VKAs (Odd ratio 0.4, 95% Confidence Interval 0.3–0.7).
Reperfusion treatment did not influence the risk of early recurrence and major bleeding in patients with AF-related acute ischemic stroke who started anticoagulant treatment.
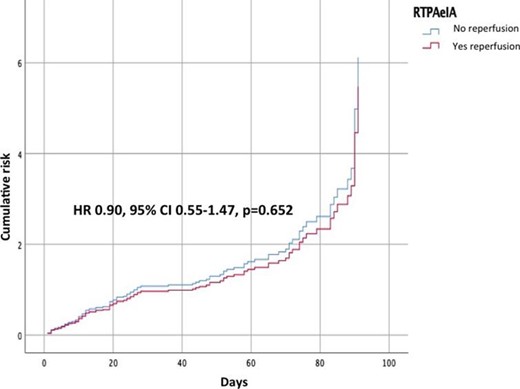
Figure 1
Type of funding source: None



