-
Views
-
Cite
Cite
Jo-Nan Liao, Yi-Hsin Chan, Ling Kuo, Chuan-Tsai Tsai, Chih-Min Liu, Tzeng-Ji Chen, Gregory Y H Lip, Shih-Ann Chen, Tze-Fan Chao, Temporal trends of prescription rates, oral anticoagulants dose, clinical outcomes, and factors associated with non-anticoagulation in patients with incident atrial fibrillation, European Heart Journal - Quality of Care and Clinical Outcomes, Volume 11, Issue 3, April 2025, Pages 300–311, https://doi.org/10.1093/ehjqcco/qcaf002
Close - Share Icon Share
Abstract
To analyse the temporal trends of oral anticoagulant (OAC) prescription, direct oral anticoagulant (DOAC) dose, clinical outcomes, and factors associated with non-anticoagulation in patients with incident atrial fibrillation (AF).
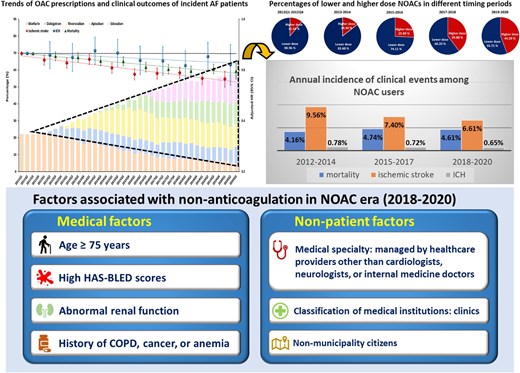
During 1 January 2011–31 December 2020, a total of 249 107 patients with newly diagnosed AF were identified, and the 1-year risks of ischaemic stroke, intracranial haemorrhage (ICH), and all-cause mortality were analysed. OAC prescription increased from 22.1% in 2011 to 57.7% in 2020 with DOAC accounting for 91.0% of overall OAC prescriptions. Compared to patients with incident AF diagnosed in 2011, there were increasing trends for a greater decrease in the risks of ischaemic stroke during 2012–2020 and mortality during 2014–2020, while the risk of ICH did not change significantly. For DOAC users, higher dose use increased from 11.04% in 2012 to 44.29% in 2019–2020 temporally associated with a lower risk of ischaemic stroke in the years 2015–2017 and 2018–2020 compared to 2012–2014. Determining factors refraining from OAC use included some ‘patient-related factors’ and ‘non-patient’ factors (AF diagnosed at clinics by physicians other than cardiologist/neurologist/internal medicine and citizens outside municipalities).
There was an increasing trend of OAC prescription, temporally associated with a decreased risk of ischaemic stroke and mortality. Among DOACs users, the risk of ischaemic stroke declined gradually, partly explained by the increasing prescriptions of higher dose DOACs. Both patient and non-patient factors were associated with non-anticoagulation. Further efforts are required to increase OAC prescription.