-
PDF
- Split View
-
Views
-
Cite
Cite
Tuğçe Çöllüoğlu, Melahat Hicran Aksu, Orhan Önalan, Yeşim Akın, An interesting observation: prolonged green urine can be a combined effect of decreased liver and renal function in a patient with heart failure—a case report, European Heart Journal - Case Reports, Volume 7, Issue 12, December 2023, ytad570, https://doi.org/10.1093/ehjcr/ytad570
Close - Share Icon Share
Abstract
The administration of propofol and methylene blue (MB) can be associated with the appearance of prolonged green urine discoloration, particularly in patients with heart failure (HF) concomitant with renal and liver dysfunction. Understanding the reasons behind this phenomenon is of clinical significance.
A 79-year-old woman with a history of HF experienced dyspnoea and persistent green urine discoloration for a week, leading to her hospitalization for acutely decompensated HF. A recent dual-chamber rate-modulated-pacemaker implantation had necessitated propofol sedation and the administration of 100 mg of MB due to methaemoglobinaemia. Upon admission, the patient exhibited elevated levels of brain natriuretic peptide (BNP) and liver function tests, as well as a significant decrease in glomerular filtration rate (GFR). Initial therapy with intravenous furosemide yielded an inadequate response, requiring the initiation of combined diuretic therapy (CDT). The patient's condition improved with CDT, resulting in the normalization of BNP, liver function tests, and GFR, along with the restoration of normal urine colour lasting 12 days.
Our case report sheds light on the complex interaction between drug metabolic pathways and their potential for prolonged side effects, particularly in patients with multiorgan dysfunction. The association between propofol, MB, and green urine discoloration in the context of HF warrants further investigation, emphasizing the need for increased awareness of drug interactions and their implications in complex clinical scenarios.
Green discoloration of the urine is a benign and transient phenomenon in patients administered propofol or methylene blue (MB).
Green-hued urine is usually observed for 2–3 days following the administration of higher doses of MB and propofol.
Prolonged green urine may be difficult to observe in patients with heart failure (HF). However, prolonged green urine may appear in HF patients with multiorgan dysfunction as a result of reduced drug metabolism and excretion.
Introduction
Green discoloration of urine can be caused by dyes, infections, ingested substances, and drugs such as propofol, methylene blue (MB), cimetidine, amitriptyline, promethazine, methocarbamol, and indomethacin.1,2 The presence of a Pseudomonas infection in the urinary tract can result in the discoloration of urine, manifesting as a green hue. The green hue is attributed to the production of pyocyanin and pyoverdin pigments by the bacterium.3 Among the most frequently encountered ones in the literature are the side effects of propofol and MB administration.4,5 The green colour is due to the excretion of quinol derivatives resulting from the renal sulfo- and glucuro-conjugation of propofol.5 Also, MB is filtered by the kidneys and has no pathologic effects but may cause urine to have a bluish or greenish hue that is self-limiting.2 However, the green discoloration of the urine usually lasts 1 or 2 days after stopping both agents.5,6 In this case, we aimed to represent the combined effect of MB and propofol-induced green urine taking longer to return to a completely normal urine colour in the patient presenting with acute decompensated heart failure (HF) due to pacemaker-induced cardiomyopathy.
