-
PDF
- Split View
-
Views
-
Cite
Cite
Stephanie Loebig, Sebastian Weyand, Alexander Metzger, Peter Seizer, Mechanical thrombectomy of a clot-in-transit followed by low-dose systemic lysis: a case report of pulmonary embolism and progressive right heart failure, European Heart Journal - Case Reports, Volume 9, Issue 2, February 2025, ytaf034, https://doi.org/10.1093/ehjcr/ytaf034
Close - Share Icon Share
Abstract
Acute pulmonary embolism (PE) is a life-threatening situation. While anticoagulation should be initiated without any delay in all patients with an intermediate or high clinical probability of PE, individual acute phase treatment in patients with intermediate or intermediate-high-risk PE still can be optimized.
An 82-year-old female patient was referred to our emergency department after experiencing syncope and acute onset of shortness of breath. Computed tomography (CT) of the chest showed central and extensive peripheral PE. Echocardiography additionally revealed a massive and highly mobile clot-in-transit located in the right atrium (RA). Given the size and mobility of the clot-in-transit, we chose to perform an off-label mechanical thrombectomy. Due to repeated PE with progressive right ventricular (RV) failure and high peripheral thrombus burden, we decided to perform low-dose systemic lysis. After 24 h, she showed significant clinical improvement and was discharged later with recovered RV function and dimensions.
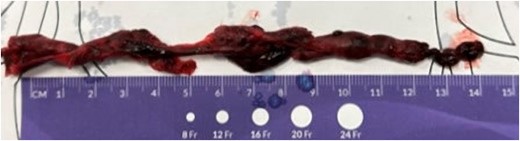
In that case, acute PE was complicated by the presence of a large clot-in-transit in the RA. Initially, there was no indication for mechanical thrombectomy or systemic lysis for the patient’s intermediate to high-risk PE. The risk of embolization of the very large clot-in-transit prompted us to remove the mobile thrombus mechanically. When the repeated PE resulted in an increase in afterload and progressive right heart failure, we decided to perform low-dose systemic lysis. The off-label use of the FlowTriever® prevented the impending embolization of the 14 cm long thrombus from the RA into the pulmonary circulation. In this case, lysis also appears to make sense, particularly given the high peripheral thrombus burden.
To acknowledge the critical importance of transthoracic echocardiography in diagnosing right heart thrombi.
To identify haemodynamic consequences of pulmonary embolism.
To be aware of the risk of repeated pulmonary embolism especially in the context of the presence of a clot-in-transit.
Introduction
Acute pulmonary embolism (PE) is a life-threatening condition that, depending on various risk factors, is associated with high morbidity and mortality. While anticoagulation should be initiated without delay in all patients with an intermediate or high clinical probability of PE,1 the individual acute phase treatment in patients with intermediate or intermediate-high-risk PE can still be optimized. We present the case of an 82-year-old female presenting with PE and a large clot-in-transit.
Summary figure
Case presentation
An 82-year-old female patient was referred to our emergency department after experiencing syncope and acute onset of shortness of breath during breakfast. Earlier that morning, immediately after getting up, she noticed a sharp pain in the back of her left lower limb. Besides that, there was no relevant past medical history. She and her husband made a stop nearby while travelling home from Italy.
At the initial presentation, she was in atrial fibrillation with a heart rate of 150 b.p.m. and a blood pressure of 108/63 mmHg. Otherwise, the physical examination was unremarkable. D-dimer levels were >99 000 µg/L (reference value: 750 µg/L). Consequently, we performed computed tomography (CT) of the chest, which revealed central and extensive peripheral pulmonary embolism (PE) with a high thrombus burden (Figure 1). At that time, echocardiography also revealed a massive and highly mobile clot-in-transit located in the right atrium (RA) (see VideoA, supplementary material). Although the right ventricular (RV) function was still preserved, RV dimensions were already mildly dilated. Ultrasound did not detect any residual deep vein thrombosis.
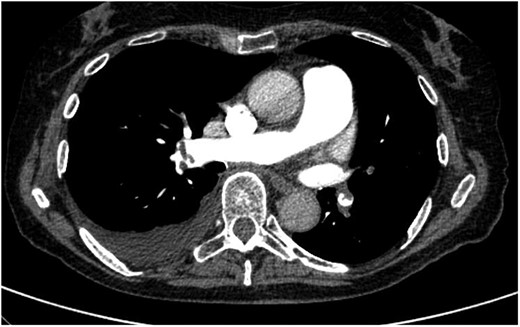
Initial computed tomography scan of the chest showing the predominantly high peripheral thrombus burden.
We immediately initiated anticoagulation with intravenous heparin. The patient’s PESI (Pulmonary Embolism Severity Index) score at the time of admission was 102, indicating a moderate risk of mortality (1.7%–3.5%). Due to RV dilatation, she was categorized in the intermediate-high-risk group for early mortality. According to the ESC Guidelines for the diagnosis and management of acute PE, there was—regarding PE—neither an indication for systemic thrombolysis nor for mechanical thrombectomy.1
Given the size and mobility of the clot-in-transit, we chose to perform an off-label mechanical thrombectomy using the FlowTriever® system. This is a catheter-based device designed to remove thrombi from circulation. Initially intended for the treatment of PE,2,3 it can also be used off-label to treat thrombi in other locations, such as the atria or ventricles. The FlowTriever offers the advantage of being minimally invasive, eliminating the need for thrombolytics, which can reduce the risk of bleeding. It also provides immediate haemodynamic improvements. However, there are some drawbacks. The large cannula size (20 or 22 French) may pose a risk of vascular injury, and the procedure requires significant expertise. Additionally, while off-label uses expand its potential applications, they also introduce increased uncertainty regarding efficacy and safety in those scenarios.
The procedure was planned and performed on Day 2 post-admission. For access, we used both femoral veins. Discs were placed in the pulmonary artery to minimize the risk of further embolization. The Triever24 device was advanced along the wire placed in the superior vena cava (SVC). After transthoracic echocardiographic control and alignment of the catheter position, thrombectomy of an ∼14 cm long thrombus was performed (Figure 2).
Following the procedure, we switched the anticoagulation from heparin to apixaban (5 mg twice daily). Despite oral anticoagulation and compression therapy for the legs, the patient experienced progressive clinical deterioration starting on Day 4 and peaking on Day 7 post-admission. During this period, she was receiving antibiotic therapy for infarct-related pneumonia (Cefotaxime 2 g i.v. twice daily for 10 days). Echocardiography on Day 7 revealed progressive RV failure with severe tricuspid regurgitation (TR). We repeated CT of her chest, which demonstrated central and progressive peripheral PE (Figure 3).

