-
PDF
- Split View
-
Views
-
Cite
Cite
Aapo L. Aro, Olli Anttonen, Tuomas Kerola, M. Juhani Junttila, Jani T. Tikkanen, Harri A. Rissanen, Antti Reunanen, Heikki V. Huikuri, Prognostic significance of prolonged PR interval in the general population, European Heart Journal, Volume 35, Issue 2, 7 January 2014, Pages 123–129, https://doi.org/10.1093/eurheartj/eht176
Close - Share Icon Share
Abstract
Prolonged PR interval, or first degree AV block, has been traditionally regarded as a benign electrocardiographic finding in healthy individuals, until recent studies have suggested that it may be associated with increased mortality and morbidity. The aim of this study was to further elucidate clinical and prognostic importance of prolonged PR interval in a large middle-aged population with a long follow-up.
We evaluated 12-lead electrocardiograms of 10 785 individuals aged 30–59 years (mean age 44 years, 52% males) recorded between 1966 and 1972, and followed the subjects for 30 ± 11 years. Prolonged PR interval was defined as PR >200 ms, with further analysis performed using PR ≥220 ms. Main endpoints were all-cause mortality, cardiovascular mortality, and sudden cardiac death, and other endpoints included hospitalizations due to cardiovascular causes. During the baseline examination, prolonged PR interval >200 ms was present in 2.1% of the subjects, but PR interval normalized to ≤200 ms in 30% of these individuals during the follow-up. No increase in mortality or in hospitalizations due to coronary artery disease, heart failure, atrial fibrillation, or stroke was associated with prolonged PR interval (P = non-significant for all endpoints). These results were not changed after multivariate adjustment or in several subanalyses.
In the middle-aged general population, prolonged PR interval normalizes in a substantial proportion of subjects during the time course, and it is not associated with an increased risk of all-cause or cardiovascular mortality.
Introduction
PR interval measured from the surface electrocardiogram (ECG) denotes the time from the beginning of atrial depolarization to the onset of ventricular depolarization. Electrocardiographically, prolonged PR interval, or first-degree atrioventricular (AV) block, is defined by PR interval >200 ms. In the majority of cases, it is due to delayed conduction in the AV node, although conduction delay in the atrium, the His-Purkinje system or multiple sites may also contribute to the prolonged PR interval.1
In the presence of coronary artery disease (CAD), prolongation of PR interval is associated with an adverse outcome,2 but in the absence of structural heart disease or other conduction abnormalities, prolonged PR interval has been traditionally considered a benign phenomenon. This belief has based on older studies conducted mainly among healthy young or middle-aged men, which could not demonstrate additional mortality or morbidity associated with PR prolongation.3–7 Recently, findings from the Framingham Heart Study population have challenged this long-standing perception by demonstrating, that prolonged PR interval is associated with an increased risk of atrial fibrillation (AF) and pacemaker implantation.8,9 Moreover, in contrast with previous studies, prolongation of the PR interval was also associated with all-cause mortality in this community-based sample.9,10
The present work, based on a 30-year follow-up of nearly 11 000 Finnish middle-aged subjects, was carried out with an objective to elucidate the clinical significance of prolonged PR interval in apparently healthy subjects. To our knowledge, it is the largest study conducted in the general population investigating the prognostic significance of prolonged PR interval, and also the first to address the impact of prolonged PR interval on the risk of cardiovascular mortality and sudden cardiac death (SCD).
Methods
Participants
The study population included 10 957 men and women aged 30–59 years, who participated the Finnish Social Insurance Institution's Coronary Heart Disease Study (CHD Study). Initial examinations were carried out 1966–72, and 12 population groups from four different areas of Finland with varying mortality rates were included representing the middle-aged Finnish population. The participation rate of the invited population was 89.6%, and the mean age of the attendees was 44.0 ± 8.5 years (52.3% male). We excluded 58 subjects with missing or unreadable ECGs, 77 subjects with bundle-branch block, pre-excitation, or higher-degree AV block, and 37 subjects with AF or unreadable PR interval. After these exclusions, the final study group composed of 10 785 participants.
Examination and electrocardiographic measurements
A detailed explanation of the CHD study rationale and the procedures performed at the initial examination has been published previously.11 Briefly, 12-lead ECG was taken, blood pressure and body mass index (BMI) were measured, and the participants underwent a routine laboratory assessment of cardiovascular risk factors. Before the examination, subjects completed a questionnaire regarding their history of previous diseases, smoking habits, and their medication during the past 3 months. The questionnaire was then checked and completed, if necessary, by a specially trained nurse. All symptoms of cardiovascular disease were documented during the examination.