Summary figure
Case report
A 79-year-old woman with hyperlipidaemia and diabetes mellitus presented to the emergency department with dyspnoea and orthopnoea for 2 days due to fluid overload. It was ascertained that the patient had undergone dual chamber pacemaker implantation due to complete atrioventricular block 1 week prior to her hospitalization. The patient’s vital signs were recorded as follows: blood pressure of 110/75 mmHg, heart rate of 124 beats per minute with regular rhythm, respiratory rate of 28 breaths per minute, body temperature of 36.7°C, and oxygen saturation by pulse oximetry of 82% while breathing room air. On physical examination, the patient had signs of pulmonary congestion, and cardiovascular auscultation revealed a grade 2/6 systolic ejection murmur at the apex. The transthoracic echocardiography revealed a left ventricular ejection fraction ranging from 30% to 35%, along with a moderate level of mitral regurgitation and tricuspid regurgitation. The subcostal view revealed the presence of an enlarged inferior vena cava measuring 22 mm in diameter, with no indications of respiratory collapse. Upon admission, laboratory results indicated an increase in brain natriuretic peptide levels to 3148 pg/mL (0–100 pg/mL), as well as elevated levels of aspartate transferase (AST) at 335 U/L (5–34 U/L), alanine transferase (ALT) at 250 U/L (10–49 U/L), blood urea nitrogen at 99 mg/dL (10–49 mg/dL), and creatinine (Cr) at 1.3 mg/dL (0.5–1.3 mg/dL). Additionally, a reduced level of glomerular filtration rate (GFR) was observed at 39 mL/min/1.73 m2. Arterial blood gas revealed respiratory and lactic acidosis with pH: 7.18 (7.35–7.45), pCO2: 68 mmHg (32–48 mmHg), pO2: 56 mmHg (83–108 mmHg), and lactate: 3.15 mmol/L (0–2 mmol/L). The remaining results of the urine and laboratory analyses were found to be within the normal range. Green-coloured urine was observed passing through the Foley catheter, as depicted in Figure 1. Since the patient had no history of HF with reduced ejection fraction, the patient was hospitalized in the coronary care unit for acute decompensated HF caused by possible pacemaker-induced cardiomyopathy and green discoloration of the urine. At follow-up, the probable cause of the green discoloration of the urine was investigated. The patient had a normal serum level of total bilirubin, showed no indication of a Pseudomonas infection and was taking no medication that can make green urine. As the medical history was being carefully examined, 1 h following the dual chamber pacemaker implantation, a rapid endotracheal entubation was performed at another hospital while the patient was under sedation with propofol, and a dosage of 100 mg (one vial) of MB was administered as a treatment for methaemoglobinaemia, which was caused by prilocaine hydrochloride. The patient stated that the green urine continued for 7 days. Hence, a diagnosis of MB and propofol-induced green-hued urine was made. Despite the administration of 40 mg of furosemide diuretic therapy for the purpose of alleviating congestion, the resulting diuresis was found to be ineffective, as evidenced by a spot urine Na+ level of 16 mEq/L at 2 h. For diuretic resistance, the furosemide dose was doubled, and indapamide 2.5 mg was added as a diuretic treatment. Following a period of 2 days, the administration of combined diuretic therapy (CDT) involving furosemide and indapamide was observed to yield superior decongestion outcomes while concurrently improving both renal and liver function. The patient’s GFR exhibited a gradual increase, while the levels of AST and ALT showed a gradual decrease following the administration of CDT and conventional medical therapy for HF. Additionally, the patient’s urine discoloration changed from a colour of grass-green to light green and subsequently to yellow (Figure 1). The patient’s urine colour completely returned to normal after 12 days of treatment. The patient was sent home with conventional medical treatment for HF. According to the response of guideline-directed medical therapy for HF, we planned to decide whether the patient should undergo cardiac resynchronization therapy upgrade in the future for newly diagnosed heart failure with reduced ejection fraction.
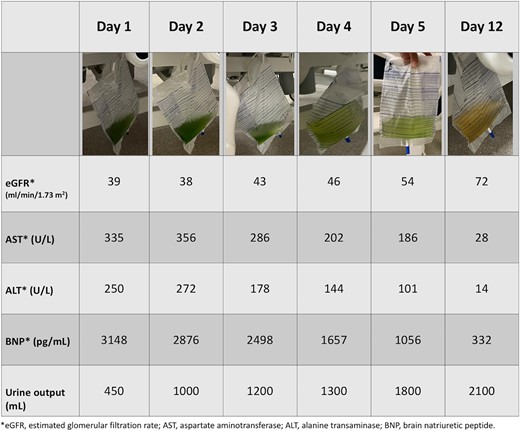
The greenish urine returns to normal colour with the improvement of daily urine output, brain natriuretic peptide, renal function, and liver function.