Computed tomography scan revealed repeated pulmonary embolism with progressive central and peripheral thrombus burden.
The patient’s risk profile had not changed. A second mechanical thrombectomy, this time targeting the pulmonary embolus, was still not indicated. However, due to the high peripheral thrombus burden, we decided to perform systemic lysis. To minimize the risk of bleeding, we opted for low-dose systemic lysis over 36 h (1 mg rt-PA/h in combination with therapeutic heparinization).4 After 24 h, the patient already showed significant clinical improvement. We discontinued lysis after an additional 12 h due to epistaxis.
Echocardiography revealed a decrease in RV dimensions and an improvement in RV function. TR improved from severe to mild. The patient was discharged on Day 17 post-admission in good functional condition and on oral anticoagulation with apixaban.
Discussion
We present a case of acute PE complicated by the presence of a large clot-in-transit in the RA. Initially, there was no indication for mechanical thrombectomy or systemic lysis for the patient’s intermediate-to-high-risk PE.1 However, the risk of embolization posed by the very large clot-in-transit prompted us to remove the mobile thrombus using the FlowTriever® system. When the repeated PE led to an increase in afterload and progressive right heart failure, we decided to perform low-dose systemic lysis. According to the guidelines, the patient’s risk profile did not justify either thrombectomy or full-dose systemic lysis.5
There are only a few studies demonstrating that low-dose systemic lysis can be safely administered to reduce pulmonary artery pressure and, consequently, RV afterload,6 without incurring the higher bleeding risk associated with full-dose systemic lysis.
In this case report, we describe a sequential therapeutic approach to two complications associated with acute PE: clot-in-transit and recurrent PE with a clinically significant increase in pulmonary artery pressure.7 The case demonstrates that combining therapy options is a viable treatment strategy for haemodynamically stable patients with intermediate-to-high risk. The off-label use of the FlowTriever® system successfully prevented the impending embolization of the 14 cm long thrombus from the RA into the pulmonary circulation. In this case, systemic lysis also proved beneficial, particularly given the high peripheral thrombus burden.
Lead author biography

Dr Stephanie Loebig is a cardiologist working at Ostalb Clinic Aalen in Germany. She has specialized in the field of cardiovascular imaging and is passionate about implementing different imaging modalities in the broad spectrum of cardiovascular interventions.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Consent: The authors confirm that the written consent for submission and publication of this case report, including images and associated text, has been obtained from the patient in line with COPE guidance.
Funding: None declared.
Data availability
The data underlying this article are available in the article and in its online Supplementary material.
References
Author notes
Conflict of interest: None declared.





Comments