-
PDF
- Split View
-
Views
-
Cite
Cite
Erdinc Soylu, Leanne Harling, Hutan Ashrafian, Christopher Rao, Roberto Casula, Thanos Athanasiou, A systematic review of the safety and efficacy of distal coronary artery anastomotic devices, European Journal of Cardio-Thoracic Surgery, Volume 49, Issue 3, March 2016, Pages 732–745, https://doi.org/10.1093/ejcts/ezv179
Close - Share Icon Share
Abstract
Interest in minimally invasive and off-pump cardiac surgical techniques has promoted the development of automated distal anastomotic devices (DADs) to facilitate construction of coronary artery anastomosis. Several DADs have been proposed for potential use in coronary surgery. However, a number of technical failures and uncertainty around both short-term morbidity and long-term patency have limited the generalized uptake of these devices. A systematic literature search identified 28 studies, incorporating 970 patients who underwent coronary artery bypass grafting using a DAD. Eight different devices were identified including Heartflo, St Jude, U-clip, vessel closure system, C-port, magnetic vascular positioner and coronary anastomosis coupler. Thirty-day mortality, cardiac-specific mortality and myocardial infarction were equal between DADs and hand-sewn cases (1.3, 0.3 and 0.8%, respectively). The overall proportion of postoperative haemorrhage was higher in the anastomotic device group (2.3%) than in the group with hand-sewn anastomoses (1.5%) although not statistically significant. Overall graft patency was 97.2% at <1 month, 94.6% at 1–3 months and 92.3% at >3 months. Of the currently available systems, the U-clip device was found to provide the best overall postoperative outcomes, which included a patency of 96.1% at >3months. The current literature is limited by its predominantly observational study design and lack of directly comparative studies. Furthermore, inter-study variation in patient selection, anticoagulation strategies and follow-up periods prevents quantitative comparison. Future research necessitates multicentre randomized, controlled studies to provide a direct comparison of current and future anastomotic device systems with established hand-sewn techniques in both the short and long term.
INTRODUCTION
The past decade has seen an increase in the number of older patients with multiple comorbidities referred for coronary revascularization surgery. Through minimizing the adverse effects of cardiopulmonary bypass and reducing surgical trauma, technological advances such as off-pump coronary artery bypass (OPCAB) and minimally invasive direct coronary artery bypass (MIDCAB) have provided some benefits in these high-risk patients. However, these advancements have created other challenges owing to the increased technical demand and the prolonged surgical learning curve associated with such procedures. In particular, ineffective stabilization and haemodynamic impairment during OPCAB surgery may complicate coronary anastomosis and lead to incomplete revascularization [ 1 ]. Similarly, the limited surgical exposure afforded during MIDCAB may increase anastomotic time and prolong myocardial ischaemia [ 2 ].
Since Alexis Carrel's first description of a hand-sewn coronary anastomosis [ 3 ], it has remained the ‘gold standard’ surgical technique. However, an automated simple and rapid distal anastomotic method that preserves the quality of the anastomosis both in the short- and long term remains lacking [ 2 ]. The ability to create a device that could perform a reproducible, patent and reliable microvascular anastomosis would not only potentiate more global uptake of OPCAB surgery, but may also permit grafting to previously inaccessible posterior vessels, facilitating a drive towards totally endoscopic surgical revascularization (TECAB). Importantly, such a device would also reduce ischaemic time [ 4 ] and establish the uniformity of graft quality and patency, a factor particularly important in patients with poor quality targets [ 5 , 6 ].
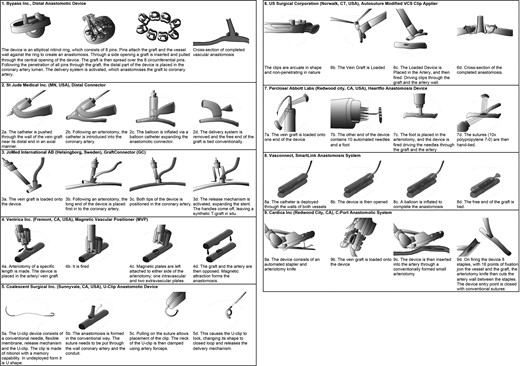
However, despite these potential benefits, the high degree of variability in coronary anatomy and pathology makes development of novel coronary anastomotic devices extremely challenging. Any universally successful device must accommodate for the diversity in location and extent of calcified plaques as well as changeability in the tortuosity and accessibility of the coronary vessel [ 7 , 8 ]. As a result, a diverse range of devices has been developed, utilizing an equally varied spectrum of methodologies (Fig. 1 ). The purpose of this study is therefore to provide a quantitative summary of the evidence surrounding the use of coronary anastomotic devices in humans. Our primary aim is to evaluate the effect of each technique on long-term graft patency. Secondarily, we consider the impact these technologies have on mortality and major postoperative morbidities both in the early and late postoperative period.
LITERATURE SEARCH CRITERIA
An electronic search was performed using MEDLINE, Ovid, EMBASE, Cochrane and the UK National Library for Health databases using the board search terms ‘coronary artery anastomosis devices’ and the following MeSH terms: ‘coronary vessels’ OR ‘coronary’ AND ‘vessels’ OR ‘coronary vessels’ OR ‘coronary’ AND ‘artery’ OR ‘coronary artery’ AND anastomosis AND ‘instrumentation’ OR ‘instrumentation’ OR ‘devices’ OR ‘equipment and supplies’ OR ‘equipment’ AND ‘supplies’ OR ‘equipment and supplies’. Articles were also identified using the ‘related articles’ function in MEDLINE and screening of the reference lists of manuscripts identified in the original search. Studies were excluded if they reported solely results from animal or in vitro testing. In the case of duplicate publication, only the most recent study was included. Owing to the small number of studies per device, those studies reporting concomitant procedures were not excluded but are discussed in our overall interpretation of results.
Data extraction was performed according to a predefined protocol by two independent reviewers (Erdinc Soylu and Leanne Harling). Short- and long-term outcomes were assessed. Short-term outcomes included: (i) 30-day mortality, (ii) 30-day major cardiac and cerebrovascular events, (iii) postoperative haemorrhage and (iv) other clinical morbidity. Long-term outcomes included: (i) mortality at the last follow-up, (ii) angiographic patency at the last follow-up and (iv) clinical outcomes at the last follow-up. The last search date was 1 June 2014.
STATISTICAL METHODS
Comparison of proportions was carried out using Fisher's exact or the χ2 test, as appropriate, to allow unweighted statistical pooling of outcome data between device and hand-sewn anastomoses across the included studies. Analysis was performed using WinPepi Version 11.32.
ANASTOMOTIC DEVICE TYPES
A summary of anastomotic device types is shown in Fig. 1 .
Magnetic vascular positioner
The magnetic vascular positioner (MVP) (Ventrica, Inc., Freemont, CA, USA) uses two sets of three magnetic gold-plated clips to create a side-to-side anastamosis. Each set of clips comprises one intravascular and two extravascular components mounted on a delivery device [ 9 , 10 ]. In order to perform the anastomosis, a longitudinal arteriotomy is made in the graft and its internal diameter measured. The distal end of the intravascular delivery device is introduced and deployed such that the two extravascular clips sandwich the vessel wall between intra- and extravascular components. This procedure is then repeated with the target vessel, and the two clip complexes brought into close proximity to be secured by magnetic attraction. Finally, the distal end of the conduit is ligated, creating a functional side-to-side anastomosis.
Heartflo
The Heartflo (Perclose/Abbott Labs, Redwood city, CA, USA) may perform both end-to-side and side-to-side anastomoses. It simultaneously delivers 10 interrupted 7-0 polypropylene interrupted sutures through the target and conduit vessel wall using a hydraulically activated mechanism. To perform the anastomosis, the proximal needle guide of the mechanism is inserted into the conduit with the foot of the device placed through the target vessel arteriotomy. When fired, the suture needles are driven simultaneously through the target and conduit walls, 1–2 mm from the arteriotomy edge. These sutures are then sorted and tied in a conventional manner [ 11 ].
St Jude distal connector
The St Jude distal anastomotic device (DAD) consists of a balloon-expandable ring-shaped stainless steel connector attached to a delivery system. The external fingers of the connector secure the distal vein graft, and the internal fingers secure the coronary artery lumen [ 12 ]. To perform the anastomosis, the vein conduit is prepared using the preformed cutting device and dilator. This creates an opening in the vein 1 cm from its distal end, allowing the delivery system to be passed through the distal end of the vein, and out of the opening. This engages the external fingers of the device on the conduit endothelium. The same is performed on the target vessel and the delivery system with the conduit attached is passed through the arteriotomy until the graft opposes the coronary artery. With the delivery device in the coronary artery, the nose cone is advanced allowing the internal fingers to engage the coronary artery endothelium. The delivery system is then oriented at 90° to the target vessel, and the balloon inflated to expand the connector and create the anastomosis. The delivery system is then removed and the distal vein graft stump ligated [ 12 ].
U-clip
The U-Clip device (Coalescent Surgical, Inc., Sunnyvale, CA, USA) allows the creation of an interrupted anastomosis while avoiding the need to tie multiple sutures. The device consists of a self-closing nitinol clip attached to a suture needle by a flexible and detachable membrane. To create the anastomosis, the conduit and coronary artery are prepared in a conventional manner. The suture needle is held with regular needle holders and used to pierce the conduit and target as routinely performed. The conduit and coronary artery are then approximated with the open clip at the intended suture point. This allows the surgeon to maintain complete control over the alignment of tissues. Compression of a 1-mm long release mechanism at the junction of the clip and flexible membrane causes detachment of the clip and a switch from a U-shape to its original closed loop configuration. This sequence is repeated to create the interrupted anastomosis [ 13 ].
Vessel closure system
The vessel closure system (VCS; US Surgical Corporation, Norwalk, CT, USA) utilizes multiple titanium microclips to create an interrupted anastomosis. To perform the anastomosis, the graft and target vessel walls are everted with forceps before application of the clip. A pincer movement on the clip applicator deforms the clip shoulders against stationary jaws, thus creating the anastomosis. The device design creates uniform clip closure and also allows for mal-positioned clips to be easily removed with specially made clip-releasing forceps [ 14 ].
Distal anastomotic device
The DAD (Bypass, Inc.) is a coupling device consisting of an elliptical nitinol ring with 8 pins. The device is designed in two sizes to adapt to the graft's external diameter (2–3.5 and 3–6 mm). To perform the anastomosis, the graft is inserted through the side opening on the delivery capsule, with the DAD device in its distal end. The graft is then pulled through the central opening on the device with a snare and its distal end spread over the eight circumferential pins. The switch at the base of the device is turned to push forward and converge the pins, which, after a change in the device handle set, enable device insertion though the coronary arteriotomy. When all the converged pins are in the coronary vessel, the handles are squeezed causing the pins to diverge circumferentially, completing the anastomosis [ 15 ].
C-port anastomotic system
The C-port distal anastomosis system (Cardica, Inc., Redwood City, CA, USA) creates a sutureless vascular end-to-side anastomosis. To perform the anastomosis, the graft is inserted between two cartridge arms of the device and attached to four spikes (two for the heel and two for the toe). The surgeon then creates a small coronary arteriotomy, through which the anvil of the C-port is inserted. The device is then deployed approximating the cartridge onto the coronary artery against the anvil inside the coronary vessel with eight separate stainless steel clips. The knife within the anvil is simultaneously deployed, cutting the coronary artery from the inside out, thus creating the arteriotomy and the anastomotic lumen between the coronary artery and the graft. The C-port cartridge is then unclamped and removed. A separate suture is often used to occlude the anvil insertion hole and occasional further sutures to ensure haemostasis at the toe and heel [ 16 , 17 ].
Coronary anastomosis coupler
The coronary anastomosis coupler (CAC) device (Converge Medical, Inc., Sunnyvale, CA, USA) consists of concentric mating nitinol frames that create an anastomosis through clamping. To perform the anastomosis, the graft is sandwiched between the frames of the device by initially placing the graft over the inner frame and then placing the outer frame over its distal end. The graft is then mounted on the delivery tool and an arteriotomy performed in the target vessel. The coupler is inserted into the coronary lumen and released from the delivery tool, allowing the deflected parts of the coupler to return to their original shape and expanding the coupler device against the coronary wall to create the anastomosis [ 18 ].
RESULTS
Description of studies
A total of 28 studies [ 1 , 2 , 5 , 6 , 8–10 , 13 , 14 , 16–34 ], incorporating 940 patients, reported outcomes for the use of DADs during coronary artery bypass graft (CABG) surgery (Table 1 ). Fifteen animal-only studies were identified but subsequently excluded from the analysis [ 1 , 4 , 7 , 11 , 12 , 15 , 35–43 ]. The postoperative results are presented in Tables 2 and 3 . The most widely-used anastomotic device was the C-port device (359 cases) followed by the U-clip device (291 cases). The most commonly used graft was an internal mammary artery (474 cases) followed by saphenous vein (460 cases), radial artery (41 cases) and right gastroepiploic artery (14 cases). In 59 cases, the conduit type was not specified. Ten studies reported the use of anastomotic devices during on-pump CABG (ONCAB) [ 6 , 10 , 14 , 18 , 22–24 , 26 , 27 , 32 ]; nine employed this technique in solely off-pump (OPCAB) cases [ 1 , 9 , 13 , 19 , 20 , 25 , 28 , 29 , 34 ]; eight studies performed a combination of OPCAB and ONCAB procedures [ 1 , 2 , 8 , 16 , 17 , 21 , 30 , 33 ] and, in one study, it was unclear whether an ONCAB or OPCAB method was employed. In 14 studies, the operative method (i.e. open CABG vs MIDCAB or TECAB) was not disclosed [ 6 , 8 , 16 , 18 , 19 , 22–24 , 26 , 31 , 32 , 34 ]. The majority of cases were performed through median sternotomy; however, two studies utilized anastomotic devices to facilitate TECAB surgery [ 20 , 29 ] and three studies reported their use in a mixture of minimally invasive and open procedures [ 13 , 30 , 33 ].
