-
PDF
- Split View
-
Views
-
Cite
Cite
Simon Sjuls, Ulf Jensen, Karin Littmann, Annette Bruchfeld, Jonas Brinck, Effective cholesterol lowering after myocardial infarction in patients with nephrotic syndrome may require a multi-pharmacological approach: a case report, European Heart Journal - Case Reports, Volume 5, Issue 5, May 2021, ytab151, https://doi.org/10.1093/ehjcr/ytab151
Close - Share Icon Share
Abstract
Nephrotic syndrome causes severe hypercholesterolaemia due to increased production and altered clearance of lipoproteins from the liver. It is challenging for patients with nephrotic syndrome and coronary heart disease to meet LDL-cholesterol (LDL-C) goals for secondary prevention with conventional lipid-lowering therapy.
We present a man with nephrotic syndrome caused by focal segmental glomerular sclerosis (FSGS) and hypercholesterolaemia. He presented at the emergency room (ER) with an ST-elevation myocardial infarction at the age of 26. On follow-up, the patient had persistent hypercholesterolaemia [LDL-C 3.9 mmol/L and lipoprotein(a) 308 nmol/L] despite a combination of lipid-lowering therapy with atorvastatin 80 mg/day and ezetimibe 10 mg/day. Addition of the proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitory antibody evolocumab 140 mg bi-monthly did not improve cholesterol levels. However, after addition of the sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin 10 mg/day on top of other anti-proteinuric treatments, the patient’s proteinuria was reduced and a dramatic drop in LDL-C level by 3.2–0.6 mmol/L (−81%) was observed when evolocumab was re-introduced.
We show that target LDL-C levels were obtained in this patient with therapy-resistant FSGS and hypercholesterolaemia following multi-pharmacological treatment with SGLT2 and PCSK9 inhibitors on top of conventional lipid-lowering therapy. The SGLT2-inhibitor reduced proteinuria and, speculatively, also reduced urinary loss of PCSK9-antibody. Therefore, in patients with nephrotic syndrome and cardiovascular disease novel therapeutic options to manage proteinuria could be considered to improve the efficacy of the lipid-lowering therapy, especially when the protein-based PCSK9 inhibitors are used.
Nephrosis may induce therapy-resistant hypercholesterolaemia that requires combination therapy with several lipid-lowering medications.
Cholesterol lowering with proprotein convertase subtilisin/kexin type 9 (PCSK9) antibodies may be less effective in patients with nephrosis due to urinary leakage.
Sodium-glucose cotransporter 2-inhibitors as add on to conventional anti-proteinuric treatments can reduce nephrosis and could be a treatment option to potentiate the effect of biological treatment such as PCSK9 antibodies.
Primary specialties involved other than cardiology
Nephrology and endocrinology.
Introduction
Patients with nephrotic syndrome present with proteinuria >3.5 g/day, hypoalbuminemia <36 g/L, hyperlipidaemia, and peripheral oedema.1 In nephrotic syndrome, loss of albumin and antithrombotic factors in the urine induces a counterbalancing hepatic hyperproduction of procoagulant factors, resulting in a prothrombotic milieu.2 Nephrotic patients also have an increased hepatic overproduction of apolipoprotein B-containing lipoproteins such as LDL and lipoprotein(a) [Lp(a)] resulting in high levels of plasma cholesterol that may be difficult to control with conventional lipid-lowering therapies.1 Reduced degradation of LDL-receptors due to overexpression of proprotein convertase subtilisin/kexin type 9 (PCSK9) contributes further to the hyperlipidaemia in patients with nephrotic syndrome. PCSK9-antibodies has proved to be an effective lipid-lowering treatment in patients with nephrotic syndrome.3
Sodium-glucose cotransporter 2 (SGLT2) inhibitors are an emerging treatment option for both diabetes and heart failure and have also proven to improve renal outcomes by reduction of hyperfiltration, tubular growth, kidney inflammation, and albuminuria.4 Recent data from the DAPA-CKD trial, dapagliflozin was shown to reduce risk of kidney failure and cardiovascular death in both diabetic and non-diabetic patients with chronic kidney disease.5
Timeline
| Date . | Medical information, treatment, or investigation . |
|---|---|
| 1990 | Patient born |
| 2014 | Patient diagnosed with focal segmental glomerular sclerosis at the age of 23. Starts treatment with atorvastatin 20 mg/day which was increased to 40 mg/day after 9 months |
| October 2016 | Patient has an ST-elevation myocardial infarction due to a thrombus in the mid-part of the left anterior descending artery Cholesterol-lowering treatment is intensified to atorvastatin 80 mg/day and ezetimibe 10 mg/day the following months |
