-
PDF
- Split View
-
Views
-
Cite
Cite
Frédéric Bodin, Caroline Dissaux, Jean-Paul Steib, Gilbert Massard, Complex posterior thoracic wall reconstruction using a crossover combined latissimus dorsi and serratus anterior free flap, European Journal of Cardio-Thoracic Surgery, Volume 49, Issue 3, March 2016, Pages 1008–1009, https://doi.org/10.1093/ejcts/ezv141
Close - Share Icon Share
Abstract
Radical resection of an extended malignant sarcoma of the chest wall requires full-thickness thoracic chest wall reconstruction. Reconstruction is tedious in the case of posteriorly located tumours, because the ipsilateral pedicled myocutaneous latissimus dorsi flap is involved and hence not usable for soft tissue coverage. We report an original case of a left giant dorsal chondrosarcoma originating from the 11th costovertebral joint. After extended resection and skeletal reconstruction, soft tissue coverage was achieved with an original contralateral free flap encompassing both latissimus dorsi and serratus anterior muscles. The flap pedicle was anastomosed to the ipsilateral thoracodorsal vessels.
INTRODUCTION
Chondrosarcoma is the most common primary malignant tumour of the rib cage. Appropriate treatment requires a wide surgical resection with adequate margins, leading to a full-thickness defect. In this case report, chest wall reconstruction was performed using an original crossover free flap encompassing the contralateral latissimus dorsi and serratus anterior muscles.
CASE REPORT
In February 2013, a 40-year old man was referred for resection of a giant left dorsal tumour. The patient's clinical history revealed the resection of a dorsal exostosis of the 11th rib in 1994. The tumour has recurred during the past 10 years with a recent acceleration of growth. Clinical examination showed a giant fixed subcutaneous tumour in the left middle back exceeding the median line. A CT scan showed a partially calcified mass originating from the 11th costovertebral junction, measuring 21 × 17 × 27 cm (Fig. 1 ). Incisional biopsy revealed a chondrosarcoma.
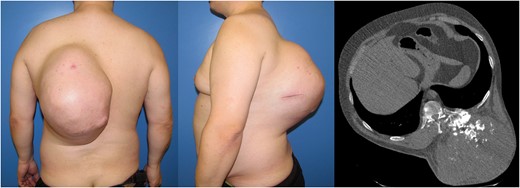
Giant chondrosarcoma located on the left posterior chest wall. A CT scan showed a partially calcified mass originating from the 11th costovertebral junction.
A complete en bloc resection was undertaken by a multidisciplinary team composed of thoracic, spine and plastic surgeons. The resection was conducted simultaneously from the outside (spine surgeon) and inside (thoracic surgeon), achieving the macroscopically complete resection of a specimen weighing 6.031 kg and measuring 30 × 24 × 20 cm. The thoracic wall defect involving three costovertebral levels (T9–T11) measured 13 × 9 cm. The vertebral reconstruction was performed with posterior spinal stabilization and an anterior titanium mesh cage. The chest wall defect was occluded by insertion of a polytetrafluoroethylene mesh. The remaining full-thickness soft tissue defect measured 30 × 30 cm. A contralateral free flap, encompassing latissimus dorsi and serratus anterior muscles, with its common thoracodorsal pedicle was harvested (Fig. 2 ). Microsurgical anastomoses were performed on the remnant ipsilateral thoracodorsal vessels. The defect was completely covered by using both muscles. However, a lumbar fasciocutaneous flap was transposed to secure the distal part of the free flap facing the osteosynthesis material (Fig. 2 ). The duration of the surgical procedure was 12 h. Eleven units of packed platelets and 14 units of packed red cells were transfused.
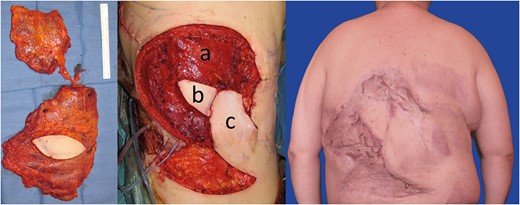
On the left side: Combined myocutaneous latissimus dorsi and serratus anterior free flap pedicled on the thoracodorsal vessels. In the middle: Soft tissue coverage with the contralateral combined latissimus dorsi and serratus anterior free flap. ( a ) Latissimus dorsi and serratus anterior muscle. ( b ) Monitoring skin paddle. ( c ) Lumbar fasciocutaneous flap transposed to secure the distal part of the free flap. On the right side: cosmetic result after split-thickness skin graft and 18 months of follow-up.
The immediate postoperative outcome was uneventful. After 2 weeks, a second operation was performed to cover the muscle with a split-thickness skin graft. Complete healing was achieved at 3 months post operation. After the 18-month follow-up, clinical and radiological examinations showed favourable outcome, with a stable chest wall and without any sign of recurrence (Fig. 2 ). Mild neurogenic pain of the left lower chest wall was controlled by paracetamol.
DISCUSSION
Chondrosarcoma of the chest wall occurs mainly in males aged between 30 and 60 years, and the most frequent location is the sternum or the anterior costochondral joint. According to Al-Refaie et al. [ 1 ], posterior chest wall chondrosarcoma is uncommon, representing only 2.2% of cases. The main therapy is radical surgical excision with generous margins, in order to avoid recurrences. Such resections implicate full-thickness resection involving one or several ribs and/or the sternum, leaving a combined defect of bone and soft tissue, and exposing the lung or mediastinum [ 2 ].
Common repair of full-thickness chest wall defects utilizes a synthetic mesh to close the skeletal defect, whereas soft tissue coverage is obtained with myocutaneous flaps [ 3 ]. The combination of a polytetrafluoroethylene mesh and titanium rib implants has proved to be effective for extensive thoracic skeleton reconstruction, guaranteeing both air-tightness and stability. A non-rigid prosthesis may be sufficient to reconstruct posterior defects. Reconstruction after total vertebral body resection requires posterior stabilization and insertion of titanium mesh cages anteriorly. Well-vascularized soft tissue coverage is essential to avoid foreign material infection. To achieve that goal, the transposition of the ipsilateral pedicled myocutaneous latissimus dorsi flap is usually performed [ 4 ].
In the case of posteriorly located large full-thickness defects, the ipsilateral latissimus dorsi muscle is at least partly included in the resection specimen. The free contralateral myocutaneous latissimus dorsi flap is a valuable option to achieve effective soft tissue coverage [ 5 ]. The deep inferior epigastric perforator flap and the tensor fascia lata flap are available alternatives. A partial or total resection of the ipsilateral latissimus dorsi muscle usually leaves generous stumps of its pedicle, which represent the optimal site for the anastomosis with the contralateral latissimus dorsi free flap, with a perfect match of diameter.
With its dimensions averaging 35 × 20 cm, the latissimus dorsi muscle is the largest muscle of the body. In case of exceptionally wide resections, the latissimus dorsi flap may be insufficient. A second flap transposition is then required to cover the entire defect. Instead of harvesting another flap from an additional donor site, the use of a combined flap appears as the most suitable alternative. Both latissimus dorsi and serratus anterior muscles are vascularized by the thoracodorsal pedicle and can be harvested together as a generous combined myocutaneous flap on a unique vascular pedicle. In our case, this original crossover combined free flap ensured a sustainable and effective coverage after extended full-thickness posterior chest wall resection.
Conflict of interest: none declared.
REFERENCES