| Study . | Device . | Study type . | n . | Age . | Gender (M:F) . | Inclusion . | Exclusion . | On/off pump . | Incision . | Graft . | Target . | Anticoag. . | Device anastomosis time (min) . | Follow-up (weeks) . | Outcomes . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Klima et al. [ 1 ] | MVP | Case series | 32 | 65 ± 9 | 27:5 | c, e, f | A1, A2, A3, A4, A5 | 26 On, 6 Off. | Median sternotomy | a1, a2 | b1, b2, b3, b4, b5 | A, B, C, D | 2.28 ± 1.32 | 4 | 4 |
| Klima et al. [ 5 ] | MVP | Case series | 11 | 60.3 ± 11.0 | 6:4 | c, d, f | A1, A2, A3, A4, A5 | Off | MIDCAB | a1 | b3 | A, B, C, D | 3.32 ± 3.18 | 26 | 1,4 |
| Casselman et al. [ 9 ] | MVP | Case series | 2 | 75.5 ± 0.7 | – | – | – | Off | Median sternotomy | a1, a2 | b3, b5 | A, C, D | <3 | 1 | 1 |
| Vicol et al. [ 10 ] | MVP | Case series | 11 | 59.7 ± 10.7 | 10:1 | c, f | A2, A6 | On | Median sternotomy | a1, a2, a3, a4 | b1, b3, b4, b5 | B, C, D | 13.5 ± 2.9 | 76 | 1 |
| Athanasiou et al. [ 2 ] | MVP | Case series | 12 | 64.8 ± 8.7 | – | a | A1, A2, A6, A7 | 3 On 9 Off | Median sternotomy | a1 | b3 | A, B, C, D | 5.6 ± 1.99 | 17 | 1,4 |
| Klima et al. [ 25 ] | MVP | Case report | 1 | 69 | 1:0 | – | – | Off | Median sternotomy | a1, a3, a4 | b1, b3, b6 | A, C | <1.5 | 10 | 1,4 |
| Martens et al. [ 6 ] | Heartflo | Case series | 60 | – | – | – | A1, A3, A4, A5, A13 | On | – | a1, a2 | b1, b2, b3, b6, b7 | – | Group1: 19 ± 0.3 Group 2: 15.6 ± 2 ( P = 0.0003) | – | 1,4 |
| Tozzi et al. [ 31 ] | Heartflo | Case series | 11 | 64 ± 3 | 7:4 | e, g, h, i | A3, A4, A7, A10, A14, A15 | – | – | a2, a5 | b1, b3, b5, b8 | – | 17.7 ± 2 | 26 | 4 |
| Wiklund et al. [ 32 ] | St Jude | RCT | 60 | 69 St Jude 67 hand-sewn | – | j | A1, A3, A4, A8, A9, A10, A11, A12 | On | – | a2 | b1, b2, b4, b5, b9 | B | 2.25 ± 0.18 (loading) <1 (deployment) | 26 | 1,4 |
| Carrel et al. [ 22 ] | St Jude | Case series | 32 | 67 ± 4.5 | 28:4 | – | A7 | On | – | a2 | b1, b2, b5, b7 | B, D | 6–8 (loading) <2 (deployment) | 52 | 1 |
| Eckstein et al. [ 24 ] | St Jude | Case series | 19 | – | – | – | – | On | – | a2 | b1, b2, b5 | – | 6–8 (loading) <2 (deployment) | 12 | 1 |
| Eckstein et al. [ 23 ] | St Jude | Case report | 1 | 61 | 1:0 | – | – | On | – | a2 | b1 | – | – | 1 | 1 |
| Morishige et al. [ 28 ] | U-clip | Case series | 118 | 69.5 ± 8 | 92:26 | – | – | Off | Median sternotomy | a1, a3, a4, a6 | b1, b3, b6 | B | 7.3 ± 2.1 (end-to-side) 6.3 ± 2.2 (side–side) | 64 | 1 |
| Caskey et al. [ 13 ] | U-clip | Case series | 18 | 64 | 18:0 | – | A7, A8, A10, A16, A17, A18, A19, A20, A21, A22 | Off | Median sternotomy = 17 (94%) MIDCAB = 1 (6%) | a1 | b3 | – | 8.6 ± 2.7 | 24 | 1 |
| Mayuga et al. [ 27 ] | U-clip | RCT | 30 | 70.4 ± 8.1 U-clips 65.3 ± 11.8 hand-sewn | 12:3 U-clip 18:7 hand-sewn | a, b, g | – | On | Median sternotomy | a1 | b3 | – | – | – | 3 |
| Wolf et al. [ 33 ] | U-Clip | Case series | 82 | 65.2 | 70:12 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | 12 On 70 Off | Median sternotomy = 70/82 (85.4%) MIDCAB = 12/82 (14.6%) | a1 | b3 | – | 12.4 | 28 | 1 |
| Shemin et al. [ 8 ] | U-Clip | Case series | 197 | 64 ± 10 U-clip 67 ± 10 hand-sewn | 40:19 | – | – | On/off | – | – | – | B | 10 | 20 | 4 |
| Ono et al. [ 30 ] | U-Clip | Case series | 13 | 64.5 ± 9.1 | 9:4 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | On/off | Median sternotomy/MIDCAB | a1 | b3 | B | 15.9 ± 5.5 | 28 | 1,4 |
| Nishida et al. [ 29 ] | U-clip | Case report | 1 | 72 | 1:0 | – | – | Off | TECAB | a1 | b3 | – | 20 min | 8 | 4 |
| Nataf et al. [ 14 ] | VCS | Case series | 10 | – | – | – | – | On | – | a1, a2 | b1, b2, b3, b4 | – | 15 | 40 | 1,4 |
| Lisi et al. [ 26 ] | VCS | Case series | 7 | 49–75 | – | – | – | On | – | a2 | b1, b2, b4, b5 | – | 12–15 | 1.4 | 1,4 |
| Kim et al. [ 34 ] | DAD | Case series | 14 | 65 ± 7 | 10:4 | – | – | Off | – | a2, a5, a6 | b1, b2, b5, | – | 2.9 ± 0.7 | 1 | 1 |
| Matschke et al. [ 16 ] | C-Port | NRCT | 130 | 68.5 ± 7.7 | 111:19 | b, I, h | A4, A8, A13, A21, A27, | On/off | – | a2 | b1, b4, b6 | – | – | 48 | 1,4 |
| Verberkmoes et al. [ 17 ] | C-Port | RCT | 71 | – | – | c, e, i, n | A2, A3, A4, A5, A8, A10, A11, A12, A13, A15, A21, A22 | On/off | Median sternotomy | a1, a2 | b1, b2, b4, b7, b8 | B | – | 56 | 1,4 |
| Balkhy et al. [ 19 ] | C-**port | Case series | 24 | 63 ± 5.1 | 23:1 | a, m | – | Off | – | – | – | – | – | 18 | 1,4 |
| Balkhy et al. [ 20 ] | C-port | Case series | 120 | 63 ± 10.4 | 86:34 | – | – | Off | TECAB | a1, a3 | b1, b3, b4, b6 | – | – | 29 | 1,4 |
| Cai et al. [ 21 ] | C-port | Case series | 50 | 68 ± 9.7 C-Port 65.5 ± 10.9 hand-sewn | – | – | – | On/off | Median sternotomy | a2 | b2, b4, b5 | B, D | – | 12 | 1,4 |
| Boening et al. [ 18 ] | CAC | Case series | 37 | 63.6 ± 7.5 | – | l | A7 | On | – | – | – | B, D | 4.8 ± 4.4 (loading) 1.8 ± 1.2 (deployment) | 8 | 1,4 |
| Study . | Device . | Study type . | n . | Age . | Gender (M:F) . | Inclusion . | Exclusion . | On/off pump . | Incision . | Graft . | Target . | Anticoag. . | Device anastomosis time (min) . | Follow-up (weeks) . | Outcomes . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Klima et al. [ 1 ] | MVP | Case series | 32 | 65 ± 9 | 27:5 | c, e, f | A1, A2, A3, A4, A5 | 26 On, 6 Off. | Median sternotomy | a1, a2 | b1, b2, b3, b4, b5 | A, B, C, D | 2.28 ± 1.32 | 4 | 4 |
| Klima et al. [ 5 ] | MVP | Case series | 11 | 60.3 ± 11.0 | 6:4 | c, d, f | A1, A2, A3, A4, A5 | Off | MIDCAB | a1 | b3 | A, B, C, D | 3.32 ± 3.18 | 26 | 1,4 |
| Casselman et al. [ 9 ] | MVP | Case series | 2 | 75.5 ± 0.7 | – | – | – | Off | Median sternotomy | a1, a2 | b3, b5 | A, C, D | <3 | 1 | 1 |
| Vicol et al. [ 10 ] | MVP | Case series | 11 | 59.7 ± 10.7 | 10:1 | c, f | A2, A6 | On | Median sternotomy | a1, a2, a3, a4 | b1, b3, b4, b5 | B, C, D | 13.5 ± 2.9 | 76 | 1 |
| Athanasiou et al. [ 2 ] | MVP | Case series | 12 | 64.8 ± 8.7 | – | a | A1, A2, A6, A7 | 3 On 9 Off | Median sternotomy | a1 | b3 | A, B, C, D | 5.6 ± 1.99 | 17 | 1,4 |
| Klima et al. [ 25 ] | MVP | Case report | 1 | 69 | 1:0 | – | – | Off | Median sternotomy | a1, a3, a4 | b1, b3, b6 | A, C | <1.5 | 10 | 1,4 |
| Martens et al. [ 6 ] | Heartflo | Case series | 60 | – | – | – | A1, A3, A4, A5, A13 | On | – | a1, a2 | b1, b2, b3, b6, b7 | – | Group1: 19 ± 0.3 Group 2: 15.6 ± 2 ( P = 0.0003) | – | 1,4 |
| Tozzi et al. [ 31 ] | Heartflo | Case series | 11 | 64 ± 3 | 7:4 | e, g, h, i | A3, A4, A7, A10, A14, A15 | – | – | a2, a5 | b1, b3, b5, b8 | – | 17.7 ± 2 | 26 | 4 |
| Wiklund et al. [ 32 ] | St Jude | RCT | 60 | 69 St Jude 67 hand-sewn | – | j | A1, A3, A4, A8, A9, A10, A11, A12 | On | – | a2 | b1, b2, b4, b5, b9 | B | 2.25 ± 0.18 (loading) <1 (deployment) | 26 | 1,4 |
| Carrel et al. [ 22 ] | St Jude | Case series | 32 | 67 ± 4.5 | 28:4 | – | A7 | On | – | a2 | b1, b2, b5, b7 | B, D | 6–8 (loading) <2 (deployment) | 52 | 1 |
| Eckstein et al. [ 24 ] | St Jude | Case series | 19 | – | – | – | – | On | – | a2 | b1, b2, b5 | – | 6–8 (loading) <2 (deployment) | 12 | 1 |
| Eckstein et al. [ 23 ] | St Jude | Case report | 1 | 61 | 1:0 | – | – | On | – | a2 | b1 | – | – | 1 | 1 |
| Morishige et al. [ 28 ] | U-clip | Case series | 118 | 69.5 ± 8 | 92:26 | – | – | Off | Median sternotomy | a1, a3, a4, a6 | b1, b3, b6 | B | 7.3 ± 2.1 (end-to-side) 6.3 ± 2.2 (side–side) | 64 | 1 |
| Caskey et al. [ 13 ] | U-clip | Case series | 18 | 64 | 18:0 | – | A7, A8, A10, A16, A17, A18, A19, A20, A21, A22 | Off | Median sternotomy = 17 (94%) MIDCAB = 1 (6%) | a1 | b3 | – | 8.6 ± 2.7 | 24 | 1 |
| Mayuga et al. [ 27 ] | U-clip | RCT | 30 | 70.4 ± 8.1 U-clips 65.3 ± 11.8 hand-sewn | 12:3 U-clip 18:7 hand-sewn | a, b, g | – | On | Median sternotomy | a1 | b3 | – | – | – | 3 |
| Wolf et al. [ 33 ] | U-Clip | Case series | 82 | 65.2 | 70:12 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | 12 On 70 Off | Median sternotomy = 70/82 (85.4%) MIDCAB = 12/82 (14.6%) | a1 | b3 | – | 12.4 | 28 | 1 |
| Shemin et al. [ 8 ] | U-Clip | Case series | 197 | 64 ± 10 U-clip 67 ± 10 hand-sewn | 40:19 | – | – | On/off | – | – | – | B | 10 | 20 | 4 |
| Ono et al. [ 30 ] | U-Clip | Case series | 13 | 64.5 ± 9.1 | 9:4 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | On/off | Median sternotomy/MIDCAB | a1 | b3 | B | 15.9 ± 5.5 | 28 | 1,4 |
| Nishida et al. [ 29 ] | U-clip | Case report | 1 | 72 | 1:0 | – | – | Off | TECAB | a1 | b3 | – | 20 min | 8 | 4 |
| Nataf et al. [ 14 ] | VCS | Case series | 10 | – | – | – | – | On | – | a1, a2 | b1, b2, b3, b4 | – | 15 | 40 | 1,4 |
| Lisi et al. [ 26 ] | VCS | Case series | 7 | 49–75 | – | – | – | On | – | a2 | b1, b2, b4, b5 | – | 12–15 | 1.4 | 1,4 |
| Kim et al. [ 34 ] | DAD | Case series | 14 | 65 ± 7 | 10:4 | – | – | Off | – | a2, a5, a6 | b1, b2, b5, | – | 2.9 ± 0.7 | 1 | 1 |
| Matschke et al. [ 16 ] | C-Port | NRCT | 130 | 68.5 ± 7.7 | 111:19 | b, I, h | A4, A8, A13, A21, A27, | On/off | – | a2 | b1, b4, b6 | – | – | 48 | 1,4 |
| Verberkmoes et al. [ 17 ] | C-Port | RCT | 71 | – | – | c, e, i, n | A2, A3, A4, A5, A8, A10, A11, A12, A13, A15, A21, A22 | On/off | Median sternotomy | a1, a2 | b1, b2, b4, b7, b8 | B | – | 56 | 1,4 |
| Balkhy et al. [ 19 ] | C-**port | Case series | 24 | 63 ± 5.1 | 23:1 | a, m | – | Off | – | – | – | – | – | 18 | 1,4 |
| Balkhy et al. [ 20 ] | C-port | Case series | 120 | 63 ± 10.4 | 86:34 | – | – | Off | TECAB | a1, a3 | b1, b3, b4, b6 | – | – | 29 | 1,4 |
| Cai et al. [ 21 ] | C-port | Case series | 50 | 68 ± 9.7 C-Port 65.5 ± 10.9 hand-sewn | – | – | – | On/off | Median sternotomy | a2 | b2, b4, b5 | B, D | – | 12 | 1,4 |
| Boening et al. [ 18 ] | CAC | Case series | 37 | 63.6 ± 7.5 | – | l | A7 | On | – | – | – | B, D | 4.8 ± 4.4 (loading) 1.8 ± 1.2 (deployment) | 8 | 1,4 |
Device—GC: graft connector; MVP: magnetic vascular positioner; DAD: distal anastomotic device.
Inclusion criteria—a: primary CABG; b: non-emergent; c: good quality target vessels; d: single-vessel disease; e: multivessel disease; f: high-grade stenosis; g: CABG only; h: reasonable LVEF (>25%); i: age >18 or woman not pregnant; j: coronary artery outer diameter >2.5 mm; k: BMI <35 kg/m 2 ; l: coronary artery inner diameter ≥2 mm; m: LIMA vessel size >2.5 mm; n : other.
Exclusion criteria—A1: poor LVEF; A2: contraindication to antiplatelet therapy; A3: emergent CABG; A4: redo CABG; A5: other concomitant cardiac procedure; A6: need for postoperative MRI; A7: poor target (calcified: narrow etc.); A8: recent neurological event; A9: COPD; A10: renal failure; A11: pregnancy; A12: need for chronic anticoagulation; A13: need for IABP; A14: recent MI; A15: haemodynamic instability; A16: contraindication to use of LIMA; A17: GI bleed; A18: severe anaemia; A19: short life expectancy; A20: severe hypertension; A21: CCF; A22: infection; A23: previous anaphylaxis to angiographic contrast media; A24: severe systemic disease; A24: history of pericarditis: median sternotomy or chest irradiation; A25: uncontrollable diabetes within 7 days; A26: vasculitis; A27: bleeding diathesis; A28: history of IVDU within a prior year.
Graft—a1: left internal mammary artery; a2: saphenous vein graft; a3: right internal mammary artery; a4: radial artery; a5: unspecified internal thoracic artery; a6: right gastroepiploic artery
Target—b1: right coronary artery; b2: PDA: posterior descending coronary artery; b3: left anterior descending coronary artery; b4: diagonal coronary artery; b5: marginal coronary artery; b6: circumflex coronary artery; b7: posterolateral artery coronary artery; b8: obtuse marginal coronary artery; b9: intermediate coronary artery.
Anticoagulation—A: preop aspirin; B: postop aspirin; C: preop clopidogrel; D: postop clopidogrel; E: preop ticlopidine; F: postop ticlopidine; G: postop dipyridamole.
Outcomes—1: angiogram; 2: histology; 3: flow measurements; 4: clinical; 5: compliance.