| 2017 | Patient receives evolocumab 140 mg bi-monthly during two periods on top of current treatment but with limited effect |
| January 2018 | Patient starts treatment with empagliflozin 10 mg/day in attempt to reduce proteinuria. A reduction in proteinuria and an increased plasma albumin is seen |
| May 2018 | Evolocumab 140 mg bi-monthly is re-introduced with marked reduction of plasma LDL-cholesterol and lipoprotein(a) |
| December 2018 | End of follow-up due to patient moving to another region |
| Date . | Medical information, treatment, or investigation . |
|---|---|
| 1990 | Patient born |
| 2014 | Patient diagnosed with focal segmental glomerular sclerosis at the age of 23. Starts treatment with atorvastatin 20 mg/day which was increased to 40 mg/day after 9 months |
| October 2016 | Patient has an ST-elevation myocardial infarction due to a thrombus in the mid-part of the left anterior descending artery Cholesterol-lowering treatment is intensified to atorvastatin 80 mg/day and ezetimibe 10 mg/day the following months |
| 2017 | Patient receives evolocumab 140 mg bi-monthly during two periods on top of current treatment but with limited effect |
| January 2018 | Patient starts treatment with empagliflozin 10 mg/day in attempt to reduce proteinuria. A reduction in proteinuria and an increased plasma albumin is seen |
| May 2018 | Evolocumab 140 mg bi-monthly is re-introduced with marked reduction of plasma LDL-cholesterol and lipoprotein(a) |
| December 2018 | End of follow-up due to patient moving to another region |
| Date . | Medical information, treatment, or investigation . |
|---|---|
| 1990 | Patient born |
| 2014 | Patient diagnosed with focal segmental glomerular sclerosis at the age of 23. Starts treatment with atorvastatin 20 mg/day which was increased to 40 mg/day after 9 months |
| October 2016 | Patient has an ST-elevation myocardial infarction due to a thrombus in the mid-part of the left anterior descending artery Cholesterol-lowering treatment is intensified to atorvastatin 80 mg/day and ezetimibe 10 mg/day the following months |
| 2017 | Patient receives evolocumab 140 mg bi-monthly during two periods on top of current treatment but with limited effect |
| January 2018 | Patient starts treatment with empagliflozin 10 mg/day in attempt to reduce proteinuria. A reduction in proteinuria and an increased plasma albumin is seen |
| May 2018 | Evolocumab 140 mg bi-monthly is re-introduced with marked reduction of plasma LDL-cholesterol and lipoprotein(a) |
| December 2018 | End of follow-up due to patient moving to another region |
| Date . | Medical information, treatment, or investigation . |
|---|---|
| 1990 | Patient born |
| 2014 | Patient diagnosed with focal segmental glomerular sclerosis at the age of 23. Starts treatment with atorvastatin 20 mg/day which was increased to 40 mg/day after 9 months |
| October 2016 | Patient has an ST-elevation myocardial infarction due to a thrombus in the mid-part of the left anterior descending artery Cholesterol-lowering treatment is intensified to atorvastatin 80 mg/day and ezetimibe 10 mg/day the following months |
| 2017 | Patient receives evolocumab 140 mg bi-monthly during two periods on top of current treatment but with limited effect |
| January 2018 | Patient starts treatment with empagliflozin 10 mg/day in attempt to reduce proteinuria. A reduction in proteinuria and an increased plasma albumin is seen |
| May 2018 | Evolocumab 140 mg bi-monthly is re-introduced with marked reduction of plasma LDL-cholesterol and lipoprotein(a) |
| December 2018 | End of follow-up due to patient moving to another region |
Case presentation
The patient is a man born in 1990 who was diagnosed with primary focal segmental glomerular sclerosis (FSGS) in 2014 at 23 years of age. At diagnosis, the patient had experienced leg oedema and foamy urine for 1 week and physical examination showed pitting oedema and elevated blood pressure, 147/88 mmHg. Urine and blood samples showed an albumin to creatinine ratio of 510 mg/mmol (ref. <5.0 mg/mmol), plasma albumin 17.7 g/L (ref. 36–48 g/L), triglycerides 0.65 mmol/L (ref. 0.45–2.6 mmol/L), total cholesterol 8.8 mmol/L (ref. 3.3–6.9 mmol/L), HDL-cholesterol (HDL-C) 2.0 mmol/L (ref. 0.8–2.1 mmol/L), and LDL-cholesterol (LDL-C) 6.5 mmol/L (ref. 1.2–4.3 mmol/L) (Figure 1A). Lipoprotein(a) was not measured at this point. The FSGS diagnosis was determined after investigation with kidney biopsy and histological evaluation including electron microscopy and treatment was initiated with prednisolone, enalapril, loop-diuretics, atorvastatin, and anti-coagulation with dalteparin. Immunosuppressants (rituximab and later tacrolimus) were commenced on several occasions over the following years without significant effects on proteinuria or disease progression.