Standard 12-lead ECG containing on average seven to eight beats was recorded ∼30 min after arrival to the Mobile Clinic at rest with the subject in the supine position, with a paper speed of 50 mm/s and calibration of 1 mV/10 mm. Eight trained technicians supervised by a physician were responsible for the initial measurements. PR interval was defined as the interval from the onset of the P-wave to the end of the PR segment, and measured from the bipolar limb lead in which the interval was longest. Paper speed 50 mm/s was used to ensure sufficient precision of the measurements, and given the resolution of clinical ECGs and the dynamic nature of the PR interval, measurements were recorded at 10 ms intervals. To further guarantee the accuracy of the electrocardiographic data, all readers were repeatedly evaluated using the standard ECG material that was not part of the present study. When compared with the reference values, intra-class correlation coefficient of r = 0.90 was demonstrated between all readers and the test material for measuring PR interval. Of note, intra-class correlation coefficient of 0.50 indicates moderate correlation, 0.75 excellent correlation, and 1.0 perfect correlation.
Follow-up and outcomes
The participants were followed from Finnish registers for a mean of 30 ± 11 years until the end of 2007. Less than 2% were lost to follow-up as a result of moving abroad, but even in this group, the survival status for the great majority could still be determined. Mortality data were obtained from the Causes of Death Register maintained by Statistics Finland that records every death in the country, and death certificates were obtained for each deceased. The relevant ICD-codes were used to define cardiovascular death. The procedure to identify cases of SCD has been described in detail by our group previously.12 Briefly, every death from cardiac causes was reviewed using death certificates, hospital records, and necropsy reports, if available, based on the definitions presented in the Cardiac Arrhythmic Pilot Study.13 Hospitalizations were obtained from the Finnish Hospital Discharge Register, which includes complete and well-validated nationwide data on all inpatient episodes in Finland at an individual level.14 In addition, a repeat ECG was performed after a median follow-up time of 6 years for 91.7% of the subjects.
Statistical analyses
All continuous data are presented as means ± SD. A general linear model was used to compare age- and sex-adjusted mean values for continuous variables and prevalence of categorical variables between groups. Hazard ratios (HRs) and 95% confidence intervals (CIs) for death and hospitalizations were calculated using the Cox proportional hazards model. Main endpoints were all-cause and cardiovascular mortality, and SCD. First, analyses were done with prolonged PR defined as PR >200 ms. Primary adjustments to these models were for age and sex, with further adjustments for covariates that differed between groups. Age, heart rate, and BMI were added as continuous variables and sex, chronotropic medication and history of cardiovascular disease were added as categorical variables. Subsequent analyses adjusted for age and sex were performed with PR >200 ms excluding subjects with chronotropic medication, suspected cardiovascular disease, and QRS duration of ≥120 ms, and separately with subjects with PR ≥220 ms, and with subjects having suspected cardiovascular disease. Age- and sex-adjusted survival curves were plotted for PR >200 ms. Statistical analyses were performed with the SAS software, version 9.1.3 (SAS Institute) and with Statistical Package for Social Studies, version 14.0 (SPSS). Two-sided statistical tests were used, and P-value < 0.05 was considered to indicate statistical significance.
Results
Electrocardiographic characteristics
Of the 10 785 eligible participants, prolonged PR interval >200 ms was present in 222 subjects (2.1% of the population). Of these subjects, 159 were men (2.8% of all men) and 63 women (1.2% of all women). Markedly prolonged PR interval >240 ms was rare and was only found in 20 individuals (0.2% of the population). Only one subject had PR interval ≥300 ms. The mean PR interval was significantly longer in men than in women (160 ± 22 ms vs. 153 ± 22 ms; P < 0.001). PR interval also increased with age in both sexes. Men aged 30–39, 40–49, and 50–59 years had the mean PR intervals of 158, 160, and 161 ms, and women 150, 152, and 158 ms, respectively.