Discussion
Drugs such as propofol and MB have been found to be associated with the appearance of greenish urine, which is considered a benign side effect of these medications.5,6 Previous reports showed that the appearance of green urine typically resolved within a period of 2 h to 2 days following the cessation of propofol infusion and MB administration.5,7,8 Indeed, there has been no mentioning that it lasts more than 64 h in the literature.8 Of interest, it took 12 days for the urine colour to completely return to normal in our patient presenting with acutely decompensated HF resulting from pacemaker-induced cardiomyopathy.
Propofol is an intravenous sedative-hypnotic agent whose pharmacokinetic profile is characterized by a rapid and extensive distribution from blood into well-perfused tissues such as the brain and a rapid elimination from blood.4,9 Propofol is mainly metabolized by the liver. The majority of propofol is conjugated to glucuronides, and ∼30% of propofol is hydroxylated in the liver.9 The urinary excretion of the parent compound and its metabolites within a span of 5 days was found to be <1%.9,10 The presence of phenolic metabolites leads to the manifestation of a greenish hue in the urine.11
Methylene blue has been identified as a potential aetiological factor for the presence of greenish urine, but green urine is not commonly observed in MB-treated patients with normal renal function. Although the mechanisms underlying the observed long-term trend of green urine output are currently a matter of speculation, prolonged greenish discoloration of the urine in patients with HF may be attributed to renal and liver hypoperfusion.12 One potential aetiology of green urine is MB, which can lead to reduced cardiac output, renal perfusion, and mesenteric blood flow at elevated dosages. The negative impacts of MB depend on the dosage and typically manifest upon exceeding a dose of 2 mg/kg.13 The administered dose of MB in the patient was calculated to be 2.5 mg/kg. The administration of a toxic dose may result in impairment of cardiac function, followed by decreased hepatic and renal perfusion. The reduction in propofol metabolism in the liver is concomitant with hepatic hypoperfusion.9 The kidneys play a major role in propofol metabolism in such cases. Kidneys contribute approximately one-third of the total body clearance of propofol.10 Phenolic metabolites formed during renal metabolism may cause green urine conversion, whereas a reduction in renal perfusion can also be a contributing factor to the persistence of green urine. Renal hypoperfusion could potentially lead to a reduction in the GFR, thereby causing a prolonged excretion of propofol metabolites through the kidneys.
Conclusion
The significance of our case lies in its demonstration of an infrequent yet benign phenomenon called green discoloration of the urine resulting from the concurrent administration of MB and propofol in patients with acute decompensated HF due to pacemaker-induced cardiomyopathy. This prolonged benign phenomenon may indicate multiorgan dysfunction leading to reduced drug metabolism and excretion in patients with acute decompensated heart failure. Additionally, the daily change in urine colour may also serve as an indicator of improvement in renal and hepatic dysfunction. Therefore, it may help us optimize medical treatment in terms of HF.
Lead author biography
 I graduated from the Ege University Faculty of Medicine as a medical doctor in 2012. I became a cardiology specialist at the Dokuz Eylül University Faculty of Medicine, Department of Cardiology in 2017. Since 2017, I have been working as an assistant professor at the Karabük University Faculty of Medicine, Department of Cardiology. I was elected as a Member of the HFA on 29 December 2022. My special interest is heart failure and cardiovascular imaging.
I graduated from the Ege University Faculty of Medicine as a medical doctor in 2012. I became a cardiology specialist at the Dokuz Eylül University Faculty of Medicine, Department of Cardiology in 2017. Since 2017, I have been working as an assistant professor at the Karabük University Faculty of Medicine, Department of Cardiology. I was elected as a Member of the HFA on 29 December 2022. My special interest is heart failure and cardiovascular imaging.
Consent: The authors confirm that written consent for submission and publication of this case report including one image and associated text has been obtained from the patient.
Funding: The funder of the case report had no role in case report design, data collection, data interpretation, and writing of the report.
Data availability
The data underlying this article are available in the article and its online supplementary material.
References
Author notes
Conflict of interest: None declared.





Comments