CAC: coronary anastomosis coupler; MIDCAB; minimally invasive direct coronary artery bypass; VCS: vessel closure system; TECAB: totally endoscopic coronary artery bypass; CABG: coronary artery bypass graft; MI: myocardial Infarction; LVEF: left ventricular ejection fraction; COPD: chronic obstructive pulmonary disease; CCF: congestive cardiac failure; IABP: intra-aortic balloon pump; IVDU: intravenous drug use; LIMA: left internal mammary artery; NRCT: non-randomised controlled trial; RCT: randomised controlled trial.
| Study . | Device . | Study type . | n . | Age . | Gender (M:F) . | Inclusion . | Exclusion . | On/off pump . | Incision . | Graft . | Target . | Anticoag. . | Device anastomosis time (min) . | Follow-up (weeks) . | Outcomes . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Klima et al. [ 1 ] | MVP | Case series | 32 | 65 ± 9 | 27:5 | c, e, f | A1, A2, A3, A4, A5 | 26 On, 6 Off. | Median sternotomy | a1, a2 | b1, b2, b3, b4, b5 | A, B, C, D | 2.28 ± 1.32 | 4 | 4 |
| Klima et al. [ 5 ] | MVP | Case series | 11 | 60.3 ± 11.0 | 6:4 | c, d, f | A1, A2, A3, A4, A5 | Off | MIDCAB | a1 | b3 | A, B, C, D | 3.32 ± 3.18 | 26 | 1,4 |
| Casselman et al. [ 9 ] | MVP | Case series | 2 | 75.5 ± 0.7 | – | – | – | Off | Median sternotomy | a1, a2 | b3, b5 | A, C, D | <3 | 1 | 1 |
| Vicol et al. [ 10 ] | MVP | Case series | 11 | 59.7 ± 10.7 | 10:1 | c, f | A2, A6 | On | Median sternotomy | a1, a2, a3, a4 | b1, b3, b4, b5 | B, C, D | 13.5 ± 2.9 | 76 | 1 |
| Athanasiou et al. [ 2 ] | MVP | Case series | 12 | 64.8 ± 8.7 | – | a | A1, A2, A6, A7 | 3 On 9 Off | Median sternotomy | a1 | b3 | A, B, C, D | 5.6 ± 1.99 | 17 | 1,4 |
| Klima et al. [ 25 ] | MVP | Case report | 1 | 69 | 1:0 | – | – | Off | Median sternotomy | a1, a3, a4 | b1, b3, b6 | A, C | <1.5 | 10 | 1,4 |
| Martens et al. [ 6 ] | Heartflo | Case series | 60 | – | – | – | A1, A3, A4, A5, A13 | On | – | a1, a2 | b1, b2, b3, b6, b7 | – | Group1: 19 ± 0.3 Group 2: 15.6 ± 2 ( P = 0.0003) | – | 1,4 |
| Tozzi et al. [ 31 ] | Heartflo | Case series | 11 | 64 ± 3 | 7:4 | e, g, h, i | A3, A4, A7, A10, A14, A15 | – | – | a2, a5 | b1, b3, b5, b8 | – | 17.7 ± 2 | 26 | 4 |
| Wiklund et al. [ 32 ] | St Jude | RCT | 60 | 69 St Jude 67 hand-sewn | – | j | A1, A3, A4, A8, A9, A10, A11, A12 | On | – | a2 | b1, b2, b4, b5, b9 | B | 2.25 ± 0.18 (loading) <1 (deployment) | 26 | 1,4 |
| Carrel et al. [ 22 ] | St Jude | Case series | 32 | 67 ± 4.5 | 28:4 | – | A7 | On | – | a2 | b1, b2, b5, b7 | B, D | 6–8 (loading) <2 (deployment) | 52 | 1 |
| Eckstein et al. [ 24 ] | St Jude | Case series | 19 | – | – | – | – | On | – | a2 | b1, b2, b5 | – | 6–8 (loading) <2 (deployment) | 12 | 1 |
| Eckstein et al. [ 23 ] | St Jude | Case report | 1 | 61 | 1:0 | – | – | On | – | a2 | b1 | – | – | 1 | 1 |
| Morishige et al. [ 28 ] | U-clip | Case series | 118 | 69.5 ± 8 | 92:26 | – | – | Off | Median sternotomy | a1, a3, a4, a6 | b1, b3, b6 | B | 7.3 ± 2.1 (end-to-side) 6.3 ± 2.2 (side–side) | 64 | 1 |
| Caskey et al. [ 13 ] | U-clip | Case series | 18 | 64 | 18:0 | – | A7, A8, A10, A16, A17, A18, A19, A20, A21, A22 | Off | Median sternotomy = 17 (94%) MIDCAB = 1 (6%) | a1 | b3 | – | 8.6 ± 2.7 | 24 | 1 |
| Mayuga et al. [ 27 ] | U-clip | RCT | 30 | 70.4 ± 8.1 U-clips 65.3 ± 11.8 hand-sewn | 12:3 U-clip 18:7 hand-sewn | a, b, g | – | On | Median sternotomy | a1 | b3 | – | – | – | 3 |
| Wolf et al. [ 33 ] | U-Clip | Case series | 82 | 65.2 | 70:12 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | 12 On 70 Off | Median sternotomy = 70/82 (85.4%) MIDCAB = 12/82 (14.6%) | a1 | b3 | – | 12.4 | 28 | 1 |
| Shemin et al. [ 8 ] | U-Clip | Case series | 197 | 64 ± 10 U-clip 67 ± 10 hand-sewn | 40:19 | – | – | On/off | – | – | – | B | 10 | 20 | 4 |
| Ono et al. [ 30 ] | U-Clip | Case series | 13 | 64.5 ± 9.1 | 9:4 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | On/off | Median sternotomy/MIDCAB | a1 | b3 | B | 15.9 ± 5.5 | 28 | 1,4 |
| Nishida et al. [ 29 ] | U-clip | Case report | 1 | 72 | 1:0 | – | – | Off | TECAB | a1 | b3 | – | 20 min | 8 | 4 |
| Nataf et al. [ 14 ] | VCS | Case series | 10 | – | – | – | – | On | – | a1, a2 | b1, b2, b3, b4 | – | 15 | 40 | 1,4 |
| Lisi et al. [ 26 ] | VCS | Case series | 7 | 49–75 | – | – | – | On | – | a2 | b1, b2, b4, b5 | – | 12–15 | 1.4 | 1,4 |
| Kim et al. [ 34 ] | DAD | Case series | 14 | 65 ± 7 | 10:4 | – | – | Off | – | a2, a5, a6 | b1, b2, b5, | – | 2.9 ± 0.7 | 1 | 1 |
| Matschke et al. [ 16 ] | C-Port | NRCT | 130 | 68.5 ± 7.7 | 111:19 | b, I, h | A4, A8, A13, A21, A27, | On/off | – | a2 | b1, b4, b6 | – | – | 48 | 1,4 |
| Verberkmoes et al. [ 17 ] | C-Port | RCT | 71 | – | – | c, e, i, n | A2, A3, A4, A5, A8, A10, A11, A12, A13, A15, A21, A22 | On/off | Median sternotomy | a1, a2 | b1, b2, b4, b7, b8 | B | – | 56 | 1,4 |
| Balkhy et al. [ 19 ] | C-**port | Case series | 24 | 63 ± 5.1 | 23:1 | a, m | – | Off | – | – | – | – | – | 18 | 1,4 |
| Balkhy et al. [ 20 ] | C-port | Case series | 120 | 63 ± 10.4 | 86:34 | – | – | Off | TECAB | a1, a3 | b1, b3, b4, b6 | – | – | 29 | 1,4 |
| Cai et al. [ 21 ] | C-port | Case series | 50 | 68 ± 9.7 C-Port 65.5 ± 10.9 hand-sewn | – | – | – | On/off | Median sternotomy | a2 | b2, b4, b5 | B, D | – | 12 | 1,4 |
| Boening et al. [ 18 ] | CAC | Case series | 37 | 63.6 ± 7.5 | – | l | A7 | On | – | – | – | B, D | 4.8 ± 4.4 (loading) 1.8 ± 1.2 (deployment) | 8 | 1,4 |
| Study . | Device . | Study type . | n . | Age . | Gender (M:F) . | Inclusion . | Exclusion . | On/off pump . | Incision . | Graft . | Target . | Anticoag. . | Device anastomosis time (min) . | Follow-up (weeks) . | Outcomes . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Klima et al. [ 1 ] | MVP | Case series | 32 | 65 ± 9 | 27:5 | c, e, f | A1, A2, A3, A4, A5 | 26 On, 6 Off. | Median sternotomy | a1, a2 | b1, b2, b3, b4, b5 | A, B, C, D | 2.28 ± 1.32 | 4 | 4 |
| Klima et al. [ 5 ] | MVP | Case series | 11 | 60.3 ± 11.0 | 6:4 | c, d, f | A1, A2, A3, A4, A5 | Off | MIDCAB | a1 | b3 | A, B, C, D | 3.32 ± 3.18 | 26 | 1,4 |
| Casselman et al. [ 9 ] | MVP | Case series | 2 | 75.5 ± 0.7 | – | – | – | Off | Median sternotomy | a1, a2 | b3, b5 | A, C, D | <3 | 1 | 1 |
| Vicol et al. [ 10 ] | MVP | Case series | 11 | 59.7 ± 10.7 | 10:1 | c, f | A2, A6 | On | Median sternotomy | a1, a2, a3, a4 | b1, b3, b4, b5 | B, C, D | 13.5 ± 2.9 | 76 | 1 |
| Athanasiou et al. [ 2 ] | MVP | Case series | 12 | 64.8 ± 8.7 | – | a | A1, A2, A6, A7 | 3 On 9 Off | Median sternotomy | a1 | b3 | A, B, C, D | 5.6 ± 1.99 | 17 | 1,4 |
| Klima et al. [ 25 ] | MVP | Case report | 1 | 69 | 1:0 | – | – | Off | Median sternotomy | a1, a3, a4 | b1, b3, b6 | A, C | <1.5 | 10 | 1,4 |
| Martens et al. [ 6 ] | Heartflo | Case series | 60 | – | – | – | A1, A3, A4, A5, A13 | On | – | a1, a2 | b1, b2, b3, b6, b7 | – | Group1: 19 ± 0.3 Group 2: 15.6 ± 2 ( P = 0.0003) | – | 1,4 |
| Tozzi et al. [ 31 ] | Heartflo | Case series | 11 | 64 ± 3 | 7:4 | e, g, h, i | A3, A4, A7, A10, A14, A15 | – | – | a2, a5 | b1, b3, b5, b8 | – | 17.7 ± 2 | 26 | 4 |
| Wiklund et al. [ 32 ] | St Jude | RCT | 60 | 69 St Jude 67 hand-sewn | – | j | A1, A3, A4, A8, A9, A10, A11, A12 | On | – | a2 | b1, b2, b4, b5, b9 | B | 2.25 ± 0.18 (loading) <1 (deployment) | 26 | 1,4 |
| Carrel et al. [ 22 ] | St Jude | Case series | 32 | 67 ± 4.5 | 28:4 | – | A7 | On | – | a2 | b1, b2, b5, b7 | B, D | 6–8 (loading) <2 (deployment) | 52 | 1 |
| Eckstein et al. [ 24 ] | St Jude | Case series | 19 | – | – | – | – | On | – | a2 | b1, b2, b5 | – | 6–8 (loading) <2 (deployment) | 12 | 1 |
| Eckstein et al. [ 23 ] | St Jude | Case report | 1 | 61 | 1:0 | – | – | On | – | a2 | b1 | – | – | 1 | 1 |
| Morishige et al. [ 28 ] | U-clip | Case series | 118 | 69.5 ± 8 | 92:26 | – | – | Off | Median sternotomy | a1, a3, a4, a6 | b1, b3, b6 | B | 7.3 ± 2.1 (end-to-side) 6.3 ± 2.2 (side–side) | 64 | 1 |
| Caskey et al. [ 13 ] | U-clip | Case series | 18 | 64 | 18:0 | – | A7, A8, A10, A16, A17, A18, A19, A20, A21, A22 | Off | Median sternotomy = 17 (94%) MIDCAB = 1 (6%) | a1 | b3 | – | 8.6 ± 2.7 | 24 | 1 |
| Mayuga et al. [ 27 ] | U-clip | RCT | 30 | 70.4 ± 8.1 U-clips 65.3 ± 11.8 hand-sewn | 12:3 U-clip 18:7 hand-sewn | a, b, g | – | On | Median sternotomy | a1 | b3 | – | – | – | 3 |
| Wolf et al. [ 33 ] | U-Clip | Case series | 82 | 65.2 | 70:12 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | 12 On 70 Off | Median sternotomy = 70/82 (85.4%) MIDCAB = 12/82 (14.6%) | a1 | b3 | – | 12.4 | 28 | 1 |
| Shemin et al. [ 8 ] | U-Clip | Case series | 197 | 64 ± 10 U-clip 67 ± 10 hand-sewn | 40:19 | – | – | On/off | – | – | – | B | 10 | 20 | 4 |
| Ono et al. [ 30 ] | U-Clip | Case series | 13 | 64.5 ± 9.1 | 9:4 | h, I, k | A8.A10, A17, A22, A19, A18, A20, A21, A7, A23, A25, A26, A27, A28 | On/off | Median sternotomy/MIDCAB | a1 | b3 | B | 15.9 ± 5.5 | 28 | 1,4 |
| Nishida et al. [ 29 ] | U-clip | Case report | 1 | 72 | 1:0 | – | – | Off | TECAB | a1 | b3 | – | 20 min | 8 | 4 |
| Nataf et al. [ 14 ] | VCS | Case series | 10 | – | – | – | – | On | – | a1, a2 | b1, b2, b3, b4 | – | 15 | 40 | 1,4 |
| Lisi et al. [ 26 ] | VCS | Case series | 7 | 49–75 | – | – | – | On | – | a2 | b1, b2, b4, b5 | – | 12–15 | 1.4 | 1,4 |
| Kim et al. [ 34 ] | DAD | Case series | 14 | 65 ± 7 | 10:4 | – | – | Off | – | a2, a5, a6 | b1, b2, b5, | – | 2.9 ± 0.7 | 1 | 1 |
| Matschke et al. [ 16 ] | C-Port | NRCT | 130 | 68.5 ± 7.7 | 111:19 | b, I, h | A4, A8, A13, A21, A27, | On/off | – | a2 | b1, b4, b6 | – | – | 48 | 1,4 |
| Verberkmoes et al. [ 17 ] | C-Port | RCT | 71 | – | – | c, e, i, n | A2, A3, A4, A5, A8, A10, A11, A12, A13, A15, A21, A22 | On/off | Median sternotomy | a1, a2 | b1, b2, b4, b7, b8 | B | – | 56 | 1,4 |
| Balkhy et al. [ 19 ] | C-**port | Case series | 24 | 63 ± 5.1 | 23:1 | a, m | – | Off | – | – | – | – | – | 18 | 1,4 |
| Balkhy et al. [ 20 ] | C-port | Case series | 120 | 63 ± 10.4 | 86:34 | – | – | Off | TECAB | a1, a3 | b1, b3, b4, b6 | – | – | 29 | 1,4 |
| Cai et al. [ 21 ] | C-port | Case series | 50 | 68 ± 9.7 C-Port 65.5 ± 10.9 hand-sewn | – | – | – | On/off | Median sternotomy | a2 | b2, b4, b5 | B, D | – | 12 | 1,4 |
| Boening et al. [ 18 ] | CAC | Case series | 37 | 63.6 ± 7.5 | – | l | A7 | On | – | – | – | B, D | 4.8 ± 4.4 (loading) 1.8 ± 1.2 (deployment) | 8 | 1,4 |
Device—GC: graft connector; MVP: magnetic vascular positioner; DAD: distal anastomotic device.
Inclusion criteria—a: primary CABG; b: non-emergent; c: good quality target vessels; d: single-vessel disease; e: multivessel disease; f: high-grade stenosis; g: CABG only; h: reasonable LVEF (>25%); i: age >18 or woman not pregnant; j: coronary artery outer diameter >2.5 mm; k: BMI <35 kg/m 2 ; l: coronary artery inner diameter ≥2 mm; m: LIMA vessel size >2.5 mm; n : other.
Exclusion criteria—A1: poor LVEF; A2: contraindication to antiplatelet therapy; A3: emergent CABG; A4: redo CABG; A5: other concomitant cardiac procedure; A6: need for postoperative MRI; A7: poor target (calcified: narrow etc.); A8: recent neurological event; A9: COPD; A10: renal failure; A11: pregnancy; A12: need for chronic anticoagulation; A13: need for IABP; A14: recent MI; A15: haemodynamic instability; A16: contraindication to use of LIMA; A17: GI bleed; A18: severe anaemia; A19: short life expectancy; A20: severe hypertension; A21: CCF; A22: infection; A23: previous anaphylaxis to angiographic contrast media; A24: severe systemic disease; A24: history of pericarditis: median sternotomy or chest irradiation; A25: uncontrollable diabetes within 7 days; A26: vasculitis; A27: bleeding diathesis; A28: history of IVDU within a prior year.
Graft—a1: left internal mammary artery; a2: saphenous vein graft; a3: right internal mammary artery; a4: radial artery; a5: unspecified internal thoracic artery; a6: right gastroepiploic artery
Target—b1: right coronary artery; b2: PDA: posterior descending coronary artery; b3: left anterior descending coronary artery; b4: diagonal coronary artery; b5: marginal coronary artery; b6: circumflex coronary artery; b7: posterolateral artery coronary artery; b8: obtuse marginal coronary artery; b9: intermediate coronary artery.
Anticoagulation—A: preop aspirin; B: postop aspirin; C: preop clopidogrel; D: postop clopidogrel; E: preop ticlopidine; F: postop ticlopidine; G: postop dipyridamole.