Baseline characteristics of the participants are presented in Table 1. Subjects with prolonged PR interval were older, more likely to be male, had higher BMI and lower heart rate, and had more often chronotropic medication and suspected cardiovascular disease than those with normal PR interval. One hundred and eighty-six (84%) of the subjects with initial PR interval >200 ms had a control ECG available from a follow-up visit a median of 6 years after the baseline examination. One hundred and thirty (71%) of these subjects still had prolonged PR interval (mean PR interval 229 ± 21 ms). These subjects with persistent PR prolongation were more likely male and had a slightly lower systolic blood pressure, but no significant differences in heart rate or other variables were observed between the groups. Markedly, prolonged PR interval >240 ms was present in 17 individuals. Three subjects had developed AF and one had probable trifascicular block (first-degree AV block and left bundle-branch block), but no second- or third-degree AV blocks or pacemaker rhythms were present.
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| PR interval (ms) | 155 ± 20 | 222 ± 17 | <0.001 |
| Males (%)a | 51.8 | 71.9 | <0.001 |
| Age (years)b | 43.9 ± 8.4 | 45.4 ± 8.7 | 0.01 |
| Current smoker (%)c | 34.1 | 29.5 | 0.12 |
| Cholesterol (mmol/L)c | 6.51 ± 1.32 | 6.36 ± 1.34 | 0.09 |
| BMI (kg/m2)c | 25.9 ± 3.8 | 26.6 ± 4.0 | 0.01 |
| Heart rate (b.p.m.)c | 76 ± 15 | 71 ± 14 | <0.001 |
| Systolic blood pressure (mmHg)c | 138 ± 21 | 139 ± 22 | 0.53 |
| Diastolic blood pressure (mmHg)c | 82 ± 12 | 82 ± 14 | 0.68 |
| Chronotropic medication (%)c | 4.2 | 8.8 | <0.001 |
| Cardiovascular disease (%)c | 7.9 | 12.9 | 0.005 |
| Electrocardiographic LVH (%)c | 31.3 | 36.2 | 0.11 |
| QTc duration (ms)c | 408 ± 27 | 406 ± 28 | 0.20 |
| QRS duration (ms)c | 87 ± 8 | 87 ± 8 | 0.18 |
| History of prior myocardial infarction (%)c | 1.1 | 1.5 | 0.57 |
| History of angina pectoris (%)c | 2.3 | 2.3 | 0.97 |
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| PR interval (ms) | 155 ± 20 | 222 ± 17 | <0.001 |
| Males (%)a | 51.8 | 71.9 | <0.001 |
| Age (years)b | 43.9 ± 8.4 | 45.4 ± 8.7 | 0.01 |
| Current smoker (%)c | 34.1 | 29.5 | 0.12 |
| Cholesterol (mmol/L)c | 6.51 ± 1.32 | 6.36 ± 1.34 | 0.09 |
| BMI (kg/m2)c | 25.9 ± 3.8 | 26.6 ± 4.0 | 0.01 |
| Heart rate (b.p.m.)c | 76 ± 15 | 71 ± 14 | <0.001 |
| Systolic blood pressure (mmHg)c | 138 ± 21 | 139 ± 22 | 0.53 |
| Diastolic blood pressure (mmHg)c | 82 ± 12 | 82 ± 14 | 0.68 |
| Chronotropic medication (%)c | 4.2 | 8.8 | <0.001 |
| Cardiovascular disease (%)c | 7.9 | 12.9 | 0.005 |
| Electrocardiographic LVH (%)c | 31.3 | 36.2 | 0.11 |
| QTc duration (ms)c | 408 ± 27 | 406 ± 28 | 0.20 |
| QRS duration (ms)c | 87 ± 8 | 87 ± 8 | 0.18 |
| History of prior myocardial infarction (%)c | 1.1 | 1.5 | 0.57 |
| History of angina pectoris (%)c | 2.3 | 2.3 | 0.97 |
LVH, electrocardiographic left ventricular hypertrophy according to the Sokolow–Lyon criteria. QTc, QT corrected for heart rate. To convert the values of cholesterol to milligrams per decilitre, divide by 0.02586. Data are presented as means ± SD.
aAdjusted for age.
bAdjusted for sex.
cAdjusted for age and sex.
