-
PDF
- Split View
-
Views
-
Cite
Cite
Randall K. Wolf, Toshiya Ohtsuka, John B. Flege, Early results of thoracoscopic internal mammary artery harvest using an ultrasonic scalpel, European Journal of Cardio-Thoracic Surgery, Volume 14, Issue Supplement_1, October 1998, Pages S54–S57, https://doi.org/10.1016/S1010-7940(98)00105-5
Close - Share Icon Share
Abstract
Objective: We developed a thoracoscopic internal mammary artery harvest technique using an ultrasonic scalpel, the Harmonic Scalpel (Ethicon Endo-Surgery, Cincinnati, OH). This is the first report of 9 month follow-up using this technique. Methods: The Harmonic Scalpel is activated ultrasonically by vibrating at 55 000 Hz. Compared with electrocautery, lower heat (≪100°C) and less smoke are generated. Thoracoscopic harvest using the Harmonic Scalpel with a hook blade was performed for 48 internal mammary arteries (42 left, six right) in 46 patients. Four (8.7%) of them were redo cases. The left internal mammary to left anterior descending artery and the right internal mammary to right coronary artery anastomoses were accomplished on the beating heart. Two left internal mammary arteries were sequentially, anastomosed to diagonal branches. Graft flow velocity was evaluated with pulsatile wave color Doppler test on the second or third postoperative day and repeated 3 and 6 months later. Results: The mean harvest time was 65 min (range 35–95 min) for the left internal mammary artery and 37 min (range 25–45 min) for the right internal mammary artery. One left internal mammary artery was lost due to intimal dissection. The Harmonic Scalpel-related morbidity was transient left phrenic palsy in one case and mild heat injury at the skin incision in the majority of cases. One Patient (2.2%) expired due to ischemic bowel on the second postoperative day. At a mean of 9 months follow-up, 45 alive patients have been free of angina. Doppler studies revealed diastolic augmentation of the graft flow velocity in 22 left and two right internal mammary arteries on the second or third postoperative day and 23 left and five right internal mammary arteries 3 and 6 months after operation. Conclusions: Thoracoscopic internal mammary artery harvest is feasible and facilitated by the use of the Harmonic Scalpel. Early results of this technique are encouraging.
1 Introduction
The thoracoscopic technique allows for complete left/right internal mammary artery (L/RIMA) harvest up to their origin in minimally invasive coronary artery bypass grafting (MICABG) [1, 4, 5]. This technique is demanding particularly in the left hemithorax where the LIMA overlies the left ventricle. An ultrasonic scalpel, the Harmonic Scalpel (Ethicon Endo-Surgery, Cincinnati, OH), has been developed and utilized for laparoscopic surgery [9, 14, 16]. We have employed the Harmonic Scalpel to facilitate IMA harvest through thoracoscopy [11]. In this communication, early results with thoracoscopic IMA harvest using the Harmonic Scalpel are reported.
2 Materials and methods
Since December 1995, 48 consecutive IMA (42 LIMAs and six RIMAs) harvests in 46 cases have been accomplished thoracoscopically with the Harmonic Scalpel. Bilateral mammary harvests were performed in two patients. Four (8.7%) of 46 were redo cases. Some IMAs had been examined with preoperative angiography. The LIMAs were utilized for anastomoses to the mid-portion of the led anterior descending artery (LAD) and the RLMAs were for the right coronary artery. In two patients. sequential anastomoses were completed to the LAD and diagonal vessels.
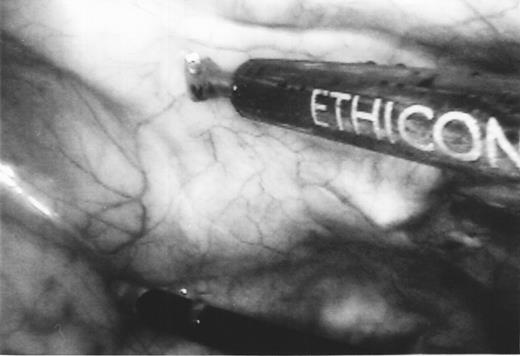
The Harmonic Scalpel is activated ultrasonically with vibration up to 55 000 Hz, producing lower heat (≪100°C) and less smoke than standard electrocautery [2,3]. A hook-shaped blade allows for coagulating and cutting of the vessels (Fig. 1).

Photograph of hook-shaped blade of the Harmonic Scalpel with hard sheath (HDH14) which eliminates heat injury to the skin.
The thoracoscopic mammary harvest method using the Harmonic Scalpel with a hook blade was devised by the senior author (R.K.W.). All the 48 mammary harvests reported here were consistently performed by R.K.W. Details of this method have been described elsewhere [11]and a summary is described below.
Patients are placed in the 20-degree left/right side-up position, exposing the left/right axilla extensively for L/RIMA harvests.