Outcomes—1: angiogram; 2: histology; 3: flow measurements; 4: clinical; 5: compliance.
CAC: coronary anastomosis coupler; MIDCAB; minimally invasive direct coronary artery bypass; VCS: vessel closure system; TECAB: totally endoscopic coronary artery bypass; CABG: coronary artery bypass graft; MI: myocardial Infarction; LVEF: left ventricular ejection fraction; COPD: chronic obstructive pulmonary disease; CCF: congestive cardiac failure; IABP: intra-aortic balloon pump; IVDU: intravenous drug use; LIMA: left internal mammary artery; NRCT: non-randomised controlled trial; RCT: randomised controlled trial.
| Study . | Device . | n . | Mortality (30-day) . | Postoperative MI . | Postoperative CVA . | Postoperative haemorrhage . | Causes of death . | Other morbidity . |
|---|---|---|---|---|---|---|---|---|
| Klima | MVP | 32 | 1/32 (3.1%) | 1/32 (3.1%) (non-MVP graft stenosis) | 0 (0%) | 3/32 (9.3%) (2 non-specific, 1 from hand-sewn anastamosis) | Low CO syndrome | AF = 2/31 (6.5%) Re-exploration for bleeding = 3 (9.3%) ARDS = 1/32 (3.1%) Pneumonia = 1/31 (3.2%) TIA = 1/32 (3.1%) Leg wound infection = 1/31 (3.2%) |
| Klima | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | – | Wound infection = 1/10 (10%) ITU stay (days) = 1.4 ± 0.4 Hospital stay (days) = 6.4 ± 1.2 |
| Casselman | MVP | 2 | 0/2 (0%) | – | – | – | – | – |
| Vicol | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 1/11 (9.1%) (non-specific) | – | Ventilation (h) = 16.5 ± 12 ITU stay (days) = 2.1 ± 0.7 |
| Athanasiou | MVP | 12 | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | – | VF = 1/12 (8.3%) Re-exploration = 1/12 (8.3%) Blood Loss = 914 ± 234 ml Visual defect = 1/12 (8.3%) Hospital stay (days) = 5.8 ± 1.2 (NS difference to routine CABG patients) |
| Klima | MVP | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | – | – |
| Martens | Heartflo | 60 | 1/60 (1.7%) | 0/60 (0%) | 1/60 (1.7%) | 1/60 (1.7%) Non-device-related from group 1 | Non-cardiac death = 1/60 (1.7%) | – |
| Tozzi | Heartflo | 11 | 0/11 (0%) | 0/11 (0%) | – | 0/11 (0%) | – | – |
| Wiklund | St Jude | 60 | 0/30 (0%) St Jude 1/30 (3.3%) hand-sewn | – | 0 (0%) St Jude 1/30 (3.3%) hand-sewn | 1/28 (3.6%) St Jude non-device-related bleed 0 (0%) hand-sewn | Arrhythmia in hand-sewn group = 1/30 (3.3%) | – |
| Carrel | St Jude | 32 | 1/32 (3.1%) | 1/32 (3.1%) | 1/32 (3.1%) | 0/32 (0%) | Neurological injury = 1/32 (3.1%) | Localized coronary dissection = 1/32 (3.1%) |
| Eckstein | St Jude | 19 | 0/19 (0%) | 0/19 (0%) | 0/19 (0%) | – | – | – |
| Eckstein | St Jude | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0 /1 (0%) | – | – |
| Morishige | U-Clip | 118 | 1/118 (0.8%) | 0/118 (0%) | 1/118 (0.8%) | – | – | IABP = 6 (5.1%) |
| Caskey | U-Clip | 18 | 0/18 (0%) | 1/18 (5.5%) unrelated to device | 0/18 (0%) | 0 /18 (0%) | – | Arrhythmias (unrelated to device) = 7 (38.9%) Pleural effusion = 1/18 (5.5%) TIA (unrelated to device) = 1/18 (5.5%) ITU stay (days) = 1.9 ± 0.05 Hospital stay (days) = 5 |
| Mayuga | U-clip | 30 | – | – | – | – | – | – |
| Wolf | U-clip | 59 | 2/82 (2.4%) | 1/82 (1.2%) | 0/82 (0%) | 1/82 (1.2%) non-device-related | Duodenal perforation = 1/82 (1.2%) Respiratory failure = 1/82 (1.2%) | Arrhythmia = 2/82 (2.4%) Pleural effusion = 1/82 (1.2%) TIA = 1/82 (1.2%) |
| Shemin | U-Clip | 197 | 1/59 (1.2%) U-clip 1/138 (0.7%) hand-sewn | 0/59 (0%) U-clip 0/138 (0%) hand-sewn | 0/59 (0%) U-Clip 0/138 (0%) hand-sewn | – | U-clip: respiratory failure (non-device-related) (1) hand-sewn: Multi-organ failure (1), Sepsis (1) | AF = 17% U-Clip group versus 22% hand-sewn group ( P = 0.38) Reoperation for bleeding = 2% U-Clip group versus 1.4% hand-sewn group ( P = 0.89) Blood transfusion (u) = 1.3 ± 1.5 U-Clip group versus 1.2 ± 1.7 hand-sewn group ( P = 0.82) Renal failure = 2% U-clip group versus 1% hand-sewn group ( P = 0.79) Sternal infection = 0% U-clip group versus 3% hand-sewn group ( P = 0.31) Ventilation time (h) = 5.0 ± 1.6 U-Clip group versus 5.3 ± 1.4 hand-sewn group ( P = 0.73) Length of stay (days) = 5.5 ± 1.7 U-clip group versus 5.9 ± 2.1 hand-sewn group ( P = 0.47) |
| Ono | U-clip | 13 | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | – | AF = 2/13 (15.4%) Inotropic support = 2/13 (15.4%) Blood transfusion (u) = 4/13 (30.8%) ITU stay (days) = 0.86 ± 0.16 Hospital stay (days) = 3.9 |
| Nishida | U-clip | 1 | 0/1 (0%) | – | – | – | – | Hospital stay (days) = 5 |
| Nataf | VCS | 10 | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | – | – |
| Lisi | VCS | 7 | 0/7 (0%) | 0/7 (0%) | 0/7 (0%) | 1 /7 (14.3%) Non-device-related | – | Reoperation for bleeding = 1/7 (14.3%) |
| Kim | DAD | 14 | 0/14 (0%) | – | – | – | – | – |
| Matschke | C-port | 130 | 3/130 (2.3%) | 0/130 (0%) | – | – | Right ventricular failure = 1 Myocardial infarction = 1 Adult respiratory distress syndrome = 1 | Reoperation for bleeding = 0 (0%) |
| Verberkmoes | C-Port | 71 | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 2/35 (6%) C-port 2/36 (6%) hand-sewn | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 1/35 (3%) C-port 1/36 (3%) hand-sewn | – | AF = 7 (20%) versus 6 (17%) P = 0.76 Reoperation for bleeding = 1/35 (3%) C-port versus 1/36 (3%) hand-sewn Prolonged ionotropics or IABP 2 (6%) C-port versus 2 (6%) hand-sewn P = 1 Pulmonary complications = 4 (11%) C-port versus 3 (8%) hand-sewn P = 0.71 Prolonged ventilation 1 (3%) C-port versus 1 (3%) hand-sewn P = 1 Renal complications = 2 (6%) C-port versus 0 (0%) hand-sewn P = 0.24 Deep wound infection = 1 (3%) C-port versus 0 (0%) hand-sewn P = 0.49 |
| Balkhy | C-Port | 24 | 0/24 (0%) | 0/24 (0%) | 1/25 (4%) | 1/25 (4%) | – | Reoperation for bleeding = 1/25 (4%) Renal failure = 3/25 (12%) Postoperative stay = 4.2 days |
| Balkhy | C-port | 120 | 1/120 (0.8%) | 1/120 (0.8%) | 1/120 (0.8%) | 2/120 (1.6%) | – | Pericardial effusion = 1/120 (0.8%) Brachial artery embolization = 1/120 (0.8%) Pleural effusion requiring intervention = 2/120 (1.6%) Phrenic nerve palsy = 1/120 (0.8%) Wound infection = 0 (0%) Prolonged hospitalization = 2/120 (1.6%) Hospital stay (days) = 3.3 ± 2.4 |
| Cai | C-port | 50 | 1/50 (2%) C-port 3/193 (1.6%) hand-sewn | 0/50 (0%) C-port 1/193 (0.5%) hand-sewn | 0/50 (0%) C-port 0/193 (0%) hand-sewn | – | Unknown cause = 1 | AF = 5/50 (10%) C-port 27/193 (14%) hand-sewn Cardiac tamponade = 0 (0%) C-port 0 (0%) hand-sewn Blood products = 23/50 (46%) C-port 74/193 (38.3%) hand-sewn Reoperative bleeding = 2/50 (4%) C-port 6/193 (3.1%) hand-sewn Pneumonia = 2/50 (4%) C-port 3/193 (1.6%) hand-sewn Renal failure = 0 (0%) C-port 6/193 (3.1%) hand-sewn GI complications = 0 (0%) C-Port 4/193 (2.1%) hand-sewn Septicaemia = 0 (0%) C-port 0 (0%) hand-sewn Sternal infection = 0 (0%) C-port 0 (0%) hand-sewn Prolonged ventilation = 1/50 (2%) C-port 10/193 (5.2%) hand-sewn |
| Boening | CAC | 37 | 0/37 (0%) | 0/37 (0%) | – | – | – |
| Study . | Device . | n . | Mortality (30-day) . | Postoperative MI . | Postoperative CVA . | Postoperative haemorrhage . | Causes of death . | Other morbidity . |
|---|---|---|---|---|---|---|---|---|
| Klima | MVP | 32 | 1/32 (3.1%) | 1/32 (3.1%) (non-MVP graft stenosis) | 0 (0%) | 3/32 (9.3%) (2 non-specific, 1 from hand-sewn anastamosis) | Low CO syndrome | AF = 2/31 (6.5%) Re-exploration for bleeding = 3 (9.3%) ARDS = 1/32 (3.1%) Pneumonia = 1/31 (3.2%) TIA = 1/32 (3.1%) Leg wound infection = 1/31 (3.2%) |
| Klima | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | – | Wound infection = 1/10 (10%) ITU stay (days) = 1.4 ± 0.4 Hospital stay (days) = 6.4 ± 1.2 |
| Casselman | MVP | 2 | 0/2 (0%) | – | – | – | – | – |
| Vicol | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 1/11 (9.1%) (non-specific) | – | Ventilation (h) = 16.5 ± 12 ITU stay (days) = 2.1 ± 0.7 |
| Athanasiou | MVP | 12 | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | – | VF = 1/12 (8.3%) Re-exploration = 1/12 (8.3%) Blood Loss = 914 ± 234 ml Visual defect = 1/12 (8.3%) Hospital stay (days) = 5.8 ± 1.2 (NS difference to routine CABG patients) |
| Klima | MVP | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | – | – |
| Martens | Heartflo | 60 | 1/60 (1.7%) | 0/60 (0%) | 1/60 (1.7%) | 1/60 (1.7%) Non-device-related from group 1 | Non-cardiac death = 1/60 (1.7%) | – |
| Tozzi | Heartflo | 11 | 0/11 (0%) | 0/11 (0%) | – | 0/11 (0%) | – | – |
| Wiklund | St Jude | 60 | 0/30 (0%) St Jude 1/30 (3.3%) hand-sewn | – | 0 (0%) St Jude 1/30 (3.3%) hand-sewn | 1/28 (3.6%) St Jude non-device-related bleed 0 (0%) hand-sewn | Arrhythmia in hand-sewn group = 1/30 (3.3%) | – |
| Carrel | St Jude | 32 | 1/32 (3.1%) | 1/32 (3.1%) | 1/32 (3.1%) | 0/32 (0%) | Neurological injury = 1/32 (3.1%) | Localized coronary dissection = 1/32 (3.1%) |
| Eckstein | St Jude | 19 | 0/19 (0%) | 0/19 (0%) | 0/19 (0%) | – | – | – |
| Eckstein | St Jude | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0 /1 (0%) | – | – |
| Morishige | U-Clip | 118 | 1/118 (0.8%) | 0/118 (0%) | 1/118 (0.8%) | – | – | IABP = 6 (5.1%) |
| Caskey | U-Clip | 18 | 0/18 (0%) | 1/18 (5.5%) unrelated to device | 0/18 (0%) | 0 /18 (0%) | – | Arrhythmias (unrelated to device) = 7 (38.9%) Pleural effusion = 1/18 (5.5%) TIA (unrelated to device) = 1/18 (5.5%) ITU stay (days) = 1.9 ± 0.05 Hospital stay (days) = 5 |
| Mayuga | U-clip | 30 | – | – | – | – | – | – |
| Wolf | U-clip | 59 | 2/82 (2.4%) | 1/82 (1.2%) | 0/82 (0%) | 1/82 (1.2%) non-device-related | Duodenal perforation = 1/82 (1.2%) Respiratory failure = 1/82 (1.2%) | Arrhythmia = 2/82 (2.4%) Pleural effusion = 1/82 (1.2%) TIA = 1/82 (1.2%) |
| Shemin | U-Clip | 197 | 1/59 (1.2%) U-clip 1/138 (0.7%) hand-sewn | 0/59 (0%) U-clip 0/138 (0%) hand-sewn | 0/59 (0%) U-Clip 0/138 (0%) hand-sewn | – | U-clip: respiratory failure (non-device-related) (1) hand-sewn: Multi-organ failure (1), Sepsis (1) | AF = 17% U-Clip group versus 22% hand-sewn group ( P = 0.38) Reoperation for bleeding = 2% U-Clip group versus 1.4% hand-sewn group ( P = 0.89) Blood transfusion (u) = 1.3 ± 1.5 U-Clip group versus 1.2 ± 1.7 hand-sewn group ( P = 0.82) Renal failure = 2% U-clip group versus 1% hand-sewn group ( P = 0.79) Sternal infection = 0% U-clip group versus 3% hand-sewn group ( P = 0.31) Ventilation time (h) = 5.0 ± 1.6 U-Clip group versus 5.3 ± 1.4 hand-sewn group ( P = 0.73) Length of stay (days) = 5.5 ± 1.7 U-clip group versus 5.9 ± 2.1 hand-sewn group ( P = 0.47) |
| Ono | U-clip | 13 | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | – | AF = 2/13 (15.4%) Inotropic support = 2/13 (15.4%) Blood transfusion (u) = 4/13 (30.8%) ITU stay (days) = 0.86 ± 0.16 Hospital stay (days) = 3.9 |
| Nishida | U-clip | 1 | 0/1 (0%) | – | – | – | – | Hospital stay (days) = 5 |
| Nataf | VCS | 10 | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | – | – |
| Lisi | VCS | 7 | 0/7 (0%) | 0/7 (0%) | 0/7 (0%) | 1 /7 (14.3%) Non-device-related | – | Reoperation for bleeding = 1/7 (14.3%) |
| Kim | DAD | 14 | 0/14 (0%) | – | – | – | – | – |
| Matschke | C-port | 130 | 3/130 (2.3%) | 0/130 (0%) | – | – | Right ventricular failure = 1 Myocardial infarction = 1 Adult respiratory distress syndrome = 1 | Reoperation for bleeding = 0 (0%) |
| Verberkmoes | C-Port | 71 | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 2/35 (6%) C-port 2/36 (6%) hand-sewn | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 1/35 (3%) C-port 1/36 (3%) hand-sewn | – | AF = 7 (20%) versus 6 (17%) P = 0.76 Reoperation for bleeding = 1/35 (3%) C-port versus 1/36 (3%) hand-sewn Prolonged ionotropics or IABP 2 (6%) C-port versus 2 (6%) hand-sewn P = 1 Pulmonary complications = 4 (11%) C-port versus 3 (8%) hand-sewn P = 0.71 Prolonged ventilation 1 (3%) C-port versus 1 (3%) hand-sewn P = 1 Renal complications = 2 (6%) C-port versus 0 (0%) hand-sewn P = 0.24 Deep wound infection = 1 (3%) C-port versus 0 (0%) hand-sewn P = 0.49 |
| Balkhy | C-Port | 24 | 0/24 (0%) | 0/24 (0%) | 1/25 (4%) | 1/25 (4%) | – | Reoperation for bleeding = 1/25 (4%) Renal failure = 3/25 (12%) Postoperative stay = 4.2 days |
| Balkhy | C-port | 120 | 1/120 (0.8%) | 1/120 (0.8%) | 1/120 (0.8%) | 2/120 (1.6%) | – | Pericardial effusion = 1/120 (0.8%) Brachial artery embolization = 1/120 (0.8%) Pleural effusion requiring intervention = 2/120 (1.6%) Phrenic nerve palsy = 1/120 (0.8%) Wound infection = 0 (0%) Prolonged hospitalization = 2/120 (1.6%) Hospital stay (days) = 3.3 ± 2.4 |
| Cai | C-port | 50 | 1/50 (2%) C-port 3/193 (1.6%) hand-sewn | 0/50 (0%) C-port 1/193 (0.5%) hand-sewn | 0/50 (0%) C-port 0/193 (0%) hand-sewn | – | Unknown cause = 1 | AF = 5/50 (10%) C-port 27/193 (14%) hand-sewn Cardiac tamponade = 0 (0%) C-port 0 (0%) hand-sewn Blood products = 23/50 (46%) C-port 74/193 (38.3%) hand-sewn Reoperative bleeding = 2/50 (4%) C-port 6/193 (3.1%) hand-sewn Pneumonia = 2/50 (4%) C-port 3/193 (1.6%) hand-sewn Renal failure = 0 (0%) C-port 6/193 (3.1%) hand-sewn GI complications = 0 (0%) C-Port 4/193 (2.1%) hand-sewn Septicaemia = 0 (0%) C-port 0 (0%) hand-sewn Sternal infection = 0 (0%) C-port 0 (0%) hand-sewn Prolonged ventilation = 1/50 (2%) C-port 10/193 (5.2%) hand-sewn |
| Boening | CAC | 37 | 0/37 (0%) | 0/37 (0%) | – | – | – |
CAC: coronary anastomosis coupler; CVA: cerebrovascular accident; DAD: distal anastomotic device; MVP: magnetic vascular positioner; VCS: vessel closure system; CABG: coronary artery bypass graft; MI: myocardial Infarction; AF: atrial fibrillation; ARDS: acute respiratory distress syndrome; CO: cardiac output; GI: gastrointestinal; IABP: intra-aortic balloon pump; ITU: intensive therapy unit; NS: non-significant; TIA: transient ischaemic attack; VF: ventricular fibrillation; NS: non-significant.