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| PR interval (ms) | 155 ± 20 | 222 ± 17 | <0.001 |
| Males (%)a | 51.8 | 71.9 | <0.001 |
| Age (years)b | 43.9 ± 8.4 | 45.4 ± 8.7 | 0.01 |
| Current smoker (%)c | 34.1 | 29.5 | 0.12 |
| Cholesterol (mmol/L)c | 6.51 ± 1.32 | 6.36 ± 1.34 | 0.09 |
| BMI (kg/m2)c | 25.9 ± 3.8 | 26.6 ± 4.0 | 0.01 |
| Heart rate (b.p.m.)c | 76 ± 15 | 71 ± 14 | <0.001 |
| Systolic blood pressure (mmHg)c | 138 ± 21 | 139 ± 22 | 0.53 |
| Diastolic blood pressure (mmHg)c | 82 ± 12 | 82 ± 14 | 0.68 |
| Chronotropic medication (%)c | 4.2 | 8.8 | <0.001 |
| Cardiovascular disease (%)c | 7.9 | 12.9 | 0.005 |
| Electrocardiographic LVH (%)c | 31.3 | 36.2 | 0.11 |
| QTc duration (ms)c | 408 ± 27 | 406 ± 28 | 0.20 |
| QRS duration (ms)c | 87 ± 8 | 87 ± 8 | 0.18 |
| History of prior myocardial infarction (%)c | 1.1 | 1.5 | 0.57 |
| History of angina pectoris (%)c | 2.3 | 2.3 | 0.97 |
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| PR interval (ms) | 155 ± 20 | 222 ± 17 | <0.001 |
| Males (%)a | 51.8 | 71.9 | <0.001 |
| Age (years)b | 43.9 ± 8.4 | 45.4 ± 8.7 | 0.01 |
| Current smoker (%)c | 34.1 | 29.5 | 0.12 |
| Cholesterol (mmol/L)c | 6.51 ± 1.32 | 6.36 ± 1.34 | 0.09 |
| BMI (kg/m2)c | 25.9 ± 3.8 | 26.6 ± 4.0 | 0.01 |
| Heart rate (b.p.m.)c | 76 ± 15 | 71 ± 14 | <0.001 |
| Systolic blood pressure (mmHg)c | 138 ± 21 | 139 ± 22 | 0.53 |
| Diastolic blood pressure (mmHg)c | 82 ± 12 | 82 ± 14 | 0.68 |
| Chronotropic medication (%)c | 4.2 | 8.8 | <0.001 |
| Cardiovascular disease (%)c | 7.9 | 12.9 | 0.005 |
| Electrocardiographic LVH (%)c | 31.3 | 36.2 | 0.11 |
| QTc duration (ms)c | 408 ± 27 | 406 ± 28 | 0.20 |
| QRS duration (ms)c | 87 ± 8 | 87 ± 8 | 0.18 |
| History of prior myocardial infarction (%)c | 1.1 | 1.5 | 0.57 |
| History of angina pectoris (%)c | 2.3 | 2.3 | 0.97 |
LVH, electrocardiographic left ventricular hypertrophy according to the Sokolow–Lyon criteria. QTc, QT corrected for heart rate. To convert the values of cholesterol to milligrams per decilitre, divide by 0.02586. Data are presented as means ± SD.
aAdjusted for age.
bAdjusted for sex.
cAdjusted for age and sex.
PR interval and outcome events
The subjects were followed up for up to 35–41 years, depending on the time of the baseline visit.
During the follow-up period, 6073 (56.3%) of the participants died, 1948 of them due to cardiovascular causes (32.1% of all deaths). Seven hundred and eighty-nine subjects suffered SCD (40.5% of all cardiac deaths). In this population cohort, prolonged PR interval >200 ms was not associated with increased mortality after adjustments for age and sex. The results were not altered after multivariable-adjusted analyses (Table 2). Survival curves for all-cause and cardiovascular mortality, and SCD are presented in Figure 1.
