-
PDF
- Split View
-
Views
-
Cite
Cite
C Merino Argos, I Marco Clement, S.O Rosillo Rodriguez, L Martin Polo, E Arbas Redondo, D Tebar Marquez, D.I Poveda Pinedo, A Velez Salas, L Rodriguez Sotelo, L.A Martinez Marin, O Gonzalez Fernandez, J Caro Codon, V Rial Baston, J.L Lopez-Sendon Hentschel, E Lopez De Sa Areses, Impact of the cardiopulmonary resuscitation-related injuries on the prognosis after cardiac arrest, European Heart Journal, Volume 41, Issue Supplement_2, November 2020, ehaa946.1819, https://doi.org/10.1093/ehjci/ehaa946.1819
Close - Share Icon Share
Abstract
Cardiopulmonary resuscitation (CPR) manoeuvres involve vigorous compressions with the proper depth and rate in order to keep sufficient perfusion to organs, especially the brain. Accordingly, high incidences of CPR-related injuries (CPR-RI) have been observed in survivors after cardiac arrest (CA).
To analyse whether CPR-related injuries have an impact on the survival and neurological outcomes of comatose survivors after CA.
Observational prospective database of consecutive patients (pts) admitted to the acute cardiac care unit of a tertiary university hospital after in-hospital and out-of-hospital CA (IHCA and OHCA) treated with targeted temperature management (TTM 32–34°) from August 2006 to December 2019. CPR-RI were diagnosed by reviewing medical records and analysing image studies during hospitalization.
A total of 498 pts were included; mean age was 62.7±14.5 years and 393 (78.9%) were men. We found a total of 145 CPR-RI in 109 (21.9%) pts: 79 rib fractures, 20 sternal fractures, 5 hepatic, 5 gastrointestinal, 3 spleen, 1 kidney, 26 lung and 6 heart injuries. Demographic characteristics and cardiovascular risk factors did not differ between the non-CPR-RI group and CPR-RI group. Also, we did not find differences in CA features (Table 1). Survival at discharge was higher in the CPR-RI group [74 (67.8%) vs 188 (48.3%); p<0.001]. Moreover, Cerebral Performance Category (CPC) 1–2 within a 3-month follow-up was significantly higher in the CPR-RI group [(71 (65.1%) vs 168 (43.2%); p<0.001; Figure 1]. Finally, pts who recieved blood transfusions were proportionally higher in the CPR-RI group [34 (32.1%) vs 65 (16.7%)]; p=0.004).
In our cohort, the presence of CPR-RI was associated with higher survival at discharge and better neurological outcomes during follow-up.
Table 1
| . | CPR-RI group . | Non-CPR-RI group . | P . |
|---|---|---|---|
| Time to ROSC (minutes) | 28.9 (±20.4) | 26.0 (±17.9) | 0.17 |
| Shockable rhythm | 68.4% | 68.1% | 0.78 |
| Out-of-hospital CA | 84.0% | 86.8% | 0.54 |
| Witnessed CA | 90.5% | 92.5% | 0.49 |
| Lactate level at admission | 6.89±4.41 | 6.18±4.52 | 0.17 |
| pH at admission | 7.16±0.16 | 7.19±0.16 | 0.23 |
| . | CPR-RI group . | Non-CPR-RI group . | P . |
|---|---|---|---|
| Time to ROSC (minutes) | 28.9 (±20.4) | 26.0 (±17.9) | 0.17 |
| Shockable rhythm | 68.4% | 68.1% | 0.78 |
| Out-of-hospital CA | 84.0% | 86.8% | 0.54 |
| Witnessed CA | 90.5% | 92.5% | 0.49 |
| Lactate level at admission | 6.89±4.41 | 6.18±4.52 | 0.17 |
| pH at admission | 7.16±0.16 | 7.19±0.16 | 0.23 |
ROSC: recovery of spontaneous circulation. CA: cardiac arrest.
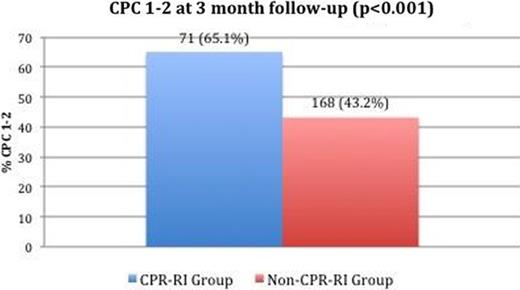
Figure 1
Type of funding source: None
- cardiopulmonary resuscitation
- cardiac arrest
- medical records
- heart injuries
- heart disease risk factors
- lung
- coma
- blood transfusion
- cardiac care facilities
- demography
- follow-up
- hospitals, university
- lactates
- perfusion
- resuscitation
- rib fractures
- survivors
- body temperature
- brain
- kidney
- spleen
- temperature
- sternum fractures
- cardiac progenitor cells
- out-of-hospital cardiac arrest
- return of spontaneous circulation
- rhythm