| Study . | Device . | n . | Mortality (30-day) . | Postoperative MI . | Postoperative CVA . | Postoperative haemorrhage . | Causes of death . | Other morbidity . |
|---|---|---|---|---|---|---|---|---|
| Klima | MVP | 32 | 1/32 (3.1%) | 1/32 (3.1%) (non-MVP graft stenosis) | 0 (0%) | 3/32 (9.3%) (2 non-specific, 1 from hand-sewn anastamosis) | Low CO syndrome | AF = 2/31 (6.5%) Re-exploration for bleeding = 3 (9.3%) ARDS = 1/32 (3.1%) Pneumonia = 1/31 (3.2%) TIA = 1/32 (3.1%) Leg wound infection = 1/31 (3.2%) |
| Klima | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | – | Wound infection = 1/10 (10%) ITU stay (days) = 1.4 ± 0.4 Hospital stay (days) = 6.4 ± 1.2 |
| Casselman | MVP | 2 | 0/2 (0%) | – | – | – | – | – |
| Vicol | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 1/11 (9.1%) (non-specific) | – | Ventilation (h) = 16.5 ± 12 ITU stay (days) = 2.1 ± 0.7 |
| Athanasiou | MVP | 12 | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | – | VF = 1/12 (8.3%) Re-exploration = 1/12 (8.3%) Blood Loss = 914 ± 234 ml Visual defect = 1/12 (8.3%) Hospital stay (days) = 5.8 ± 1.2 (NS difference to routine CABG patients) |
| Klima | MVP | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | – | – |
| Martens | Heartflo | 60 | 1/60 (1.7%) | 0/60 (0%) | 1/60 (1.7%) | 1/60 (1.7%) Non-device-related from group 1 | Non-cardiac death = 1/60 (1.7%) | – |
| Tozzi | Heartflo | 11 | 0/11 (0%) | 0/11 (0%) | – | 0/11 (0%) | – | – |
| Wiklund | St Jude | 60 | 0/30 (0%) St Jude 1/30 (3.3%) hand-sewn | – | 0 (0%) St Jude 1/30 (3.3%) hand-sewn | 1/28 (3.6%) St Jude non-device-related bleed 0 (0%) hand-sewn | Arrhythmia in hand-sewn group = 1/30 (3.3%) | – |
| Carrel | St Jude | 32 | 1/32 (3.1%) | 1/32 (3.1%) | 1/32 (3.1%) | 0/32 (0%) | Neurological injury = 1/32 (3.1%) | Localized coronary dissection = 1/32 (3.1%) |
| Eckstein | St Jude | 19 | 0/19 (0%) | 0/19 (0%) | 0/19 (0%) | – | – | – |
| Eckstein | St Jude | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0 /1 (0%) | – | – |
| Morishige | U-Clip | 118 | 1/118 (0.8%) | 0/118 (0%) | 1/118 (0.8%) | – | – | IABP = 6 (5.1%) |
| Caskey | U-Clip | 18 | 0/18 (0%) | 1/18 (5.5%) unrelated to device | 0/18 (0%) | 0 /18 (0%) | – | Arrhythmias (unrelated to device) = 7 (38.9%) Pleural effusion = 1/18 (5.5%) TIA (unrelated to device) = 1/18 (5.5%) ITU stay (days) = 1.9 ± 0.05 Hospital stay (days) = 5 |
| Mayuga | U-clip | 30 | – | – | – | – | – | – |
| Wolf | U-clip | 59 | 2/82 (2.4%) | 1/82 (1.2%) | 0/82 (0%) | 1/82 (1.2%) non-device-related | Duodenal perforation = 1/82 (1.2%) Respiratory failure = 1/82 (1.2%) | Arrhythmia = 2/82 (2.4%) Pleural effusion = 1/82 (1.2%) TIA = 1/82 (1.2%) |
| Shemin | U-Clip | 197 | 1/59 (1.2%) U-clip 1/138 (0.7%) hand-sewn | 0/59 (0%) U-clip 0/138 (0%) hand-sewn | 0/59 (0%) U-Clip 0/138 (0%) hand-sewn | – | U-clip: respiratory failure (non-device-related) (1) hand-sewn: Multi-organ failure (1), Sepsis (1) | AF = 17% U-Clip group versus 22% hand-sewn group ( P = 0.38) Reoperation for bleeding = 2% U-Clip group versus 1.4% hand-sewn group ( P = 0.89) Blood transfusion (u) = 1.3 ± 1.5 U-Clip group versus 1.2 ± 1.7 hand-sewn group ( P = 0.82) Renal failure = 2% U-clip group versus 1% hand-sewn group ( P = 0.79) Sternal infection = 0% U-clip group versus 3% hand-sewn group ( P = 0.31) Ventilation time (h) = 5.0 ± 1.6 U-Clip group versus 5.3 ± 1.4 hand-sewn group ( P = 0.73) Length of stay (days) = 5.5 ± 1.7 U-clip group versus 5.9 ± 2.1 hand-sewn group ( P = 0.47) |
| Ono | U-clip | 13 | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | – | AF = 2/13 (15.4%) Inotropic support = 2/13 (15.4%) Blood transfusion (u) = 4/13 (30.8%) ITU stay (days) = 0.86 ± 0.16 Hospital stay (days) = 3.9 |
| Nishida | U-clip | 1 | 0/1 (0%) | – | – | – | – | Hospital stay (days) = 5 |
| Nataf | VCS | 10 | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | – | – |
| Lisi | VCS | 7 | 0/7 (0%) | 0/7 (0%) | 0/7 (0%) | 1 /7 (14.3%) Non-device-related | – | Reoperation for bleeding = 1/7 (14.3%) |
| Kim | DAD | 14 | 0/14 (0%) | – | – | – | – | – |
| Matschke | C-port | 130 | 3/130 (2.3%) | 0/130 (0%) | – | – | Right ventricular failure = 1 Myocardial infarction = 1 Adult respiratory distress syndrome = 1 | Reoperation for bleeding = 0 (0%) |
| Verberkmoes | C-Port | 71 | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 2/35 (6%) C-port 2/36 (6%) hand-sewn | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 1/35 (3%) C-port 1/36 (3%) hand-sewn | – | AF = 7 (20%) versus 6 (17%) P = 0.76 Reoperation for bleeding = 1/35 (3%) C-port versus 1/36 (3%) hand-sewn Prolonged ionotropics or IABP 2 (6%) C-port versus 2 (6%) hand-sewn P = 1 Pulmonary complications = 4 (11%) C-port versus 3 (8%) hand-sewn P = 0.71 Prolonged ventilation 1 (3%) C-port versus 1 (3%) hand-sewn P = 1 Renal complications = 2 (6%) C-port versus 0 (0%) hand-sewn P = 0.24 Deep wound infection = 1 (3%) C-port versus 0 (0%) hand-sewn P = 0.49 |
| Balkhy | C-Port | 24 | 0/24 (0%) | 0/24 (0%) | 1/25 (4%) | 1/25 (4%) | – | Reoperation for bleeding = 1/25 (4%) Renal failure = 3/25 (12%) Postoperative stay = 4.2 days |
| Balkhy | C-port | 120 | 1/120 (0.8%) | 1/120 (0.8%) | 1/120 (0.8%) | 2/120 (1.6%) | – | Pericardial effusion = 1/120 (0.8%) Brachial artery embolization = 1/120 (0.8%) Pleural effusion requiring intervention = 2/120 (1.6%) Phrenic nerve palsy = 1/120 (0.8%) Wound infection = 0 (0%) Prolonged hospitalization = 2/120 (1.6%) Hospital stay (days) = 3.3 ± 2.4 |
| Cai | C-port | 50 | 1/50 (2%) C-port 3/193 (1.6%) hand-sewn | 0/50 (0%) C-port 1/193 (0.5%) hand-sewn | 0/50 (0%) C-port 0/193 (0%) hand-sewn | – | Unknown cause = 1 | AF = 5/50 (10%) C-port 27/193 (14%) hand-sewn Cardiac tamponade = 0 (0%) C-port 0 (0%) hand-sewn Blood products = 23/50 (46%) C-port 74/193 (38.3%) hand-sewn Reoperative bleeding = 2/50 (4%) C-port 6/193 (3.1%) hand-sewn Pneumonia = 2/50 (4%) C-port 3/193 (1.6%) hand-sewn Renal failure = 0 (0%) C-port 6/193 (3.1%) hand-sewn GI complications = 0 (0%) C-Port 4/193 (2.1%) hand-sewn Septicaemia = 0 (0%) C-port 0 (0%) hand-sewn Sternal infection = 0 (0%) C-port 0 (0%) hand-sewn Prolonged ventilation = 1/50 (2%) C-port 10/193 (5.2%) hand-sewn |
| Boening | CAC | 37 | 0/37 (0%) | 0/37 (0%) | – | – | – |
| Study . | Device . | n . | Mortality (30-day) . | Postoperative MI . | Postoperative CVA . | Postoperative haemorrhage . | Causes of death . | Other morbidity . |
|---|---|---|---|---|---|---|---|---|
| Klima | MVP | 32 | 1/32 (3.1%) | 1/32 (3.1%) (non-MVP graft stenosis) | 0 (0%) | 3/32 (9.3%) (2 non-specific, 1 from hand-sewn anastamosis) | Low CO syndrome | AF = 2/31 (6.5%) Re-exploration for bleeding = 3 (9.3%) ARDS = 1/32 (3.1%) Pneumonia = 1/31 (3.2%) TIA = 1/32 (3.1%) Leg wound infection = 1/31 (3.2%) |
| Klima | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | – | Wound infection = 1/10 (10%) ITU stay (days) = 1.4 ± 0.4 Hospital stay (days) = 6.4 ± 1.2 |
| Casselman | MVP | 2 | 0/2 (0%) | – | – | – | – | – |
| Vicol | MVP | 11 | 0/11 (0%) | 0/11 (0%) | 0/11 (0%) | 1/11 (9.1%) (non-specific) | – | Ventilation (h) = 16.5 ± 12 ITU stay (days) = 2.1 ± 0.7 |
| Athanasiou | MVP | 12 | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | 0/12 (0%) | – | VF = 1/12 (8.3%) Re-exploration = 1/12 (8.3%) Blood Loss = 914 ± 234 ml Visual defect = 1/12 (8.3%) Hospital stay (days) = 5.8 ± 1.2 (NS difference to routine CABG patients) |
| Klima | MVP | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | – | – |
| Martens | Heartflo | 60 | 1/60 (1.7%) | 0/60 (0%) | 1/60 (1.7%) | 1/60 (1.7%) Non-device-related from group 1 | Non-cardiac death = 1/60 (1.7%) | – |
| Tozzi | Heartflo | 11 | 0/11 (0%) | 0/11 (0%) | – | 0/11 (0%) | – | – |
| Wiklund | St Jude | 60 | 0/30 (0%) St Jude 1/30 (3.3%) hand-sewn | – | 0 (0%) St Jude 1/30 (3.3%) hand-sewn | 1/28 (3.6%) St Jude non-device-related bleed 0 (0%) hand-sewn | Arrhythmia in hand-sewn group = 1/30 (3.3%) | – |
| Carrel | St Jude | 32 | 1/32 (3.1%) | 1/32 (3.1%) | 1/32 (3.1%) | 0/32 (0%) | Neurological injury = 1/32 (3.1%) | Localized coronary dissection = 1/32 (3.1%) |
| Eckstein | St Jude | 19 | 0/19 (0%) | 0/19 (0%) | 0/19 (0%) | – | – | – |
| Eckstein | St Jude | 1 | 0/1 (0%) | 0/1 (0%) | 0/1 (0%) | 0 /1 (0%) | – | – |
| Morishige | U-Clip | 118 | 1/118 (0.8%) | 0/118 (0%) | 1/118 (0.8%) | – | – | IABP = 6 (5.1%) |
| Caskey | U-Clip | 18 | 0/18 (0%) | 1/18 (5.5%) unrelated to device | 0/18 (0%) | 0 /18 (0%) | – | Arrhythmias (unrelated to device) = 7 (38.9%) Pleural effusion = 1/18 (5.5%) TIA (unrelated to device) = 1/18 (5.5%) ITU stay (days) = 1.9 ± 0.05 Hospital stay (days) = 5 |
| Mayuga | U-clip | 30 | – | – | – | – | – | – |
| Wolf | U-clip | 59 | 2/82 (2.4%) | 1/82 (1.2%) | 0/82 (0%) | 1/82 (1.2%) non-device-related | Duodenal perforation = 1/82 (1.2%) Respiratory failure = 1/82 (1.2%) | Arrhythmia = 2/82 (2.4%) Pleural effusion = 1/82 (1.2%) TIA = 1/82 (1.2%) |
| Shemin | U-Clip | 197 | 1/59 (1.2%) U-clip 1/138 (0.7%) hand-sewn | 0/59 (0%) U-clip 0/138 (0%) hand-sewn | 0/59 (0%) U-Clip 0/138 (0%) hand-sewn | – | U-clip: respiratory failure (non-device-related) (1) hand-sewn: Multi-organ failure (1), Sepsis (1) | AF = 17% U-Clip group versus 22% hand-sewn group ( P = 0.38) Reoperation for bleeding = 2% U-Clip group versus 1.4% hand-sewn group ( P = 0.89) Blood transfusion (u) = 1.3 ± 1.5 U-Clip group versus 1.2 ± 1.7 hand-sewn group ( P = 0.82) Renal failure = 2% U-clip group versus 1% hand-sewn group ( P = 0.79) Sternal infection = 0% U-clip group versus 3% hand-sewn group ( P = 0.31) Ventilation time (h) = 5.0 ± 1.6 U-Clip group versus 5.3 ± 1.4 hand-sewn group ( P = 0.73) Length of stay (days) = 5.5 ± 1.7 U-clip group versus 5.9 ± 2.1 hand-sewn group ( P = 0.47) |
| Ono | U-clip | 13 | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | 0/13 (0%) | – | AF = 2/13 (15.4%) Inotropic support = 2/13 (15.4%) Blood transfusion (u) = 4/13 (30.8%) ITU stay (days) = 0.86 ± 0.16 Hospital stay (days) = 3.9 |
| Nishida | U-clip | 1 | 0/1 (0%) | – | – | – | – | Hospital stay (days) = 5 |
| Nataf | VCS | 10 | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | 0/10 (0%) | – | – |
| Lisi | VCS | 7 | 0/7 (0%) | 0/7 (0%) | 0/7 (0%) | 1 /7 (14.3%) Non-device-related | – | Reoperation for bleeding = 1/7 (14.3%) |
| Kim | DAD | 14 | 0/14 (0%) | – | – | – | – | – |
| Matschke | C-port | 130 | 3/130 (2.3%) | 0/130 (0%) | – | – | Right ventricular failure = 1 Myocardial infarction = 1 Adult respiratory distress syndrome = 1 | Reoperation for bleeding = 0 (0%) |
| Verberkmoes | C-Port | 71 | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 2/35 (6%) C-port 2/36 (6%) hand-sewn | 0/35 (0%) C-port 0/36 (0%) hand-sewn | 1/35 (3%) C-port 1/36 (3%) hand-sewn | – | AF = 7 (20%) versus 6 (17%) P = 0.76 Reoperation for bleeding = 1/35 (3%) C-port versus 1/36 (3%) hand-sewn Prolonged ionotropics or IABP 2 (6%) C-port versus 2 (6%) hand-sewn P = 1 Pulmonary complications = 4 (11%) C-port versus 3 (8%) hand-sewn P = 0.71 Prolonged ventilation 1 (3%) C-port versus 1 (3%) hand-sewn P = 1 Renal complications = 2 (6%) C-port versus 0 (0%) hand-sewn P = 0.24 Deep wound infection = 1 (3%) C-port versus 0 (0%) hand-sewn P = 0.49 |
| Balkhy | C-Port | 24 | 0/24 (0%) | 0/24 (0%) | 1/25 (4%) | 1/25 (4%) | – | Reoperation for bleeding = 1/25 (4%) Renal failure = 3/25 (12%) Postoperative stay = 4.2 days |
| Balkhy | C-port | 120 | 1/120 (0.8%) | 1/120 (0.8%) | 1/120 (0.8%) | 2/120 (1.6%) | – | Pericardial effusion = 1/120 (0.8%) Brachial artery embolization = 1/120 (0.8%) Pleural effusion requiring intervention = 2/120 (1.6%) Phrenic nerve palsy = 1/120 (0.8%) Wound infection = 0 (0%) Prolonged hospitalization = 2/120 (1.6%) Hospital stay (days) = 3.3 ± 2.4 |
| Cai | C-port | 50 | 1/50 (2%) C-port 3/193 (1.6%) hand-sewn | 0/50 (0%) C-port 1/193 (0.5%) hand-sewn | 0/50 (0%) C-port 0/193 (0%) hand-sewn | – | Unknown cause = 1 | AF = 5/50 (10%) C-port 27/193 (14%) hand-sewn Cardiac tamponade = 0 (0%) C-port 0 (0%) hand-sewn Blood products = 23/50 (46%) C-port 74/193 (38.3%) hand-sewn Reoperative bleeding = 2/50 (4%) C-port 6/193 (3.1%) hand-sewn Pneumonia = 2/50 (4%) C-port 3/193 (1.6%) hand-sewn Renal failure = 0 (0%) C-port 6/193 (3.1%) hand-sewn GI complications = 0 (0%) C-Port 4/193 (2.1%) hand-sewn Septicaemia = 0 (0%) C-port 0 (0%) hand-sewn Sternal infection = 0 (0%) C-port 0 (0%) hand-sewn Prolonged ventilation = 1/50 (2%) C-port 10/193 (5.2%) hand-sewn |
| Boening | CAC | 37 | 0/37 (0%) | 0/37 (0%) | – | – | – |
CAC: coronary anastomosis coupler; CVA: cerebrovascular accident; DAD: distal anastomotic device; MVP: magnetic vascular positioner; VCS: vessel closure system; CABG: coronary artery bypass graft; MI: myocardial Infarction; AF: atrial fibrillation; ARDS: acute respiratory distress syndrome; CO: cardiac output; GI: gastrointestinal; IABP: intra-aortic balloon pump; ITU: intensive therapy unit; NS: non-significant; TIA: transient ischaemic attack; VF: ventricular fibrillation; NS: non-significant.