Unadjusted and adjusted hazard ratios for death associated with prolonged PR interval
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| All-cause mortality | |||
| Number of deaths | 5933 | 140 | |
| Unadjusted HR (95% CI) | 1 | 1.28 (1.08–1.52) | 0.005 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.04 (0.88–1.23) | 0.67 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.05 (0.89–1.24) | 0.56 |
| Cardiovascular mortality | |||
| Number of deaths | 1904 | 44 | |
| Unadjusted HR (95% CI) | 1 | 1.24 (0.92–1.68) | 0.17 |
| Age- and sex-adjusted HR (95% CI) | 1 | 0.95 (0.71–1.29) | 0.75 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.94 (0.70–1.27) | 0.68 |
| Sudden cardiac death | |||
| Number of deaths | 766 | 23 | |
| Unadjusted HR (95% CI) | 1 | 1.59 (1.05–2.41) | 0.04 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.18 (0.78–1.78) | 0.46 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.16 (0.76–1.75) | 0.51 |
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| All-cause mortality | |||
| Number of deaths | 5933 | 140 | |
| Unadjusted HR (95% CI) | 1 | 1.28 (1.08–1.52) | 0.005 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.04 (0.88–1.23) | 0.67 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.05 (0.89–1.24) | 0.56 |
| Cardiovascular mortality | |||
| Number of deaths | 1904 | 44 | |
| Unadjusted HR (95% CI) | 1 | 1.24 (0.92–1.68) | 0.17 |
| Age- and sex-adjusted HR (95% CI) | 1 | 0.95 (0.71–1.29) | 0.75 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.94 (0.70–1.27) | 0.68 |
| Sudden cardiac death | |||
| Number of deaths | 766 | 23 | |
| Unadjusted HR (95% CI) | 1 | 1.59 (1.05–2.41) | 0.04 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.18 (0.78–1.78) | 0.46 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.16 (0.76–1.75) | 0.51 |
aAdjusted for age, sex, BMI, heart rate, chronotropic medication, and cardiovascular disease.
Unadjusted and adjusted hazard ratios for death associated with prolonged PR interval
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| All-cause mortality | |||
| Number of deaths | 5933 | 140 | |
| Unadjusted HR (95% CI) | 1 | 1.28 (1.08–1.52) | 0.005 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.04 (0.88–1.23) | 0.67 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.05 (0.89–1.24) | 0.56 |
| Cardiovascular mortality | |||
| Number of deaths | 1904 | 44 | |
| Unadjusted HR (95% CI) | 1 | 1.24 (0.92–1.68) | 0.17 |
| Age- and sex-adjusted HR (95% CI) | 1 | 0.95 (0.71–1.29) | 0.75 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.94 (0.70–1.27) | 0.68 |
| Sudden cardiac death | |||
| Number of deaths | 766 | 23 | |
| Unadjusted HR (95% CI) | 1 | 1.59 (1.05–2.41) | 0.04 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.18 (0.78–1.78) | 0.46 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.16 (0.76–1.75) | 0.51 |
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| All-cause mortality | |||
| Number of deaths | 5933 | 140 | |
| Unadjusted HR (95% CI) | 1 | 1.28 (1.08–1.52) | 0.005 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.04 (0.88–1.23) | 0.67 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.05 (0.89–1.24) | 0.56 |
| Cardiovascular mortality | |||
| Number of deaths | 1904 | 44 | |
| Unadjusted HR (95% CI) | 1 | 1.24 (0.92–1.68) | 0.17 |
| Age- and sex-adjusted HR (95% CI) | 1 | 0.95 (0.71–1.29) | 0.75 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.94 (0.70–1.27) | 0.68 |
| Sudden cardiac death | |||
| Number of deaths | 766 | 23 | |
| Unadjusted HR (95% CI) | 1 | 1.59 (1.05–2.41) | 0.04 |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.18 (0.78–1.78) | 0.46 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.16 (0.76–1.75) | 0.51 |
aAdjusted for age, sex, BMI, heart rate, chronotropic medication, and cardiovascular disease.
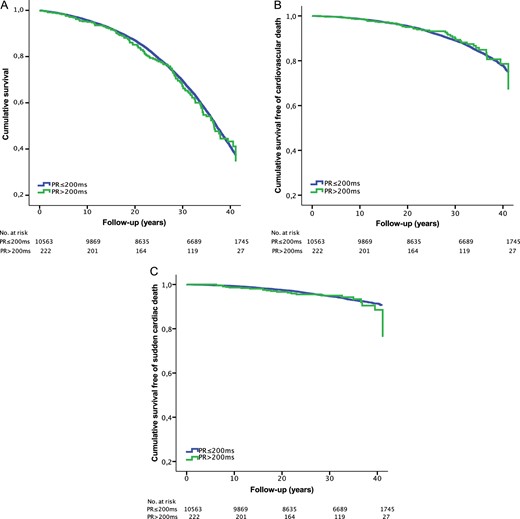
Age- and sex-adjusted survival plots for overall mortality (A), cardiovascular mortality (B), and sudden cardiac death (C) in subjects with prolonged PR interval.