Blood lipids (A) and kidney function (B) over time. (A) Lipid-lowering therapies over time and changes in low-density lipoprotein-cholesterol (black) and lipoprotein(a) (red). (B) Kidney function over time measured in estimated glomerular filtration rate (black), urinary albumin to creatinine ratio (red), and plasma albumin (green). A40/80, atorvastatin 40/80 mg/day; eGFR, estimated glomerular filtration rate; Emp10, empagliflozin 10 mg/day; Ev140, evolocumab 140 mg/day; EZ10, ezetimibe 10 mg/day; LDL-C, LDL-cholesterol; STEMI, ST-elevation myocardial infarction.
In 2016, the patient was referred to the ER from a primary care facility due to onset of breathing-correlated chest pain and numbness in both arms following physical exercise the evening before. Electrocardiogram (ECG) showed ST-elevations in the leads V1–V4 (Figure 2A) and a bedside echocardiogram was performed which showed an ejection fraction of 45–50% and mild hypokinesia of the apical region. The symptoms and ECG as well as echocardiography were initially interpreted as a myocarditis and he was planned for ECG monitoring in a cardiac ward. Upon receiving the elevated troponin-T (972 ng/L, ref. <15 ng/L) the ER physician and the senior cardiology consultant decided to perform an acute coronary angiography on the suspicion on of acute coronary syndrome. The patient underwent percutaneous coronary intervention about two and a half hours after admission to the ER where a large thrombus in the mid-left anterior descending artery, as well as distal thrombus embolization, was identified (Figure 2B and Video 1A) and managed with thrombectomy and local intracoronary thrombolysis.
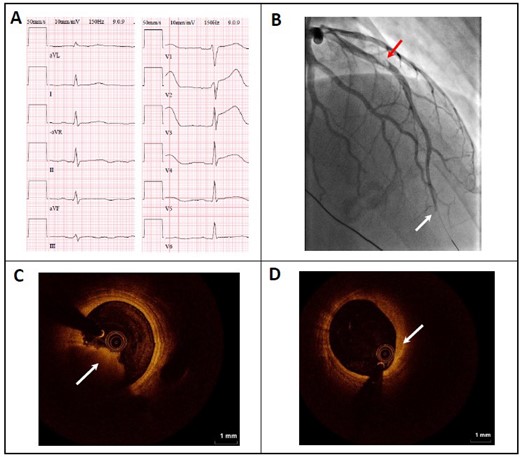
Electrocardiogram, angiography, and optical coherence tomography images before intervention. (A) Twelve-lead electrocardiography in ER showing ST-elevations in leads V1–V4 compatible with anteroseptal ST-segment elevation myocardial infarction. (B) Coronary angiography in right anterior oblique view with red arrow indicating partial occlusion in mid-left anterior descending artery and white arrow indicating total occlusion in the distal part of left anterior descending artery. Intracoronary optical coherence tomography imaging during second coronary intervention with arrows indicating red thrombus (C) and fibroatheroma (D) in left anterior descending artery.
Coronary angiography and optical coherence tomography videos before intervention. (A) Coronary angiography showing partial occlusion in mid-left anterior descending artery and total occlusions in distal part of left anterior descending artery. (B) Intracoronary optical coherence tomography imaging during second coronary intervention showing thrombus in mid-left anterior descending artery and fibroatheromas.