| Study . | Device . | Subject . | n . | Short-term angiographic patency (<1 month) . | Intermediate-term angiographic patency (1–3 months) . | Long-term angiographic patency (>3 months) . | Clinical outcome . |
|---|---|---|---|---|---|---|---|
| Klima | MVP | Human | 32 | 29/31 (93.5%) MVP 9/9 (100%) MVP (LITA to LAD) 66/72 (91.7%) hand-sewn ( P = NS) | – | – | MVP group: Preoperative CCS = 2.3 ± 0.8 Postoperative CCS = 0.37 ± 0.5 at 30 days ( P < 0.0001) |
| Klima | MVP | Human | 11 | 3/3 (100%) | – | 8/8 (100%) | – |
| Casselman | MVP | Human | 2 | 4/4 | – | – | – |
| Vicol | MVP | Human | 11 | 18/18 (100%) MVP 18/18 (100%) hand-sewn | – | 15/18 (83.3%) MVP 18/18 (100%) hand-sewn | – |
| Athanasiou | MVP | Human | 12 | 3/3 (100%) | – | – | Angina-free at 4 months = 12/12 (100%) |
| Klima | MVP | Human | 1 | 3/3 (100%) | – | – | Angina-free at 2.5 months |
| Martens | Heartflo | Human | 60 | 6/6 (100%) | – | – | – |
| Tozzi | Heartflo | Human | 11 | – | – | – | No clinical or instrumental evidence of ischaemia at 6 months |
| Wiklund | St Jude | Human | 60 | 28/28 (100%) St Jude 29/29 (100%) hand-sewn | – | 20/27 (74%) St Jude 27/27 (100%) hand-sewn | Angina-free at 6 months = 28/28 (100%) St Jude versus 31/31 (100%) hand-sewn |
| Carrel | St Jude | Human | 32 | 14/14 (100%) St Jude | 11/12 (91.7%) St Jude 41/43 (95.3%) hand-sewn | 7/10 (70%) St Jude 24/25 (96%) hand-sewn | No major adverse cardiac event or recurrence of angina at 3,6,12 months postoperatively. |
| Eckstein | St Jude | Human | 19 | 14/14 (100%) | 10/11 (90.9%) | – | – |
| Eckstein | St Jude | Human | 1 | 1/1 (100%) | – | – | – |
| Morishige | U-clip | Human | 118 | 96/101 (95.1%) | – | 31/36 (86%) | – |
| Caskey | U-clip | Human | 18 | – | – | 17/17 (100%) | – |
| Mayuga | U-clip | Human | 30 | – | – | – | – |
| Wolf | U-clip | Human | 82 | – | – | 63/63 (100%) | – |
| Shemin | U-clip | Human | 59 | – | – | – | CCS class I–II at follow-up = 90% |
| Ono | U-clip | Human | 13 | – | – | 12/12 (100%) | No ischaemic symptoms in any patient after a mean follow-up of 7.0 ± 1.7 months |
| Nishida | U-clip | Human | 1 | – | – | – | Free of symptoms 1 year postoperatively |
| Nataf | VCS | Human | 10 | – | 3/3 (100%) | – | – |
| Lisi | VCS | Human | 7 | 12/13 (92.3%) | – | – | – |
| Kim | DAD | Human | 14 | 13/14 (92.9%) DAD 32/34 (94.1%) hand-sewn | – | – | – |
| Matschke | C-port | Human | 130 | 106/107 (99.1%) | – | 94/98 (95.9%) | CCS class I-II = 98% (103/105) at 6 months postoperatively and 93% at 12 months postoperatively NYHA class I-II = 99% (104/105) at 6 months postoperatively and 98% at 12 months postoperatively |
| Verberkmoes | C-port | Human | 71 | – | – | 25/29 (86.2%) C-port versus 28/32 (87.5%) | – |
| Balkhy | C-port | Human | 24 | – | 10/10 (100%) | 14/15 (93%) | – |
| Balkhy | C-port | Human | 120 | – | – | 80/85 (94.1%) (LIMA to LAD = 55/56 = 98.2%) | – |
| Cai | C-port | – | 42/45 (93.3%) C-port 16/18 (88.9%) hand-sewn ( P = 0.62) | – | – | ||
| Boening | CAC | Human | 33 | – | 29/30 (96.7%) | – | No recurrent angina 2 months postoperatively |
| Study . | Device . | Subject . | n . | Short-term angiographic patency (<1 month) . | Intermediate-term angiographic patency (1–3 months) . | Long-term angiographic patency (>3 months) . | Clinical outcome . |
|---|---|---|---|---|---|---|---|
| Klima | MVP | Human | 32 | 29/31 (93.5%) MVP 9/9 (100%) MVP (LITA to LAD) 66/72 (91.7%) hand-sewn ( P = NS) | – | – | MVP group: Preoperative CCS = 2.3 ± 0.8 Postoperative CCS = 0.37 ± 0.5 at 30 days ( P < 0.0001) |
| Klima | MVP | Human | 11 | 3/3 (100%) | – | 8/8 (100%) | – |
| Casselman | MVP | Human | 2 | 4/4 | – | – | – |
| Vicol | MVP | Human | 11 | 18/18 (100%) MVP 18/18 (100%) hand-sewn | – | 15/18 (83.3%) MVP 18/18 (100%) hand-sewn | – |
| Athanasiou | MVP | Human | 12 | 3/3 (100%) | – | – | Angina-free at 4 months = 12/12 (100%) |
| Klima | MVP | Human | 1 | 3/3 (100%) | – | – | Angina-free at 2.5 months |
| Martens | Heartflo | Human | 60 | 6/6 (100%) | – | – | – |
| Tozzi | Heartflo | Human | 11 | – | – | – | No clinical or instrumental evidence of ischaemia at 6 months |
| Wiklund | St Jude | Human | 60 | 28/28 (100%) St Jude 29/29 (100%) hand-sewn | – | 20/27 (74%) St Jude 27/27 (100%) hand-sewn | Angina-free at 6 months = 28/28 (100%) St Jude versus 31/31 (100%) hand-sewn |
| Carrel | St Jude | Human | 32 | 14/14 (100%) St Jude | 11/12 (91.7%) St Jude 41/43 (95.3%) hand-sewn | 7/10 (70%) St Jude 24/25 (96%) hand-sewn | No major adverse cardiac event or recurrence of angina at 3,6,12 months postoperatively. |
| Eckstein | St Jude | Human | 19 | 14/14 (100%) | 10/11 (90.9%) | – | – |
| Eckstein | St Jude | Human | 1 | 1/1 (100%) | – | – | – |
| Morishige | U-clip | Human | 118 | 96/101 (95.1%) | – | 31/36 (86%) | – |
| Caskey | U-clip | Human | 18 | – | – | 17/17 (100%) | – |
| Mayuga | U-clip | Human | 30 | – | – | – | – |
| Wolf | U-clip | Human | 82 | – | – | 63/63 (100%) | – |
| Shemin | U-clip | Human | 59 | – | – | – | CCS class I–II at follow-up = 90% |
| Ono | U-clip | Human | 13 | – | – | 12/12 (100%) | No ischaemic symptoms in any patient after a mean follow-up of 7.0 ± 1.7 months |
| Nishida | U-clip | Human | 1 | – | – | – | Free of symptoms 1 year postoperatively |
| Nataf | VCS | Human | 10 | – | 3/3 (100%) | – | – |
| Lisi | VCS | Human | 7 | 12/13 (92.3%) | – | – | – |
| Kim | DAD | Human | 14 | 13/14 (92.9%) DAD 32/34 (94.1%) hand-sewn | – | – | – |
| Matschke | C-port | Human | 130 | 106/107 (99.1%) | – | 94/98 (95.9%) | CCS class I-II = 98% (103/105) at 6 months postoperatively and 93% at 12 months postoperatively NYHA class I-II = 99% (104/105) at 6 months postoperatively and 98% at 12 months postoperatively |
| Verberkmoes | C-port | Human | 71 | – | – | 25/29 (86.2%) C-port versus 28/32 (87.5%) | – |
| Balkhy | C-port | Human | 24 | – | 10/10 (100%) | 14/15 (93%) | – |
| Balkhy | C-port | Human | 120 | – | – | 80/85 (94.1%) (LIMA to LAD = 55/56 = 98.2%) | – |
| Cai | C-port | – | 42/45 (93.3%) C-port 16/18 (88.9%) hand-sewn ( P = 0.62) | – | – | ||
| Boening | CAC | Human | 33 | – | 29/30 (96.7%) | – | No recurrent angina 2 months postoperatively |
CAC: coronary anastomosis coupler; DAD: distal anastomotic device; MVP: magnetic vascular positioner; VCS: vessel closure system; CCS: Canadian Cardiovascular Society grading of angina; LAD: Left anterior descending coronary artery; LIMA: left internal mammary artery; NS: non-significant; NYHA: New York Heart Association (NYHA) Functional Classification.