The outcomes remained unchanged for each endpoint in the further analyses performed. First, we excluded all the individuals with AV nodal blocking medication and suspected cardiovascular disease. In these subjects with PR interval >200 ms, HRs for all-cause mortality, cardiovascular mortality, and SCD were 0.94 (95% CI: 0.77–1.14), 0.84 (95% CI: 0.58–1.20), and 1.18 (95% CI: 0.74–1.89), respectively (P = NS for all endpoints). Excluding the subjects with QRS duration ≥120 ms did not change these results. Secondly, we used the cut-off ≥220 ms used in some clinical studies to define a first-degree AV block. PR interval ≥220 ms was present in 123 subjects, but it was not associated with increased mortality either (HR: 1.10 for all-cause mortality, 95% CI: 0.88–1.37; HR: 1.01 for cardiovascular mortality, 95% CI: 0.88–1.37; HR: 1.25 for SCD, 95% CI: 0.72–2.16; P = NS for all endpoints). Thirdly, we studied if prolonged PR interval >200 ms predicts future hospitalizations due to CAD, heart failure (HF), AF, and stroke or transient ischaemic attack (TIA). As presented in Table 3, risk of hospitalizations of these subjects did not differ from the rest of the population. The outcome did not depend on the cut-off used to define prolonged PR interval, or on exclusion or inclusion of the subjects with cardiovascular disease or medication affecting the heart rate (P = NS for all endpoints). When subjects who presented with persistent PR prolongation (n = 130) were analysed separately, no differences in mortality or risk of future hospitalizations were observed (P = NS for all endpoints). Finally, we did an analysis restricted only to those with suspected cardiovascular disease (n = 861). In these subjects, prolonged PR interval >200 ms was associated with non-significant increase in mortality (HR: 1.40; 95% CI: 0.96–2.03; P = 0.09), but the number of individuals with prolonged PR interval and cardiovascular disease was small (n = 32).
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| Heart failure | |||
| Number of cases | 1673 | 43 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.27 (0.94–1.72) | 0.14 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.22 (0.90–1.65) | 0.22 |
| Coronary artery disease | |||
| Number of cases | 3465 | 74 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.02 (0.81–1.29) | 0.84 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.97 (0.77–1.22) | 0.80 |
| Atrial fibrillation | |||
| Number of cases | 1591 | 35 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.10 (0.79–1.55) | 0.57 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.03 (0.74–1.45) | 0.85 |
| TIA or stroke | |||
| Number of cases | 1877 | 50 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.30 (0.98–1.72) | 0.08 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.23 (0.92–1.62) | 0.17 |
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| Heart failure | |||
| Number of cases | 1673 | 43 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.27 (0.94–1.72) | 0.14 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.22 (0.90–1.65) | 0.22 |
| Coronary artery disease | |||
| Number of cases | 3465 | 74 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.02 (0.81–1.29) | 0.84 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.97 (0.77–1.22) | 0.80 |
| Atrial fibrillation | |||
| Number of cases | 1591 | 35 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.10 (0.79–1.55) | 0.57 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.03 (0.74–1.45) | 0.85 |
| TIA or stroke | |||
| Number of cases | 1877 | 50 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.30 (0.98–1.72) | 0.08 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.23 (0.92–1.62) | 0.17 |
aAdjusted for age, sex, BMI, heart rate, chronotropic medication, and cardiovascular disease.
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| Heart failure | |||
| Number of cases | 1673 | 43 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.27 (0.94–1.72) | 0.14 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.22 (0.90–1.65) | 0.22 |
| Coronary artery disease | |||
| Number of cases | 3465 | 74 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.02 (0.81–1.29) | 0.84 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.97 (0.77–1.22) | 0.80 |
| Atrial fibrillation | |||
| Number of cases | 1591 | 35 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.10 (0.79–1.55) | 0.57 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.03 (0.74–1.45) | 0.85 |
| TIA or stroke | |||
| Number of cases | 1877 | 50 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.30 (0.98–1.72) | 0.08 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.23 (0.92–1.62) | 0.17 |
| . | PR ≤200 ms . | PR >200 ms . | P-value . |
|---|---|---|---|
| (n = 10 563) . | (n = 222) . | ||
| Heart failure | |||
| Number of cases | 1673 | 43 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.27 (0.94–1.72) | 0.14 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.22 (0.90–1.65) | 0.22 |
| Coronary artery disease | |||
| Number of cases | 3465 | 74 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.02 (0.81–1.29) | 0.84 |
| Multivariate-adjusted HR (95% CI)a | 1 | 0.97 (0.77–1.22) | 0.80 |
| Atrial fibrillation | |||
| Number of cases | 1591 | 35 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.10 (0.79–1.55) | 0.57 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.03 (0.74–1.45) | 0.85 |
| TIA or stroke | |||
| Number of cases | 1877 | 50 | |
| Age- and sex-adjusted HR (95% CI) | 1 | 1.30 (0.98–1.72) | 0.08 |
| Multivariate-adjusted HR (95% CI)a | 1 | 1.23 (0.92–1.62) | 0.17 |
aAdjusted for age, sex, BMI, heart rate, chronotropic medication, and cardiovascular disease.