One lung ventilation and insufflation with CO2 gas was required.
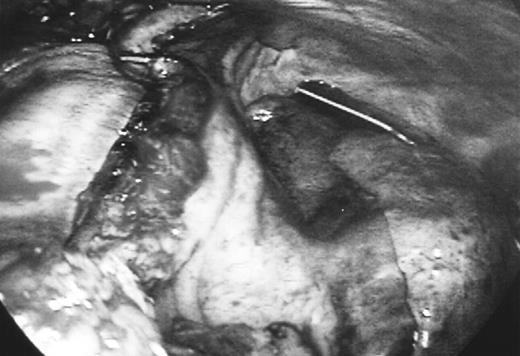
Harmonic Scalpel with hook blade and endoscopic kittner dissector are utilized (Fig. 2).
Branches of the IMA are coagulated with the blunt side of the blade and divided with the hook side.
IMAs are pedicled up to the upper margin of the first rib or higher.
Thoracoscopic view of the Harmonic Scalpel and endoscopic kittner dissector used for IMA harvest in the insufflated left hemithorax. Arrows, proximal portion of the LIMA; Arrow head, first rib.
Before dividing the IMA pedicle distally, in situ graft flow was checked with a hand-held Doppler probe. Just after completion of coronary anastomosis, the graft flow was examined with a transit time flow probe (Transonic Systems, Ithaca, NY). On the second or third postoperative day, a pulsatile wave color Doppler study was performed for subclavian and mammary arteries and repeated 3 and 6 months later. In this study, velocities of the IMA were measurer bilaterally and diastolic augmentation in the grafted IMA was documented [6]. In selected patients. an intraoperative or postoperative arteriogram was performed.
3 Results
All the 48 IMA harvests were completed thoracoscopically, using only the Harmonic Scalpel and endoscopic kittner dissector. Each pedicle was dissected up to the upper margin of the first rib or higher and down to the fifth rib. In four redo cases, prior to IMA harvest, mediastinal pleural adhesions were safely freed with the Harmonic Scalpel. The mean harvest time was 65 min (range 35–95 min) for the LIMA and 37 min (range 25–45 min) for the RIMA. Vascular branches were coagulated without charring and divided with excellent hemostasis. By using warmed CO2 insufflation, an intrathoracic space between the anterior chest wall and the ventricle was produced, providing a satisfactory view for the IMA harvest maneuver. Hemodynamics were stable in each patient during insufflation with an intrathoracic pressure of 8–10 mmHg. After coronary anastomosis on the beating heart, each IMA pedicle had a comfortable lie on the mediastinum with no tension (Fig. 3).
Thoracoscopic view of the LIMA graft after completion of anastomosis to the LAD. The LIMA was harvested higher than the first rib and the graft had a comfortable lie on the mediastinum with no tension.
In situ IMA flow assessment performed before IMA division revealed excellent Doppler signal in all but one in which intimal dissection occurred. The graft flow measured immediately after coronary anastomosis ranged from 20 to 110 ml/min. In one patient, intraoperative coronary angiography was performed to confirm patency of sequential anastomoses to the LAD and the second diagonal branch. Pulsatile wave color Doppler test was accomplished for 22 LIMAs and two RIMAs on the second or third postoperative day. Each graft had augmented velocities in the diastolic phase. One patient underwent angiography on the second postoperative day and the IMA graft to the LAD was widely patent.
As of November 1997, follow-up was 100% complete and the mean follow-up period was 9 months (range 6–24 months). One patient (2.2%) died due to ischemic bowel on the second postoperative day. Forty-five patients have been free of angina. One patient had transient (5 days) left phrenic palsy after LIMA–LAD procedure. Doppler studies have been achieved for 32 IMAs 3 and 6 months after operation. Four of them were undetectable due to incomplete visualization. In the remaining 28 (23 LIMAs, four RIMAs), diastolic augmentation of the flow velocity was documented (Fig. 4a,b). In one patient, 6 months postoperative angiography documented patent LIMA–LAD anastomosis.
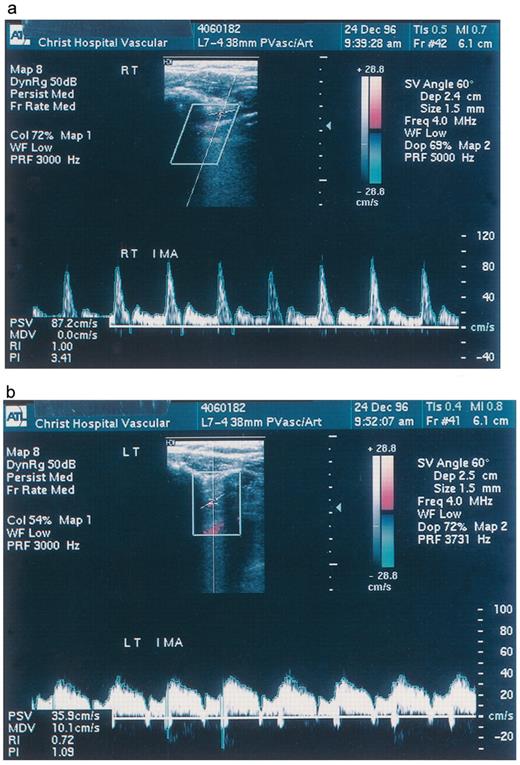
Pulsatile wave color Doppler study for the IMA performed 6 months after operation. In the unused RIMA, the flow was mainly systolic (a). Diastolic flow velocity remarkably increased in the LIMA anastomosed to the LAD (b).
