-
PDF
- Split View
-
Views
-
Cite
Cite
I Marco Clement, S.O Rosillo Rodriguez, C Merino Argos, L Martin-Polo, L.A Martinez-Marin, L Rodriguez-Sotelo, E Arbas Redondo, D.I Poveda Pinedo, D Tebar Marquez, E Armada Romero, D Garcia-Arribas, O Gonzalez Fernandez, J Caro Codon, J.L Lopez-Sendon, E Lopez-De-Sa, Impact of resuscitation guidelines updates on global outcomes after cardiac arrest, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.1858, https://doi.org/10.1093/ehjci/ehaa946.1858
Close - Share Icon Share
Abstract
Cardiopulmonary resuscitation (CPR) Guidelines are updated every five years in the light of new evidence. Recent major changes emphasized the importance of quality chest compressions during CPR and simplified recommendations for lay providers, but it is unknown whether these changes improved neurological outcomes.
To analyse whether changes in CPR guidelines had an impact on the prognosis of comatose survivors after cardiac arrest (CA).
Prospective database of consecutive patients (pts) admitted to the acute cardiac care unit of a tertiary hospital after in-hospital and out-of-hospital CA (IHCA and OHCA) treated with targeted temperature management (32–34°) from August 2006 to January 2020. Patients were divided into three groups, each one representing the 5-year time frame of publication/implementation of CPR Guidelines: G1 (2006–2010); G2 (2011–2015); G3 (2016–2020).
A total of 510 pts were included: G1 94 (18.4%), G2 243 (47.6%), G3 173 (33.9%). Mean age was 62.6±14.5 and 413 (81.0%) were men. Demographic characteristics and cardiovascular risk factors did not differ significantly among groups. Changes in CA features among the three analysed periods are shown in Table 1. On regards of prehospital care, CPR provided by lay bystanders (G1 51.6%; G2 63.3%, G3 69.8%) and the use of automated external defibrillators (AED) (G1 11.0%; G2 14.9%; G3 18.9%) progressively increased (p=0.01 and p=0.04, respectively) (Figure 1, A and B). After 2010, there was a higher proportion of CPR-related injuries: G1 12.7%, G2 23.5%, G3 22.7% (p=0.02). Global survival at discharge was 51.6% (263/510). Cerebral Performance Category (CPC) of 1–2 within a 3-month follow-up period significantly increased over time when comparing G1, G2, G3 groups (p=0.04) (Figure 1, D). Among all pts, those with CPR related injuries had a higher proportion of CPC 1–2 (71/109, 65.1% vs 168/389, 43.2%, p<0.01).
We found a progressive increase of lay bystander CPR and use of AED over the three time periods. Moreover, a higher proportion of CPR-related injuries was observed after publication of 2010 CPR Guidelines which recommended greater depth and higher rate of chest compressions. Survival and neurological outcomes improved significantly over time.
Table 1. CA features
| . | G1 (n=94) . | G2 (n=243) . | G3 (n=173) . | p . |
|---|---|---|---|---|
| No-flow, minutes (mean ± SD) | 4.0±4.3 | 4.2±5.0 | 3.7±4.5 | 0.63 |
| Time to ROSC, minutes (mean ± SD) | 24.7±16.4 | 25.4±4.3 | 30.3±22.8 | 0.018 |
| Shockable rhythm, n (%) | 60 (63.8) | 161 (66.3) | 126 (72.8) | 0.049 |
| Out-of-hospital CA, n (%) | 76 (80.9) | 205 (84.4) | 157 (91.8) | 0.019 |
| . | G1 (n=94) . | G2 (n=243) . | G3 (n=173) . | p . |
|---|---|---|---|---|
| No-flow, minutes (mean ± SD) | 4.0±4.3 | 4.2±5.0 | 3.7±4.5 | 0.63 |
| Time to ROSC, minutes (mean ± SD) | 24.7±16.4 | 25.4±4.3 | 30.3±22.8 | 0.018 |
| Shockable rhythm, n (%) | 60 (63.8) | 161 (66.3) | 126 (72.8) | 0.049 |
| Out-of-hospital CA, n (%) | 76 (80.9) | 205 (84.4) | 157 (91.8) | 0.019 |
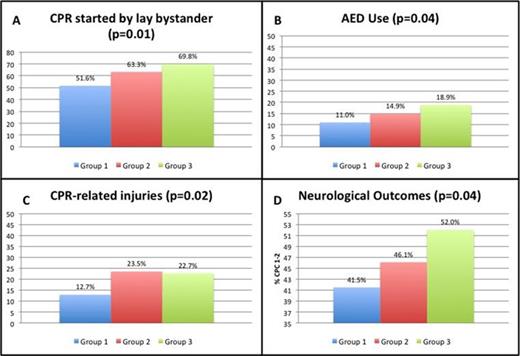
Figure 1
Type of funding source: None
- cardiopulmonary resuscitation
- cardiac arrest
- heart disease risk factors
- coma
- defibrillator, automatic external
- cardiac care facilities
- demography
- follow-up
- resuscitation
- survivors
- time factors
- body temperature
- brain
- guidelines
- temperature
- cardiac progenitor cells
- out-of-hospital cardiac arrest
- return of spontaneous circulation
- cpr prior to ems arrival
- rhythm
- fluid flow
- pre-hospital care