Discussion
Results of this large, prospective study with a long follow-up suggest that prolonged PR interval, or a first-degree AV block, is not associated with increased mortality or SCD in the middle-aged general population. Secondly, prolonged PR interval normalized in a substantial proportion of middle-aged subjects during the time course. Moreover, no excess in hospitalizations due to AF, stroke, or HF was associated with prolonged PR interval.
In most cases, prolonged PR interval is due to prolonged conduction in the AV node, which is profoundly influenced by changes in autonomic tone.15 However, the first-degree AV block can also be a sign of disturbed conduction in the His-Purkinje system, which is often associated with underlying heart disease, and can preclude higher-degree AV block and SCD.16–18 Previous studies on the prognostic significance of the first-degree AV block have mostly included young and healthy men from the military. In the first study on the natural course of prolonged PR interval involving 1000 young aviators from the US Army, no cardiac mortality or evidence of heart disease was demonstrated in the individuals with PR interval >200 ms during the 10-year follow-up, although 20% of the subjects died, mainly due to accidents and aerial combat.3 Subsequent studies conducted on over 18 000 male civil servants with a 5-year follow-up,6 and almost 4000 pilots recruited after World War II with a 30-year follow-up5 could not show any association between prolonged PR interval ≥220 ms and mortality or CAD, although some studies have provided somewhat contradictory evidence on the relation between PR interval and incidence of CAD.19,20
Only two major community-based studies have looked into the prognostic significance of the first-degree AV block in the general population. The first, conducted in the 1960s in Tecumseh, Michigan, involving 4678 participants, showed no excess incidence of cardiovascular disease or mortality among persons with PR interval ≥220 ms during the 4-year observation period, although PR interval correlated with cardiac abnormalities especially in persons past 60 years of age.7 However, the results of these previous studies have recently been challenged by an investigation of 7575 individuals from the Framingham Heart Study.9 In this population-based sample, PR interval >200 ms predicted all-cause mortality, with unadjusted HR of 2.7 and multivariable-adjusted HR of 1.4, during the follow-up of 20 years, and was significantly associated with pacemaker implantation and incidence of AF.
In the present study, PR interval >200 ms was not associated with increase in all-cause mortality or cardiovascular death during the 30-year follow-up of our middle-aged cohort, and, furthermore, no additional hospitalizations for heart failure, coronary disease, AF, or stroke were observed. Information on pacemaker implantation or AF not resulting in hospitalization was not systematically gathered throughout our study, so we cannot directly compare these incidence rates with those of the Framingham study.9 However, at the follow-up visit after 6 years, we observed few cases of AF in subjects with long PR interval, and AV block of higher degree was not detected on any of the subjects. Besides, if AF would have been substantially prevalent in the subjects with long PR interval, it could have been detected as higher hospitalization rates for AF, or as an increase in mortality and hospitalizations for HF or stroke, given the two-fold risk of death and over three-fold risk of HF and stroke generally associated with AF.21,22 The difference in mortality observed in the Framingham population and our study could be due to some methodological differences, but this seems unlikely since the cut-off for the first-degree AV block was the same in both studies, and even when we did analysis using a cut-off ≥220 ms to define prolonged PR interval, no differences in outcomes was noted. A more likely reason for the different results between these two large studies lies in different population samples. In the present study, subjects with prolonged PR interval were predominantly male and 1.5 years older than the rest of the population, hence when unadjusted analysis was used there seemed to be a slight difference in outcomes between the groups that disappeared after adjustments for age and sex. However, in the Framingham population individuals with prolonged PR interval were almost 10 years older than rest of the subjects, and also 10 years older than our population, thus underlying structural heart disease resulting in long PR interval or making it less tolerable would be more likely. Electrocardiographic manifestation of fibrosis and calcification of the cardiac conduction system associated with ageing can be prolongation of PR interval,23 and especially in the elderly, prolonged PR interval could precede a higher-degree AV block thus affecting the outcome. Prolonged PR intervals can also disturb left ventricular filling and cause diastolic mitral regurgitation, which may be important in patients with systolic or diastolic left ventricular dysfunction.24–26 This is supported by a recent study with an elderly population with CAD, in which the first-degree AV block was associated with increase in HF hospitalizations and cardiovascular mortality.2
