-
Views
-
Cite
Cite
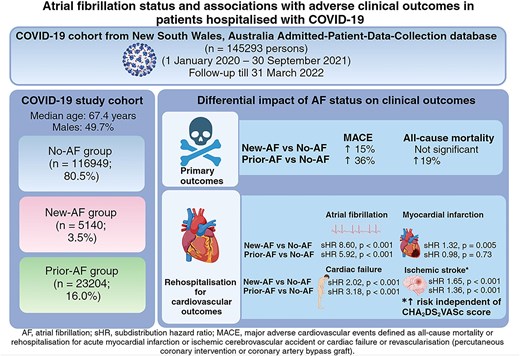
Jia Yi Anna Ne, Clara K Chow, Vincent Chow, Karice Hyun, Leonard Kritharides, David Brieger, Austin Chin Chwan Ng, Atrial fibrillation status and associations with adverse clinical outcomes in patients hospitalized with COVID-19: a large unselected statewide population-linkage study, European Heart Journal - Quality of Care and Clinical Outcomes, Volume 11, Issue 3, April 2025, Pages 291–299, https://doi.org/10.1093/ehjqcco/qcae115
Close - Share Icon Share
Abstract
Atrial fibrillation (AF) is common in COVID-19 patients. The impact of AF on major-adverse-cardiovascular-events (MACE is defined as all-cause mortality, myocardial infarction, ischaemic stroke, cardiac failure, or coronary revascularization), recurrent AF admission, and venous thromboembolism in hospitalized COVID-19 patients is unclear.
Patients admitted with COVID-19 (1 January 2020 to 30 September 2021) were identified from the New South Wales Admitted-Patient-Data-Collection database, stratified by AF status (no-AF vs. prior-AF or new-AF during index COVID-19 admission) and followed-up until 31 March 2022. Multivariable Cox regression and competing risk analyses were performed to assess the impact of AF on MACE and non-fatal outcomes respectively. Our cohort comprised 145 293 COVID-19 patients (median age 67.4 years old; 49.7% males): new-AF, n = 5140 (3.5%); prior-AF, n = 23 204 (16.0%). During a median follow-up of 9 months, prior-AF and new-AF patients had significantly higher MACE events (44.7% vs. 36.2% vs. 18.0%) and all-cause mortality (36.0% vs. 28.7% vs. 15.2%) compared to no-AF patients (both logrank P < 0.001). After adjusting for age, gender, intensive-care-unit admission, referral source, and comorbidities, compared to no-AF, new-AF and prior-AF groups were independently associated with MACE [adjusted hazard ratio (aHR) = 1.15, 95% confidence interval (CI) = 1.09–1.20; aHR = 1.36, 95% CI = 1.33–1.40, respectively]. Competing risk analyses showed rehospitalization rates for ischaemic stroke, cardiac failure, and AF, but not venous thromboembolism, were significantly higher in these patients. Both new-AF and prior-AF patients had higher rehospitalization rates for ischaemic stroke compared to no-AF patients, independent of CHA2DS2VASc.
COVID-19 patients with AF are at high risk of adverse clinical outcomes. Such patients may need increased surveillance and consideration for early anticoagulation.