-
PDF
- Split View
-
Views
-
Cite
Cite
Yong Soo Choi, Young Mog Shim, Jhingook Kim, Kwhanmien Kim, Recurrence-free survival and prognostic factors in resected pN2 non-small cell lung cancer, European Journal of Cardio-Thoracic Surgery, Volume 22, Issue 5, November 2002, Pages 695–700, https://doi.org/10.1016/S1010-7940(02)00473-6
Close - Share Icon Share
Abstract
Objective: We sought to evaluate recurrence pattern and prognostic factors of recurrence-free survival in surgically resected N2 non-small cell lung cancer. Methods: Between September 1994 and December 1999, 564 patients underwent operation for non-small cell lung cancer at our institute. Of these 564 patients, 101 patients were found to have pathologic N2 disease. Systematic mediastinal lymph node dissection was performed in all these patients. Recurrence was determined and nineteen clinicopathologic prognostic factors were evaluated in relation to recurrence-free survival. Results: Complete resection rate was 83.2% and overall 5-year survival was 23.3%. Locoregional and distant metastasis were detected in 50 of 101 patients (49.5%) during follow-up. Five-year recurrence-free survival was 19.6%. Among 19 clinicopathologic prognostic factors, incomplete resection and non-downstaging after neoadjuvant therapy were unfavorable prognostic factors in univariate analyses. Clinical N2 status, multiple N2 nodes, and cell type of adenocarcinoma showed poor prognosis but were not statistically significant. Postoperative chemotherapy showed good prognosis but was not statistically significant. Multivariate analysis showed that significant favorable prognostic factors were complete resection and adjuvant chemotherapy. Conclusions: Complete resection and responsiveness to neoadjuvant therapy were the most important favorable prognostic factors in recurrence-free survival. Postoperative chemotherapy was also a favorable prognostic factor but not statistically significant in recurrence-free survival in pN2 non-small cell lung cancer.
1 Introduction
It is controversial that surgical treatment of N2 disease should always be undertaken. Some authors reported that the preoperative finding of N2 disease is a poor sign of prognosis [1–3]. Non-small cell lung cancer has a low 5-year survival rate and its poor prognosis is related to distant and locoregional recurrences. We reviewed cases of pathologically proven N2 disease in our institute and tried to find out their recurrence-free survival and prognostic factors. This study reports recurrence pattern, recurrence-free survival and clinicopathologic prognostic factors in pathologic N2 disease.
2 Materials and methods
Between September 1994 and December 1999, 564 consecutive patients underwent operation for non-small cell lung cancer by three operators at our institute. Fifteen were women and 86 were men. Their age varied from 34 to 78 years, with a median of 60 years. All patients underwent thoracic computed tomography (CT) scan and those who have a cell type of adenocarcinoma or neurological symptoms also underwent brain CT. Clinical staging was decided by bronchoscopy, chest CT scan, abdominal ultrasonogram and bone scan finding. Lymph nodes with a shortest diameter of 10mm or more were considered enlarged. Mediastinal lymph node labeling was done according to the classification of Naruke and colleagues. Clinical or pathological staging was based on the TNM classification of the International Union Against Cancer, 5th edition. Of these 564 patients, 101 patients (17.9%) have pathologic N2 disease. We did not perform mediastinoscopy in every patient especially in the early period of the study. Mediastinoscopy was performed in 61 patients (60.4%) of 101 patients and another 40 patients underwent thoracotomy without mediastinoscopy. Nowadays we try to perform mediastinoscopy before thoracotomy on every patient even with N0 disease.
Neoadjuvant chemotherapy or chemoradiotherapy was indicated in the patients mediastinoscopically N2-positive or highly N2-suspicious in imaging study. Two cycles of cisplatin and etoposide were included in neoadjuvant chemotherapy and radiation of 45 Gy was added in some patients. In the same period, 48 patients of 564 patients had entered neoadjuvant therapy setting and 19 of 48 patients remained N2 in spite of neoadjuvant therapy and they were included in this study population (29 patients were excluded due to progression of tumor or downstaging to pathologic N0–N1 disease). Among these 19 patients, eight had N2 disease at mediastinoscopy and underwent lung resection after neoadjuvant therapy. Another 11 patients received neoadjuvant therapy due to definite mediastinal lymphadenopathy on CT finding.
Routine systematic hilar and mediastinal lymph node dissection was performed in all patients even if clinical lymph node staging was N0 or N1. Curativity was considered in case of complete resection. Incomplete resection of tumor was defined in case of tumor-positive resection margin at microscopic findings at permanent pathological findings. Operative mortality included intraoperative death and postoperative 30-day death due to any cause. Postoperative chemotherapy was indicated in advanced T status and tolerable performance status. Postoperative radiotherapy was indicated in incomplete resection and multiple nodal metastases.