| Study . | Device . | Subject . | n . | Short-term angiographic patency (<1 month) . | Intermediate-term angiographic patency (1–3 months) . | Long-term angiographic patency (>3 months) . | Clinical outcome . |
|---|---|---|---|---|---|---|---|
| Klima | MVP | Human | 32 | 29/31 (93.5%) MVP 9/9 (100%) MVP (LITA to LAD) 66/72 (91.7%) hand-sewn ( P = NS) | – | – | MVP group: Preoperative CCS = 2.3 ± 0.8 Postoperative CCS = 0.37 ± 0.5 at 30 days ( P < 0.0001) |
| Klima | MVP | Human | 11 | 3/3 (100%) | – | 8/8 (100%) | – |
| Casselman | MVP | Human | 2 | 4/4 | – | – | – |
| Vicol | MVP | Human | 11 | 18/18 (100%) MVP 18/18 (100%) hand-sewn | – | 15/18 (83.3%) MVP 18/18 (100%) hand-sewn | – |
| Athanasiou | MVP | Human | 12 | 3/3 (100%) | – | – | Angina-free at 4 months = 12/12 (100%) |
| Klima | MVP | Human | 1 | 3/3 (100%) | – | – | Angina-free at 2.5 months |
| Martens | Heartflo | Human | 60 | 6/6 (100%) | – | – | – |
| Tozzi | Heartflo | Human | 11 | – | – | – | No clinical or instrumental evidence of ischaemia at 6 months |
| Wiklund | St Jude | Human | 60 | 28/28 (100%) St Jude 29/29 (100%) hand-sewn | – | 20/27 (74%) St Jude 27/27 (100%) hand-sewn | Angina-free at 6 months = 28/28 (100%) St Jude versus 31/31 (100%) hand-sewn |
| Carrel | St Jude | Human | 32 | 14/14 (100%) St Jude | 11/12 (91.7%) St Jude 41/43 (95.3%) hand-sewn | 7/10 (70%) St Jude 24/25 (96%) hand-sewn | No major adverse cardiac event or recurrence of angina at 3,6,12 months postoperatively. |
| Eckstein | St Jude | Human | 19 | 14/14 (100%) | 10/11 (90.9%) | – | – |
| Eckstein | St Jude | Human | 1 | 1/1 (100%) | – | – | – |
| Morishige | U-clip | Human | 118 | 96/101 (95.1%) | – | 31/36 (86%) | – |
| Caskey | U-clip | Human | 18 | – | – | 17/17 (100%) | – |
| Mayuga | U-clip | Human | 30 | – | – | – | – |
| Wolf | U-clip | Human | 82 | – | – | 63/63 (100%) | – |
| Shemin | U-clip | Human | 59 | – | – | – | CCS class I–II at follow-up = 90% |
| Ono | U-clip | Human | 13 | – | – | 12/12 (100%) | No ischaemic symptoms in any patient after a mean follow-up of 7.0 ± 1.7 months |
| Nishida | U-clip | Human | 1 | – | – | – | Free of symptoms 1 year postoperatively |
| Nataf | VCS | Human | 10 | – | 3/3 (100%) | – | – |
| Lisi | VCS | Human | 7 | 12/13 (92.3%) | – | – | – |
| Kim | DAD | Human | 14 | 13/14 (92.9%) DAD 32/34 (94.1%) hand-sewn | – | – | – |
| Matschke | C-port | Human | 130 | 106/107 (99.1%) | – | 94/98 (95.9%) | CCS class I-II = 98% (103/105) at 6 months postoperatively and 93% at 12 months postoperatively NYHA class I-II = 99% (104/105) at 6 months postoperatively and 98% at 12 months postoperatively |
| Verberkmoes | C-port | Human | 71 | – | – | 25/29 (86.2%) C-port versus 28/32 (87.5%) | – |
| Balkhy | C-port | Human | 24 | – | 10/10 (100%) | 14/15 (93%) | – |
| Balkhy | C-port | Human | 120 | – | – | 80/85 (94.1%) (LIMA to LAD = 55/56 = 98.2%) | – |
| Cai | C-port | – | 42/45 (93.3%) C-port 16/18 (88.9%) hand-sewn ( P = 0.62) | – | – | ||
| Boening | CAC | Human | 33 | – | 29/30 (96.7%) | – | No recurrent angina 2 months postoperatively |
| Study . | Device . | Subject . | n . | Short-term angiographic patency (<1 month) . | Intermediate-term angiographic patency (1–3 months) . | Long-term angiographic patency (>3 months) . | Clinical outcome . |
|---|---|---|---|---|---|---|---|
| Klima | MVP | Human | 32 | 29/31 (93.5%) MVP 9/9 (100%) MVP (LITA to LAD) 66/72 (91.7%) hand-sewn ( P = NS) | – | – | MVP group: Preoperative CCS = 2.3 ± 0.8 Postoperative CCS = 0.37 ± 0.5 at 30 days ( P < 0.0001) |
| Klima | MVP | Human | 11 | 3/3 (100%) | – | 8/8 (100%) | – |
| Casselman | MVP | Human | 2 | 4/4 | – | – | – |
| Vicol | MVP | Human | 11 | 18/18 (100%) MVP 18/18 (100%) hand-sewn | – | 15/18 (83.3%) MVP 18/18 (100%) hand-sewn | – |
| Athanasiou | MVP | Human | 12 | 3/3 (100%) | – | – | Angina-free at 4 months = 12/12 (100%) |
| Klima | MVP | Human | 1 | 3/3 (100%) | – | – | Angina-free at 2.5 months |
| Martens | Heartflo | Human | 60 | 6/6 (100%) | – | – | – |
| Tozzi | Heartflo | Human | 11 | – | – | – | No clinical or instrumental evidence of ischaemia at 6 months |
| Wiklund | St Jude | Human | 60 | 28/28 (100%) St Jude 29/29 (100%) hand-sewn | – | 20/27 (74%) St Jude 27/27 (100%) hand-sewn | Angina-free at 6 months = 28/28 (100%) St Jude versus 31/31 (100%) hand-sewn |
| Carrel | St Jude | Human | 32 | 14/14 (100%) St Jude | 11/12 (91.7%) St Jude 41/43 (95.3%) hand-sewn | 7/10 (70%) St Jude 24/25 (96%) hand-sewn | No major adverse cardiac event or recurrence of angina at 3,6,12 months postoperatively. |
| Eckstein | St Jude | Human | 19 | 14/14 (100%) | 10/11 (90.9%) | – | – |
| Eckstein | St Jude | Human | 1 | 1/1 (100%) | – | – | – |
| Morishige | U-clip | Human | 118 | 96/101 (95.1%) | – | 31/36 (86%) | – |
| Caskey | U-clip | Human | 18 | – | – | 17/17 (100%) | – |
| Mayuga | U-clip | Human | 30 | – | – | – | – |
| Wolf | U-clip | Human | 82 | – | – | 63/63 (100%) | – |
| Shemin | U-clip | Human | 59 | – | – | – | CCS class I–II at follow-up = 90% |
| Ono | U-clip | Human | 13 | – | – | 12/12 (100%) | No ischaemic symptoms in any patient after a mean follow-up of 7.0 ± 1.7 months |
| Nishida | U-clip | Human | 1 | – | – | – | Free of symptoms 1 year postoperatively |
| Nataf | VCS | Human | 10 | – | 3/3 (100%) | – | – |
| Lisi | VCS | Human | 7 | 12/13 (92.3%) | – | – | – |
| Kim | DAD | Human | 14 | 13/14 (92.9%) DAD 32/34 (94.1%) hand-sewn | – | – | – |
| Matschke | C-port | Human | 130 | 106/107 (99.1%) | – | 94/98 (95.9%) | CCS class I-II = 98% (103/105) at 6 months postoperatively and 93% at 12 months postoperatively NYHA class I-II = 99% (104/105) at 6 months postoperatively and 98% at 12 months postoperatively |
| Verberkmoes | C-port | Human | 71 | – | – | 25/29 (86.2%) C-port versus 28/32 (87.5%) | – |
| Balkhy | C-port | Human | 24 | – | 10/10 (100%) | 14/15 (93%) | – |
| Balkhy | C-port | Human | 120 | – | – | 80/85 (94.1%) (LIMA to LAD = 55/56 = 98.2%) | – |
| Cai | C-port | – | 42/45 (93.3%) C-port 16/18 (88.9%) hand-sewn ( P = 0.62) | – | – | ||
| Boening | CAC | Human | 33 | – | 29/30 (96.7%) | – | No recurrent angina 2 months postoperatively |
CAC: coronary anastomosis coupler; DAD: distal anastomotic device; MVP: magnetic vascular positioner; VCS: vessel closure system; CCS: Canadian Cardiovascular Society grading of angina; LAD: Left anterior descending coronary artery; LIMA: left internal mammary artery; NS: non-significant; NYHA: New York Heart Association (NYHA) Functional Classification.
Postoperative outcomes
Five studies [ 8 , 17 , 21 , 27 , 32 ] reported comparative results of postoperative outcomes for hand-sewn anastomosis versus DADs. A further 23 studies [ 1 , 2 , 5 , 6 , 8–10 , 13 , 14 , 16–26 , 28–34 ] reported results for anastomotic devices without a comparative group. A summary of the postoperative results is reported in Table 4 .
| . | Mortality . | MI . | CVA . | Postoperative haemorrhage . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Number of studies . | Observed mortality . | Cardiac-related mortality . | Number of studies . | Observed MI . | Number of studies . | Observed CVA . | Number of studies . | Observed postoperative haemorrhage . | |
| MVP | 6 | 1.4% (1/69) | 1.4% (1/69) | 5 | 1.5% (1/67) | 5 | 0% (0/67) | 5 | 6% (4/67) |
| Heartflo | 2 | 1.4% (1/71) | 0% (0/71) | 2 | 0% (0/71) | 1 | 0% (1/60) | 2 | 1.4% (1/71) |
| St Jude | 4 | 1.2% (1/82) | 0% (0/82) | 3 | 1.9% (1/52) | 4 | 1.2% (1/82) | 3 | 1.6% (1/61) |
| U-clip | 7 | 1.4% (4/291) | 0% (0/291) | 5 | 0.7% (2/290) | 5 | 0.3% (1/290) | 3 | 0.8% (1/123) |
| VCS | 2 | 0% (0/17) | 0% (0/17) | 2 | 0% (0/17) | 2 | 0% (0/17) | 2 | 5.9% (1/17) |
| DAD | 1 | 0% (0/14) | 0% (0/14) | – | – | – | – | – | – |
| C-port | 5 | 1.4% (5/359) | 0.6% (2/359) | 5 | 0.8% (3/359) | 4 | 0.9% (2/230) | 2 | 2.2% (4/180) |
| CAC | 1 | 0% (0/37) | 0% (0/37) | 1 | 0% (0/37) | – | – | – | – |
| Overall device proportions | 28 | 1.3% (12/940) | 0.3% (3/940) | 23 | 0.8% (7/893) | 21 | 0.7% (5/746) | 17 | 2.3% (12/519) |
| Overall hand-sewn proportions | 5 | 1.3% (5/397) | 0.3% (1/397) | 2 | 0.8% (3/367) | 4 | 0.3% (1/397) | 2 | 1.5% (1/66) |
| . | Mortality . | MI . | CVA . | Postoperative haemorrhage . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Number of studies . | Observed mortality . | Cardiac-related mortality . | Number of studies . | Observed MI . | Number of studies . | Observed CVA . | Number of studies . | Observed postoperative haemorrhage . | |
| MVP | 6 | 1.4% (1/69) | 1.4% (1/69) | 5 | 1.5% (1/67) | 5 | 0% (0/67) | 5 | 6% (4/67) |
| Heartflo | 2 | 1.4% (1/71) | 0% (0/71) | 2 | 0% (0/71) | 1 | 0% (1/60) | 2 | 1.4% (1/71) |
| St Jude | 4 | 1.2% (1/82) | 0% (0/82) | 3 | 1.9% (1/52) | 4 | 1.2% (1/82) | 3 | 1.6% (1/61) |
| U-clip | 7 | 1.4% (4/291) | 0% (0/291) | 5 | 0.7% (2/290) | 5 | 0.3% (1/290) | 3 | 0.8% (1/123) |
| VCS | 2 | 0% (0/17) | 0% (0/17) | 2 | 0% (0/17) | 2 | 0% (0/17) | 2 | 5.9% (1/17) |
| DAD | 1 | 0% (0/14) | 0% (0/14) | – | – | – | – | – | – |
| C-port | 5 | 1.4% (5/359) | 0.6% (2/359) | 5 | 0.8% (3/359) | 4 | 0.9% (2/230) | 2 | 2.2% (4/180) |
| CAC | 1 | 0% (0/37) | 0% (0/37) | 1 | 0% (0/37) | – | – | – | – |
| Overall device proportions | 28 | 1.3% (12/940) | 0.3% (3/940) | 23 | 0.8% (7/893) | 21 | 0.7% (5/746) | 17 | 2.3% (12/519) |
| Overall hand-sewn proportions | 5 | 1.3% (5/397) | 0.3% (1/397) | 2 | 0.8% (3/367) | 4 | 0.3% (1/397) | 2 | 1.5% (1/66) |
CAC: coronary anastomosis coupler; CVA: cerebrovascular accident; DAD: distal anastomotic device; MVP: magnetic vascular positioner; VCS: vessel closure system; MI: myocardial Infarction.
| . | Mortality . | MI . | CVA . | Postoperative haemorrhage . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Number of studies . | Observed mortality . | Cardiac-related mortality . | Number of studies . | Observed MI . | Number of studies . | Observed CVA . | Number of studies . | Observed postoperative haemorrhage . | |
| MVP | 6 | 1.4% (1/69) | 1.4% (1/69) | 5 | 1.5% (1/67) | 5 | 0% (0/67) | 5 | 6% (4/67) |
| Heartflo | 2 | 1.4% (1/71) | 0% (0/71) | 2 | 0% (0/71) | 1 | 0% (1/60) | 2 | 1.4% (1/71) |
| St Jude | 4 | 1.2% (1/82) | 0% (0/82) | 3 | 1.9% (1/52) | 4 | 1.2% (1/82) | 3 | 1.6% (1/61) |
| U-clip | 7 | 1.4% (4/291) | 0% (0/291) | 5 | 0.7% (2/290) | 5 | 0.3% (1/290) | 3 | 0.8% (1/123) |
| VCS | 2 | 0% (0/17) | 0% (0/17) | 2 | 0% (0/17) | 2 | 0% (0/17) | 2 | 5.9% (1/17) |
| DAD | 1 | 0% (0/14) | 0% (0/14) | – | – | – | – | – | – |
| C-port | 5 | 1.4% (5/359) | 0.6% (2/359) | 5 | 0.8% (3/359) | 4 | 0.9% (2/230) | 2 | 2.2% (4/180) |
| CAC | 1 | 0% (0/37) | 0% (0/37) | 1 | 0% (0/37) | – | – | – | – |
| Overall device proportions | 28 | 1.3% (12/940) | 0.3% (3/940) | 23 | 0.8% (7/893) | 21 | 0.7% (5/746) | 17 | 2.3% (12/519) |
| Overall hand-sewn proportions | 5 | 1.3% (5/397) | 0.3% (1/397) | 2 | 0.8% (3/367) | 4 | 0.3% (1/397) | 2 | 1.5% (1/66) |
| . | Mortality . | MI . | CVA . | Postoperative haemorrhage . | |||||
|---|---|---|---|---|---|---|---|---|---|
| Number of studies . | Observed mortality . | Cardiac-related mortality . | Number of studies . | Observed MI . | Number of studies . | Observed CVA . | Number of studies . | Observed postoperative haemorrhage . | |
| MVP | 6 | 1.4% (1/69) | 1.4% (1/69) | 5 | 1.5% (1/67) | 5 | 0% (0/67) | 5 | 6% (4/67) |
| Heartflo | 2 | 1.4% (1/71) | 0% (0/71) | 2 | 0% (0/71) | 1 | 0% (1/60) | 2 | 1.4% (1/71) |
| St Jude | 4 | 1.2% (1/82) | 0% (0/82) | 3 | 1.9% (1/52) | 4 | 1.2% (1/82) | 3 | 1.6% (1/61) |
| U-clip | 7 | 1.4% (4/291) | 0% (0/291) | 5 | 0.7% (2/290) | 5 | 0.3% (1/290) | 3 | 0.8% (1/123) |
| VCS | 2 | 0% (0/17) | 0% (0/17) | 2 | 0% (0/17) | 2 | 0% (0/17) | 2 | 5.9% (1/17) |
| DAD | 1 | 0% (0/14) | 0% (0/14) | – | – | – | – | – | – |
| C-port | 5 | 1.4% (5/359) | 0.6% (2/359) | 5 | 0.8% (3/359) | 4 | 0.9% (2/230) | 2 | 2.2% (4/180) |
| CAC | 1 | 0% (0/37) | 0% (0/37) | 1 | 0% (0/37) | – | – | – | – |
| Overall device proportions | 28 | 1.3% (12/940) | 0.3% (3/940) | 23 | 0.8% (7/893) | 21 | 0.7% (5/746) | 17 | 2.3% (12/519) |
| Overall hand-sewn proportions | 5 | 1.3% (5/397) | 0.3% (1/397) | 2 | 0.8% (3/367) | 4 | 0.3% (1/397) | 2 | 1.5% (1/66) |
CAC: coronary anastomosis coupler; CVA: cerebrovascular accident; DAD: distal anastomotic device; MVP: magnetic vascular positioner; VCS: vessel closure system; MI: myocardial Infarction.
Mortality
The overall 30-day and cardiac-specific mortality was equal between DADs (overall 1.3%; 12/940; cardiac-specific 0.3%; 3/940) and hand-sewn cases (overall 1.3%; 5/397; cardiac-specific 0.3%; 1/397) (Fisher's exact test (two-tailed) P = 0.57 overall, P = 1.000 cardiac-specific mortality).
The lowest cardiac-specific mortality (0/291) was observed with a U-clip device; however, the St Jude (0/82), Heartflo (0/71), CAC (0/37), VCS clip applier (0/17) and DAD (0/14) devices also demonstrated low mortality in their limited sample sizes. One cardiac-specific death was observed with the MVP device (1.4%; 1/69) [ 1 ]; however, no graft occlusion was noted during re-exploration and the low cardiac output state was attributed to ischaemia from a non-grafted vessel [ 1 ]. Similarly, the 2 cases of cardiac-specific death (2/359) reported in studies using the C-port device were also found to be unrelated to device use [ 16 ]. The first of these was secondary to myocardial infarction in the territory grafted using a hand-sewn technique and the second was due to right ventricular dysfunction with no evidence of anastomotic occlusion [ 16 ].
Morbidity: myocardial infarction, cerebrovascular accident and postoperative bleeding
Overall, myocardial infarction was demonstrated to be equivalent between DADs (0.8%; 7/893) and hand-sewn cases (0.8%; 3/367) [Fisher's exact test (two-tailed) P = 1.000]. Zero myocardial infarction was observed with the Heartflo (0/71), CAC (0/37) and VCS (0/17) devices. The St Jude (1.9%; 1/52) and MVP (1.5%; 1/67) devices were associated with the highest proportion of postoperative myocardial infarction (MI), whereas lower proportions were observed in the larger series from the C-port (0.8%; 3/359) and U-clip (0.7%; 2/290) devices. Of these events, only one MI was attributed to technical device failure (in a case utilizing the C-port), which necessitated conversion to the hand-sewn approach.