4 Discussion
Thoracoscopy with insufflation provides for excellent visualization of the IMA and the anatomic relationships of the adjacent structures. Particularly in the proximal portion of the IMA, the relationship to the phrenic nerve can be clearly appreciated and dissection higher than the nerve is feasible (Fig. 2) [10, 12, 15]. When the lung is reexpanded after completion of coronary anastomosis, the edge of the lung moves beyond the IMA graft. In our experience, the IMA pedicle, anastomosed to the mid-portion of the LAD, should be dissected from its bed at least up to the upper margin of the first rib so that IMA graft is tension-free and free of interference from pulmonary motion. In addition to excellent visualization for the IMA, thoracoscopic complete IMA dissection can avoid rib resection via thoracotomy and thoracoscopy allows the surgeon to place an anterior thoracotomy directly over the coronary target site.
The advantages of the Harmonic Scalpel are less smoke, lower heat creation and fewer instrument transfers compared with electrocautery [11]. In 1995, we completed a survivor mongrel dog experiment in which the Harmonic Scalpel was compared with electrocautery during thoracoscopic IMA harvest. Each animal had IMA harvest on one side with Harmonic Scalpel and on the other with electrocautery. The electrocautery used was bipolar for branches. The follow-up included angiograms on postoperative day 5 and histologic sections on all explanted IMAs at animal sacrifice on day 5. Histologic sections were reviewed using trichrome stains by a pathologist blinded to the method of harvest. The results were that all IMAs were patent at angiography on day 5 and all histologic sections revealed no injury to the IMA at branch points. This animal experiment confirmed that the Harmonic Scalpel was safe for IMA dissection and branch coagulation. When compared with electrocautery, considerably less smoke was produced by the Harmonic Scalpel. providing clear thoracoscopic views. In addition, fewer instrument transfers were required using the Harmonic Scalpel, as the instrument facilitates dissection of all tissues, as well as coagulation and transection of side branches.
A device producing minimal smoke is very helpful, eliminating the need for suctioning in the closed insufflated chest cavity. Coulson et al. reported tissue temperature rose by 1°C or lower 0.5 cm away from the activated Harmonic Scalpel [7]. Actually, no charring was appreciated at coagulated IMA branches in our series and the ultrasonic scalpel might function more protectively for IMA harvest than electrocautery. To accomplish harvest higher than the first rib in the left. attention should be paid to the crossing of the IMA and the phrenic nerve [8, 10]. There was minor heat-related morbidity with the skin [13]. The Harmonic Scalpel had been placed directly through the skin incision to improve its intrathoracic mobility and the vibrating shaft caused thermal injury at the incision with white blanching of the dermal margin. In the latest two cases, a new shaft with a hard sheath (HDH 14, Fig. 1) was utilized and protected the skin perfectly.
Thoracoscopic techniques do require special skills such as sophisticated hand-eye coordination and handling of unique endoscopic instruments and there is a learning curve. We believe the Harmonic Scalpel facilitates the thoracoscopic IMA harvest technique in MICABG procedures, allowing for safe and long dissection of the IMA higher than the first rib. Early results with Doppler study were encouraging. We understand that postoperative angiogram is a most ideal follow-up in these patients. In our current situation, however, non-invasive, cost-effective follow-up for MICABG has been accepted from both a patient and financial standpoint. Although we recognize that longer follow-up and experience are needed, it is concluded that thoracoscopic IMA harvest using the Harmonic Scalpel is a reliable and reproducible technique in MICABG.
The assistance of Beverly Hahn. R.N., B.E.S is greatly appreciated.
References
- angina pectoris
- gastrointestinal tract vascular insufficiency
- doppler color flow
- internal thoracic artery
- anterior descending branch of left coronary artery
- right coronary artery
- doppler echocardiography
- doppler ultrasound
- anastomosis, surgical
- diastole
- tissue dissection
- follow-up
- heat (physical force)
- paralysis
- smoke
- surgical procedures, operative
- thoracoscopy
- tissue transplants
- electrocoagulation
- heart
- morbidity
- skin
- thermal injury
- ultrasound surgical units
- expiration, function
- harmonic scalpels
- harmonics
- fluid flow