In a retrospective review of 101 pathologic N2 patients, 19 clinicopathologic prognostic factors were collected: (1) clinical characteristics (age and sex), (2) clinical staging and type of treatment (clinical T status, clinical N status, lobectomy or pneumonectomy, neoadjuvant therapy, radiotherapy, chemotherapy and curativity), (3) characteristics of pathological findings (cell type of adenocarcinoma, differentiation, primary tumor size, pathological T status, pathological TNM stage, pleural invasion, vascular invasion, intrapulmonary metastasis, number of metastatic mediastinal lymph nodes and number of station of positive mediastinal lymph nodes).
Recurrence was evaluated with our hospital records and information from other hospitals. Recurrence pattern was classified into two categories: locoregional and distant metastasis. Locoregional recurrence included cancer development to supraclavicular nodes, mediastinal nodes, pleural effusion or seeding, bronchial stump and ipsilateral lung. Distant metastasis categorized metastasis to contralateral lung, brain, bone, liver, adrenal and other organs. Simultaneous locoregional and distant metastasis was considered distant metastasis group. Survival was calculated by the Kaplan–Meier method. Length of recurrence-free survival was defined as the interval in months from the operation to the detection of recurrence or the interval to death in cases that the cause of death was not identified or evidence of recurrence was not found before death. On follow-up telephone call some patients were found to have died and we were not informed of their cause of death, so we selected recurrence-free survival to include these patients in our study and did not consider them censored but event cases in statistical analysis. The log-rank statistic was used for univariate analysis and Cox regression was applied for multivariate analysis. Forward conditional method was used in Cox regression and a 0.10 level of significance was selected for entering or removing of covariate from a model. Statistical package was SPSS 8.0.
3 Results
3.1 Survival of total patients
Five (4.9%) of 101 patients died of respiratory failure within 30 days of operation. Follow-up data was collected in 96 patients who survived over 30 days after operation. Follow-up period was 19.5 months in median value and ranged from 2 months to 69 months. Sixty-two patients died during follow-up. The overall survival curve is depicted in Fig. 1 . Overall 2-year survival was 44.0% and 5-year survival was 23.3%. One patient died by suicide 5 months after operation and his data were counted as censored. All mortality cases except this patient were considered event cases in the analysis of recurrence-free survival. Seventy-one patients were grouped as event cases in recurrence-free survival. Fifty patients of 71 patients revealed recurrence and 21 of 71 patients died without knowing the status of recurrence. Actually 11 of 50 patients who developed recurrence were alive at the end-point of the study and they were grouped as censored cases. Three of these patients survived over 12 months after detection of recurrence: one patient underwent completion pneumonectomy for recurrence in ipsilateral remnant lung, the second received chemotherapy for recurrence in both lungs, and the third received radiotherapy for intrapulmonary metastasis.
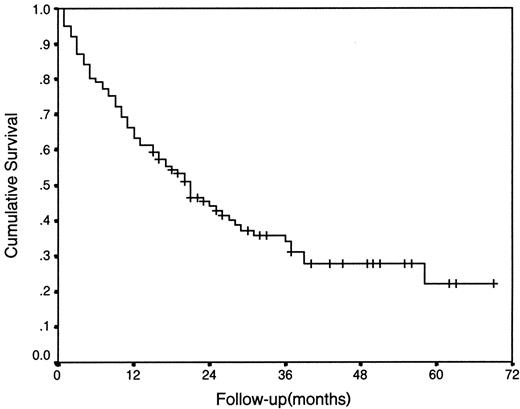
Overall survival curve of 101 patients with resected pN2 disease.
3.2 Recurrence pattern
Cancer recurrence was detected in 50 patients (49.5%) after resection. Interval from the operation to recurrence varied from 1 to 45 months and its median value was 9.5 months. The initial recurrence site was analyzed and is presented in Table 1 . Distant metastasis was identified in 38 (76%) of 50 patients including simultaneous locoregional and distant metastasis. Locoregional recurrence was found in 12 (24%) of 50 patients. The most common site of distant recurrence was contralateral lung and the most common site as a locoregional recurrence was intrapulmonary metastasis. Treatments for recurrences were undertaken in 39 (78%) of 50 patients: radiotherapy in 24, chemotherapy in 10, chemoradiotherapy in two, operation for brain metastasis in four, completion pneumonectomy in two, and wedge resection in one patient. Eleven patients did not receive any treatment. Interval from initial detection of recurrences to death was available in 35 patients and its median value was 8 months (range: 1–31 months).

