-
PDF
- Split View
-
Views
-
Cite
Cite
Lorena Iezzi, Anna Sorella, Kristian Galanti, Sabina Gallina, Anwar A Chahal, Barbara Bauce, Alberto Cipriani, Rui Providencia, Luis R Lopes, Fabrizio Ricci, Mohammed Y Khanji, Arrhythmogenic cardiomyopathy diagnosis and management: a systematic review of clinical practice guidelines and recommendations with insights for future research, European Heart Journal - Quality of Care and Clinical Outcomes, 2025;, qcaf029, https://doi.org/10.1093/ehjqcco/qcaf029
Close - Share Icon Share
Abstract
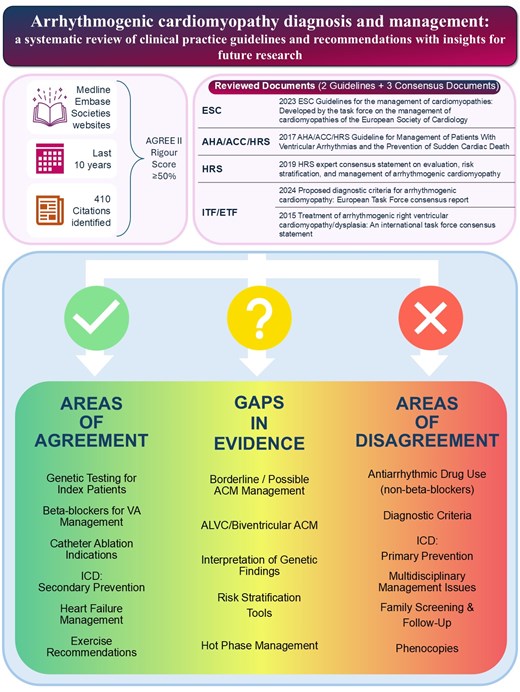
Arrhythmogenic cardiomyopathy (ACM) is addressed in international guidelines and expert consensus statements. To assist clinicians in their routine practice and support decision-making, we performed a systematic review of the most relevant guidelines and recommendations for ACM diagnosis and management. Our search, covering MEDLINE, EMBASE, and resources from scientific societies over the last 10 years, identified two guidelines and three consensus statements that met rigorous inclusion criteria for detailed analysis.
In the examined documents, key areas of agreement included the critical role of cardiac imaging for initial diagnosis and ongoing monitoring, genetic testing in index patients, ventricular arrhythmia management, catheter ablation indications, heart failure treatment strategies, and exercise recommendations. However, significant differences were found in definitions and diagnostic criteria for ACM, interpretation of phenocopies, management of family members, and criteria for ICD implantation. Additional discrepancies emerged regarding the role of multidisciplinary teams, non-cardiac surgical considerations, atrial fibrillation management, and reproductive issues.
Crucially, there remain considerable gaps in evidence, especially in areas such as the management and follow-up of patients with potential or borderline ACM diagnoses, as well as the care of their relatives. The clinical implications of genetic findings, along with the clinical management of left-dominant, biventricular phenotypes, and hot phases of disease, are also insufficiently addressed. Furthermore, a critical shortfall is the lack of externally validated risk assessment tools to guide clinical decision-making. Bridging these gaps could help guiding future research and guideline development towards improving patient outcomes.
Author notes
Fabrizio Ricci and Mohammed Y. Khanji shared senior authorship


