-
Views
-
Cite
Cite
C Vandenbriele, A Azzu, A Gambaro, M Morosin, D Arachchillage, R Trimlett, A Rosenberg, S Ledot, B Patel, S Price, P1716
Dual antiplatelet therapy on veno arterial ECMO to bleed or not to bleed?, European Heart Journal, Volume 40, Issue Supplement_1, October 2019, ehz748.0471, https://doi.org/10.1093/eurheartj/ehz748.0471Close - Share Icon Share
Abstract
Patients presenting with INTERMACS-1 cardiogenic shock and necessitating VA-ECMO, often undergo coronary angiography and percutaneous coronary intervention (PCI). Therefore, a substantial subset of VA-ECMO patients will have an indication for dual antiplatelet therapy (DAPT) plus unfractionated heparin (UFH). According to atrial fibrillation registry data, bleeding incidence on DAPT combined with oral anticoagulation is significantly higher as compared to anticoagulation alone. Although it has been reported that the addition of low dose aspirin to UFH did not increase bleeding or transfusion in VenoVenous (VV)-ECMO patients, it remains to be elucidated whether the addition of DAPT to UFH on VA-ECMO-therapy enhances bleeding.
We report single center data for 100 VA-ECMO patients between 2011 and 2019. VA-ECMO-patients post-surgery were excluded. Patient demographics, blood product transfusions and reported/radiographically diagnosed bleeding or thrombotic complications were analysed. All VA-ECMO patients received UFH, aiming for an anti-Xa levels of at least 0,3 U/ml. Targets were hemoglobin 7 g/dl, fibrinogen 100 mg/dl (or 150 mg/dl when active bleeding) and platelet counts above 50/fL. DAPT-patients were on a low dose aspirin plus a P2Y12-inhibitor (clopidogrel or ticagrelor).
51% Of the VA-ECMO-group received DAPT (59% clopidogrel and 41% ticagrelor). UFH-levels were comparable between both groups. Patients on DAPT were significantly older (DAPT 52.8 vs. Control 41.3; p<0.001) and predominantly male (DAPT 76% vs. Control 63%). Total bleedings (DAPT 52% vs. Control 55%; p=0,68) and major bleedings (BARC score of 3 or more; DAPT 41% vs. Control 45%; p=0,71) did not differ significantly. We observed a significant lower number of clinically or radiographically overt arterial/venous thromboses (DAPT 13.7% vs. Control 36.2%; p=0,02) in the DAPT-group. When comparing fresh frozen plasma (FFP), red blood cell and platelet pool transfusions between both groups, only FFP-tranfusion (DAPT 0.47 units/day vs. Control 1.18 units/day; p=0,047) intends to be lower for the DAPT-group.
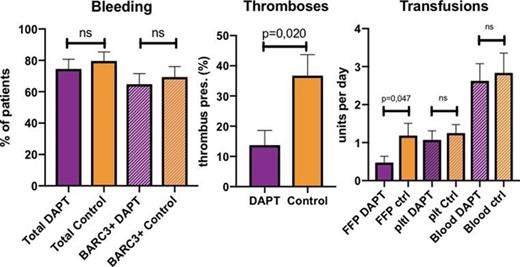
DAPT (plus UFH) vs control (plus UFH)
Haemorrhage is frequent during extracorporeal support. However, in our cohort, DAPT on top of UFH in the treatment of VA-ECMO-supported ischemic cardiogenic shock does not increase the risk of major bleeding. Therefore, DAPT should not necessarily be witheld in the setting of VA-ECMO. Interestingly, our data support a lower incidence of overt thromboses and a trend towards less FFP-transfusion. These findings suggest DAPT-induced platelet inhibition being protective against both thrombotic events and posibly consumptive coagulopathy without paying a price for major bleeding.