The overall proportion of stroke was slightly higher for DADs than for hand-sewn cases [0.7% (5/746) vs 0.3% (1/397)], although this was not statistically significant [Fisher's exact test (two-tailed) P = 0.67]. Zero stroke events were observed in cases utilizing the MVP (0/67), Heartflo (1/60) and VCS (0/17) devices. There was one case of neurological injury with the St Jude device (1/82), attributed to grade 3 ascending aortic atherosclerosis rather than being device related [ 22 ]. Postoperative stroke was also observed in one patient undergoing concomitant aortic valve replacement [ 19 ] and another who underwent carotid endarterectomy 2 days prior to CABG [ 20 ]. One stroke was observed with the use of the U-clip device although the aetiology of this is not recorded [ 28 ].
The overall proportion of patients experiencing postoperative haemorrhage (as defined by the study's authors) was higher in the anastomotic device group (2.3%; 12/519) in comparison with hand-sewn anastomosis (1.5%; 1/66). Again, this did not reach statistical significance [Fisher's exact test (two-tailed) P = 1.000]. The lowest proportion of postoperative haemorrhage was found with the U-clip device (0.8%; 1/123). In contrast, the highest proportion of postoperative haemorrhage was observed with the VCS device (5.9%; 1/17), followed by the C-port (2.2%; 4/180), St Jude (1.6%; 1/61) and Heartflo (1.4%; 1/71) devices. With the MVP device, three postoperative bleeding cases were reported as non-specific and one from a hand-sewn radial artery branch [ 1 , 10 ] .
Anastomotic patency
A summary of graft patency outcomes is presented in Table 5 . In 21 studies, patency was assessed using angiography [ 1 , 2 , 5 , 6 , 9 , 10 , 13 , 14 , 16–18 , 22–26 , 28 , 30 , 32–34 ]. In the remaining seven studies, three used computed tomography [ 19–21 ] and four studies had no patency data [ 8 , 27 , 29 , 31 ].
| . | <1 month . | 1–3 months . | >3 months . | |||
|---|---|---|---|---|---|---|
| Number of studies . | Short-term angiographic patency . | Number of studies . | Intermediate-term angiographic patency . | Number of studies . | Long-term angiographic patency . | |
| MVP | 6 | 96.8% (60/62) | – | – | 2 | 88.5% (23/26) |
| Heartflo | 1 | 100% (6/6)) | – | – | – | – |
| St Jude | 4 | 100% (57/57) | 2 | 91.3% (21/23) | 2 | 73% (27/37) |
| U-Clip | 1 | 95.1% (96/101) | – | – | 4 | 96.1% (123/128) |
| VCS | 1 | 92.3% (12/13) | 1 | 100% (3/3) | – | – |
| DAD | 1 | 92.9% (13/14) | – | – | – | – |
| C-Port | 1 | 99.1% (106/107) | 2 | 94.5% (52/55) | 4 | 93.8% (213/227) |
| CAC | – | – | 1 | 96.7% (29/30) | – | – |
| Overall device patency | 15 | 97.2% (350/360) | 6 | 94.6% (105/111) | 12 | 92.3% (386/418) |
| Overall hand-sewn patency | 3 | 94.8% (145/153) | 2 | 93.4% (57/61) | 3 | 95.1% (97/102) |
| . | <1 month . | 1–3 months . | >3 months . | |||
|---|---|---|---|---|---|---|
| Number of studies . | Short-term angiographic patency . | Number of studies . | Intermediate-term angiographic patency . | Number of studies . | Long-term angiographic patency . | |
| MVP | 6 | 96.8% (60/62) | – | – | 2 | 88.5% (23/26) |
| Heartflo | 1 | 100% (6/6)) | – | – | – | – |
| St Jude | 4 | 100% (57/57) | 2 | 91.3% (21/23) | 2 | 73% (27/37) |
| U-Clip | 1 | 95.1% (96/101) | – | – | 4 | 96.1% (123/128) |
| VCS | 1 | 92.3% (12/13) | 1 | 100% (3/3) | – | – |
| DAD | 1 | 92.9% (13/14) | – | – | – | – |
| C-Port | 1 | 99.1% (106/107) | 2 | 94.5% (52/55) | 4 | 93.8% (213/227) |
| CAC | – | – | 1 | 96.7% (29/30) | – | – |
| Overall device patency | 15 | 97.2% (350/360) | 6 | 94.6% (105/111) | 12 | 92.3% (386/418) |
| Overall hand-sewn patency | 3 | 94.8% (145/153) | 2 | 93.4% (57/61) | 3 | 95.1% (97/102) |
CAC: coronary anastomosis coupler; VCS: vessel closure system; DAD: distal anastomotic device; MVP: magnetic vascular positioner.
| . | <1 month . | 1–3 months . | >3 months . | |||
|---|---|---|---|---|---|---|
| Number of studies . | Short-term angiographic patency . | Number of studies . | Intermediate-term angiographic patency . | Number of studies . | Long-term angiographic patency . | |
| MVP | 6 | 96.8% (60/62) | – | – | 2 | 88.5% (23/26) |
| Heartflo | 1 | 100% (6/6)) | – | – | – | – |
| St Jude | 4 | 100% (57/57) | 2 | 91.3% (21/23) | 2 | 73% (27/37) |
| U-Clip | 1 | 95.1% (96/101) | – | – | 4 | 96.1% (123/128) |
| VCS | 1 | 92.3% (12/13) | 1 | 100% (3/3) | – | – |
| DAD | 1 | 92.9% (13/14) | – | – | – | – |
| C-Port | 1 | 99.1% (106/107) | 2 | 94.5% (52/55) | 4 | 93.8% (213/227) |
| CAC | – | – | 1 | 96.7% (29/30) | – | – |
| Overall device patency | 15 | 97.2% (350/360) | 6 | 94.6% (105/111) | 12 | 92.3% (386/418) |
| Overall hand-sewn patency | 3 | 94.8% (145/153) | 2 | 93.4% (57/61) | 3 | 95.1% (97/102) |
| . | <1 month . | 1–3 months . | >3 months . | |||
|---|---|---|---|---|---|---|
| Number of studies . | Short-term angiographic patency . | Number of studies . | Intermediate-term angiographic patency . | Number of studies . | Long-term angiographic patency . | |
| MVP | 6 | 96.8% (60/62) | – | – | 2 | 88.5% (23/26) |
| Heartflo | 1 | 100% (6/6)) | – | – | – | – |
| St Jude | 4 | 100% (57/57) | 2 | 91.3% (21/23) | 2 | 73% (27/37) |
| U-Clip | 1 | 95.1% (96/101) | – | – | 4 | 96.1% (123/128) |
| VCS | 1 | 92.3% (12/13) | 1 | 100% (3/3) | – | – |
| DAD | 1 | 92.9% (13/14) | – | – | – | – |
| C-Port | 1 | 99.1% (106/107) | 2 | 94.5% (52/55) | 4 | 93.8% (213/227) |
| CAC | – | – | 1 | 96.7% (29/30) | – | – |
| Overall device patency | 15 | 97.2% (350/360) | 6 | 94.6% (105/111) | 12 | 92.3% (386/418) |
| Overall hand-sewn patency | 3 | 94.8% (145/153) | 2 | 93.4% (57/61) | 3 | 95.1% (97/102) |
CAC: coronary anastomosis coupler; VCS: vessel closure system; DAD: distal anastomotic device; MVP: magnetic vascular positioner.
Overall early patency (<1 month) was reported for 360 of 940 device-related anastomoses and 153 of 397 hand-sewn anastomoses. The overall pooled early (<1 month) patency for all DADs was 97.2% (350/360) compared with 94.8% (145/153) for hand-sewn cases (Pearson's χ2 , P = 0.168). The St Jude (57/57) and Heartflo (6/6) anastomotic devices exhibited 100% patency at 1 month.
Overall mid-term patency (1–3 months) was reported for 111 of 940 device-related anastomoses and 61 of 397 hand-sewn anastomoses. The mid-term patency was 94.6% (105/111) for DADs compared with 93.4% (57/61) in the hand-sewn cases (Pearson's χ2P = 0.757), although notably only one-third of the original device patients had patency re-assessed at this stage.
Overall long-term (>3 months) patency data were reported for 418 of 940 device-related anastomoses and 102 of 397 hand-sewn anastomoses. The long-term patency was 92.3% for DADs (386/418) compared with 95.1% (97/102) for hand-sewn anastomoses (Pearson's χ2P = 0.332). The highest long-term patency was observed for the U-clip device at 96.1% (123/128). Importantly, there was a significant reduction in patency from the early to late period with the St Jude, MVP and C-port devices, accounting for the lower overall observed late patency in comparison with hand-sewn cases.
DISCUSSION
The overall cardiac-specific mortality was equivalent between device (0.3%; 3/940) and hand-sewn (0.3%; 1/397) cases reported in this pooled series of data. U-clip, St Jude, Heartflo, CAC, VCS and DAD devices reported no cardiac-specific mortality and further analysis revealed no association between the mortality observed in cases utilizing the MVP and C-port systems and anastomotic device use.
Similarly, the pooled proportion of postoperative MI was also equivalent between anastomotic (0.8%; 7/893) and hand-sewn (0.8%; 3/367) cases, with only two of these events attributable to device use (C-port device [ 17 , 20 ]).
The overall proportion of patients experiencing cerebrovascular accidents (CVAs) was slightly higher for anastomotic devices (0.7%; 5/746) in comparison with (0.3%; 1/397) hand-sewn cases although this was not statistically significant. The highest proportion of CVAs was observed with the St Jude anastomotic device (1.2%; 1/82). However, cases of neurological injury observed with the use of the S. Jude and C-port devices were both unrelated to use of an anastomotic device, instead being associated with atherosclerosis of the aorta [ 22 ], concomitant aortic valve replacement [ 19 ] and carotid endarterectomy, respectively [ 20 ]. The lowest proportion of CVAs was reported with the U-clip device [ 28 ], demonstrating equivalence to hand-sewn cases (0.3%).
Although there appears to be equivalence between the devices in terms of mortality and postoperative MI in these small series, the least overall postoperative bleeding is observed with the U-clip device, likely related to its mechanics and handling. The U-clip device (Fig. 1 ) allows the placement of interrupted sutures without the need for knot tying. Unlike other devices that force the coronary tissue to conform to the instrument, the U-clip design allows suture placement similar to that of any conventional interrupted surgical anastomosis, with good adaptability to variation in tissue architecture. As a result, its learning curve is also less than with other devices that utilize unfamiliar device-specific anastomotic techniques (Fig. 1 ) [ 8 ].
In contrast, the most postoperative bleeding was observed with the MVP device. However, two studies reporting on 4 cases of postoperative bleeding did not reveal any relation between use of the MVP device and bleeding [ 1 , 10 ]. One notable disadvantage of the MVP device is the need to create a perfectly sized arteriotomy in both the graft and the native coronary vessel, necessitating a degree of experience in the technique. If the arteriotomy is too small, there will be surplus tissue within the vessel lumen resulting in a stenosis at the anastomotic site. However, if the arteriotomy is too wide, this may leave little arterial wall between the two magnet rings (Fig. 1 ), resulting in a poor haemostatic seal and leakage between the magnets [ 1 , 38 ]. As such, it is possible that a degree of the increased bleeding documented with the MVP device is related to this technical limitation inherent in the device design.
Similarly, the VCS device was also observed to be associated with a relatively higher proportion of overall postoperative bleeding. The VCS works through the insertion of non-penetrating clips on the outside of the graft and coronary vessel to achieve an anastomosis. However, this technique produces two key disadvantages. Firstly, as the device relies on everting the wall of the coronary artery, it may not be suitable in calcified or thickened vessels. Secondly, it is pertinent that the clips are placed in close proximity (∼1 mm apart) and additional clip placement to achieve haemostasis may be technically very challenging [ 14 , 26 ].
Histological samples from animal studies have shown that complete endothelialization of the luminal surface of a device-constructed anastomosis can occur within 6 weeks of implantation [ 2 ]. As a result, a comparison of patency observations beyond a 30-day follow-up is of paramount importance when considering the use of anastomotic devices. At mid-late term follow-up (>3 months), the best overall graft patency was observed with the U-clip device. Through modelling an interrupted suture design, the nitinol U-clip is able to maintain the perianastomotic compliance seen with hand-sewn anastomoses, while also minimizing the extent of the non-intimal surface of the vessel present in the luminal side of the anastomosis [the blood-exposed non-intimal surface (BENIS) in device-constructed anastomoses area]. These features together help to reduce both intimal hyperplasia [ 28 ] and the perianastomotic inflammatory response. As a result, the nitinol U-clip may produce comparable levels of postoperative anastomotic stenosis to hand-sewn techniques, both in the short- and mid-term [ 28 , 44 ].
Good mid-term patency was also seen with the C-port device, which through a similar principle to the U-clip minimizes surgical trauma and exposure of the non-intimal surface of the vessel wall (BENIS area) [ 16 ]. In comparison, both the MVP (33 mm 2 ) [ 10 ] and St Jude (3–4 mm 2 ) [ 22 , 32 ] DADs have higher BENIS area, particularly when compared with hand-sewn anastomoses (0.91 mm 2 ) [ 22 ], which may precipitate intimal hyperplasia and subsequent anastomotic stenosis [ 18 ].
Comparatively lower mid-term patency was observed with the MVP and St Jude devices, likely occurring as a result of features inherent in the device design. For example, the MVP device requires an ideal arteriotomy on the graft and native vessels to achieve a good haemostatic seal while at the same time avoiding excessive tissue in the anastomotic orifice. If the arteriotomy is too small, protrusion of the arterial wall into the new lumen following insertion of the magnets may result in narrowing of the anastomosis, turbulent flow, thrombosis and graft failure [ 38 ]. Conversely, the St Jude device creates a redundant blind-ended sac after completion of the anastomosis, which may later form a nidus for thrombus formation and subsequent intimal hyperplasia [ 32 ].
Limitations
There are several limitations in both the study design and outcome reporting which influence the interpretation of these results. Firstly, the majority of trials were small observational studies with only four randomized controlled trials. Only nine studies reported more than 50 recruited patients. Secondly, while some comparison was made between anastomotic devices and hand-sewn cases, no direct comparison exists between different device types. Furthermore, inter-study variations in the extent of coronary artery stenosis and calcification, target vessel quality, choice of graft and target vessel, choice of access (Open vs MIDCAB vs TECAB), comorbidities, anticoagulation strategies and follow-up period are likely to influence pooled results and should be taken into consideration when interpreting outcome data. Similarly, as only five studies directly compared devices with the hand-sewn anastomosis, of which just two utilized the same device, a meta-analysis comparing these techniques is not possible and, consequently, only a non-weighted comparison of proportions has been reported.
CONCLUSIONS
The development of distal coronary anastomotic devices to facilitate CABG has met with a number of technical challenges. In addition, variations in the pathological presentation of coronary artery disease and the need to maintain consistency in anastomotic precision and quality without compromising long-term patency has led to slow progress in the development and uptake of such technologies.
The majority of presently available data exist for the C-port (359 anastomoses) and U-clip (291 anastomoses) devices. In fact, these are the only two available devices currently approved for use by the U.S. Food and Drug Administration. In this pooled series of data, the U-clip device was found to provide the best overall long-term graft patency with no cardiac-specific mortality and the least overall proportion of postoperative bleeding. Furthermore, the associated numbers of postoperative MI and CVAs were comparable with those for hand-sewn techniques. This device is also able to provide better long-term graft patency, utilizing an interrupted approach that minimizes vessel wall trauma. The combination of these factors is likely to result in better anastomotic compliance, minimal intimal hyperplasia and reduced anastomotic stenosis when compared with other devices (Fig. 1 ), which often compromise on at least one of these factors. In terms of anastomotic bleeding, the interrupted suture design of the U-clip device has again produced results comparable with hand-sewn techniques, and through removing the need for knot tying, it provides a promising tool for procedures such as TECAB. However, it is notable that this approach compromises on device automaticity as it still requires the placement of 8–12 anastomotic sutures.
In summary, while the U-clip device provides comparatively the best published results to date, these findings highlight the difficulty in developing a device that not only produces results comparable with hand-sewn techniques, but also preserves automaticity. Further phase IV clinical trials should focus on randomization to compare novel devices with hand-sewn techniques in carefully selected patient groups, specifying both the territory of the vessel grafted and the operative technique used (i.e. open, MIDCAB, TECAB). With the reporting of results, one should carefully examine both short- and long-term morbidity and mortality outcomes with interval angiographic follow-up in order to perform a quantitative assessment of long-term graft patency.
Funding
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest: none declared.
REFERENCES