3.3 Clinicopathologic factors and recurrence-free survival
Nineteen clinicopathologic factors were analyzed with relation to recurrence-free survival (Table 2) .
Recurrence-free survival (RFS) according to the clinicopathologic factors
3.4 Univariate analyses of prognostic factors
With regard to clinical characteristics, no significant prognostic factors were found. In clinical staging and type of treatment, curativity and neoadjuvant therapy were statistically significant prognostic factors. Complete resection was done in 84 (83.2%) of 101 patients. Complete resection rate was higher, though not statistically significant, in the patients who underwent mediastinoscopy (86.9 vs. 75.0%). The incompletely resected group of patients showed a follow-up period of maximal 26 months and 5-year survival could not be calculated. Complete resection was an essential factor for good prognosis after resection. The result revealed that non-downstaging after neoadjuvant therapy was an unfavorable prognostic factor. It should be noted that 19 patients of the neoadjuvant group had not been downstaged after neoadjuvant therapy and their N2 status persisted after neoadjuvant therapy. Clinical N2 status was also a poor prognostic sign but was not statistically significant. Postoperative chemotherapy was a favorable factor but was not statistically significant. Characteristics of pathological findings showed no statistically significant prognostic factors, but patients with only single metastatic mediastinal lymph node had better results in recurrence-free survival than those with multiple nodes. Cell type of adenocarcinoma influenced recurrence-free survival but was not statistically significant.
3.5 Multivariate analysis of prognostic factors
All 19 prognostic factors were evaluated with Cox regression. Table 3 shows that only curativity was a significant prognostic factor in multivariate analysis. Patients who received postoperative chemotherapy revealed better recurrence-free survival but the P value was more than 0.05.
Multivariate analysis of prognostic factors in resected pN2 disease
4 Discussion
The 5-year survival of 23.3% is higher than in other series [1,4–6]. We can explain our better result by high complete resection rate of our cases. Our data show a resectability rate of 83.2% in pN2 non-small cell lung cancer and this figure is high and comparable to other reports [1,3,6,7]. We confirmed that mediastinoscopy helps to avoid futile incomplete resections [1,3,4,6].
Distant metastasis comprised 78% of recurrence and this figure is similar to other series [8]. Deaths after resection of non-small cell lung cancer result mainly from cancer recurrence. In our results, the patients who developed cancer recurrences died after a median period of 8 months. Therefore we added cancer recurrence to analyses of survival of pN2 disease. It is logical that we include 21 deaths whose causes of death were not known in the recurrence group.
It is of no doubt that complete resection is the most important prognostic factor. According to some reports [9–14] neoadjuvant therapy has been known to increase survival of stage IIIA by downstaging after neoadjuvant therapy. We confirmed that patients who are not downstaged do not benefit from surgical resection. Comparative analysis between responders and non-responders is in progress in the patients who received neoadjuvant therapy followed by surgery in our hospital.
Some authors reported that clinical N status was significant prognostic factor in surgically resected pN2 non-small cell cancer [1,6,15]. Most of those of clinical N2 in our study population had unforeseen pN2 after CT and mediastinoscopy so it is reasonable that their prognostic value was insignificant. The number of metastatic mediastinal lymph nodes is considered one of the important prognostic factors [4,16,17]. In our study, metastasis to more than single mediastinal lymph nodes was a relevant unfavorable prognostic factor and its P value was close to 0.05 in univariate study.
No prospective randomized trial has shown that any regimen improves survival with adjuvant therapy in patients with locally advanced non-small cell lung cancer. According to the research of the Lung Cancer Study Group on patients with stage II or IIIA who had undergone resection, postoperative radiation gained significantly lower local recurrence rate but no benefit for survival [18]. This result is understandable since patients with non-small cell lung cancer die of disseminated disease. Some studies have randomized data on disseminated disease receiving systemic chemotherapy or supportive care [19–22]. Meta-analyses [22,23] generally showed that there was a 10% increase in survival at 1 year, but an increase of only 2 months in median survival. A practically prospective randomized trial of adjuvant therapy is not easy to perform because it is not acceptable who will be assigned to the no-therapy arm.
In conclusion, although some prognostic factors influence recurrence-free survival in surgically resected pN2 non-small cell lung cancer, complete resection is the most important factor to get better results in recurrence-free survival. Systematic mediastinal lymph node dissection is essential to verify complete resection of lung cancer. Downstaging by neoadjuvant therapy may play an important prognostic factor and adjuvant systemic chemotherapy may help to avoid disseminated disease in surgically resected non-small cell lung cancer.