In the present study, PR interval >200 ms was present in ∼2% of the individuals. This is in accordance with previous studies, although the reported prevalence of prolonged PR interval has varied depending on the population studied and the cut-off used to define first-degree AV block. Of healthy young adults aged 20–40 years, 0.5–1.5% have presented with prolonged PR interval, but the prevalence has increased to 2–3% in subjects of 40–60 years of age and even more thereafter.4–7,27 Among trained athletes, >10% may have prolonged PR interval >200 ms reflecting slow AV conduction mediated by increased parasympathetic tone and decreased resting sympathetic tone.28,29 It is likely, that among young individuals enhanced vagal tone is a major contributor to prolonged PR interval, while in older subjects prevalence of organic heart disease and fibrosis of the conduction system becomes more significant. There is also evidence of considerable genetic contribution to the cardiac conduction system, with 34% hereditability of PR interval reported.30,31 Several common genetic variants modulate heart rate, PR interval, QRS duration, and the risk of atrial arrhythmias,32,33 and in a recent report prolonged PR interval and other conduction abnormalities were highly prevalent among parents of children with an idiopathic congenital AV block.34
In our study, prolonged PR interval was normalized to ≤200 ms in almost 30% of the subjects during the first 6 years of follow-up. This is in accordance with previous studies, some of which have demonstrated that the persistence of the first-degree AV block has been <50% at least in some age groups.5,7 This could be at least partly due to decreased vagal tone associated with ageing. Besides, PR interval shows a significant circadian variation,35 which depends on the prevailing autonomic tone affecting AV conduction. However, excluding the subjects in whom PR interval was normalized during the follow-up did not alter our results.
Several limitations of the present study deserve attention. The study was not designed for non-inferiority, so although no statistically significant level of adverse events were observed with subjects having prolonged PR interval, it is possible that with a larger sample size some differences between the groups could have been demonstrated. The prevalence of AF was based on hospitalization data only, which is likely to underestimate potential association between prolonged PR interval and AF episodes. It is also well known, that heart rate and PR interval have inverse relationship, with PR becoming shorter with increasing heart rate and vice versa,36 thus the cut-off of >200 ms to define prolonged PR interval can be affected by present heart rate. It has also been suggested, that using the post-exercise assessment of AV conduction may improve cardiovascular risk prediction with better unmasking functional abnormalities of the heart.37 Nevertheless, similarly to clinical practice, a protocol of taking single resting 12-lead ECG and using PR interval cut-off >200 ms to define prolongation was employed in this study.
In conclusion, our findings indicate that in the middle-aged population, prolonged PR interval is a partially transient phenomenon, and not associated with an increased risk of hospitalization, overall mortality, or SCD. It is possible, however, that the prognosis of prolonged PR interval is not as favourable in the elderly, or when cardiac disease or other electrocardiographic conduction disturbances are present. Further studies are needed to better define the group of patients in whom the detection of prolonged PR interval adds additional information to the conventional risk stratification.
Funding
This work was supported by a scholarship from the Finnish Foundation for Cardiovascular Research, and by a grant from the Sigrid Juselius Foundation, Helsinki, Finland (HVH).
Conflict of interest: none declared.
References
- atrial fibrillation
- electrocardiogram
- coronary arteriosclerosis
- sudden cardiac death
- first degree atrioventricular block
- p-r interval
- prolonged p-r interval
- cerebrovascular accident
- ischemic stroke
- heart failure
- cardiovascular system
- follow-up
- middle-aged adult
- mortality
- patient prognosis
- cardiovascular death
- surrogate endpoints