The patient admitted that he had poor compliance to medical treatment for nephrotic syndrome, including dalteparin injections, which partly explained the state of hypercoagulability, hypoalbuminemia (plasma albumin 7.1 g/L), and hypercholesterolaemia (triglycerides 3.3 mmol/L, total cholesterol 15.9 mmol/L, and LDL-C 13.2 mmol/L; Figure 1). The second coronary angiography 2 days after admission showed that the mural thrombus had not dissolved completely and optical coherence tomography (OCT; Figure 2C and D and Video 1B) showed fibroatheromas and signs of plaque at the segment for the thrombus, which was managed by insertion of a drug-eluting stent. It was concluded that the patient’s ST-elevation myocardial infarction (STEMI) had been caused by a state of hypercoagulability generating a thrombus and an atherosclerotic process, both which were secondary to the nephrotic syndrome. In addition to dalteparin injections, acetylsalicylic acid and ticagrelor were prescribed as secondary prevention. An echocardiogram was performed which showed an ejection fraction of 35% and moderately impaired function of the left ventricle 3 days after the STEMI. Follow-up echocardiogram 1 month after the STEMI showed an ejection fraction of 50% and mild left ventricular impairment. Warfarin replaced dalteparin 6 months after the STEMI in accordance with recommendations for long-term thrombosis prophylaxis in nephrotic patients.6 At the same time, acetylsalicylic acid and ticagrelor were replaced with clopidogrel. After the STEMI the patient’s lipid-lowering therapy was intensified to atorvastatin 80 mg/day and addition of ezetimibe 10 mg/day in December 2016 (Figure 1A). In January 2017, the patient had a lipid profile with triglycerides 1.9 mmol/L, total cholesterol 6.6 mmol/L, HDL-C 1.8 mmol/L, LDL-C 3.9 mmol/L, and Lp(a) 308 nmol/L. To improve the LDL-C level further, treatment with the PCSK9 inhibitory antibody evolocumab 140 mg was initiated and evaluated after 2 weeks with only minor effect on LDL-C (3.3 mmol/L; −16%) and an increased Lp(a) (321 nmol/L; +12%). A second attempt with evolocumab was initiated in August 2017 [LDL-C 5.1 mmol/L and Lp(a) 208 nmol/L] for 2 months after which LDL-C was reduced significantly (LDL-C 2.6 mmol/L; −50%), but again an increase in Lp(a) was observed (254 nmol/L; +22%). At this time point, evolocumab was stopped temporarily because of unclear regulation concerning indication for subsidy of PCSK9-inhibition treatment by the government agency (Dental and Pharmaceutical Benefits Agency).
In January 2018, therapy with SGLT2-inhibitor empagliflozin was introduced in attempt to improve nephrosis, increase plasma albumin, and, if possible, stabilize estimated glomerular filtration rate (eGFR) decline. At initiation of empagliflozin the patient was treated with both angiotensin-converting enzyme (ACE)-inhibitor (enalapril 20 mg/day) and mineralocorticoid receptor antagonist (spironolactone 25 mg/day) and had an eGFR of 30 mL/min/1.73 m2 and plasma albumin of ∼12 g/L (Figure 1B). The patient had a plasma lipid profile with triglycerides 0.52 mmol/L, total cholesterol 6.1 mmol/L, HDL-C 2.4 mmol/L, LDL-C 3.6 mmol/L, and Lp(a) 258 nmol/L (Figure 1A). After 1 month of treatment the patient reported a clear improvement in leg oedema at the same time as the proteinuria decreased from 5100 to 2000 mg/L and the patient could also reduce the diuretics dose. After 9 months of empagliflozin therapy the urine-albumin/creatinine ratio decreased from 984 to 618 mg/mmol (−37%, Figure 1B). In addition, plasma albumin increased to 22 g/L (+47%; Figure 1B) after 10 months. A 30% reduction in LDL-C from 3.6 to 2.5 mmol/L and 19% reduction in Lp(a) from 258 to 209 nmol/L was observed 4 months after initiation of empagliflozin therapy. Treatment with evolocumab was initiated for the third time in May 2018 following the reduction of proteinuria. Both LDL-C and Lp(a) levels decreased further to 0.6 mmol/L (−76%) and 123 nmol/L (−41%), respectively, after 4 months with the combination therapy empagliflozin and evolocumab on top of conventional lipid-lowering therapy (Figure 1A). Estimated glomerular filtration rate decreased from 25 to 23 mL/min/1.73 m2 (−8%) during the first 4 months after initiation of evolocumab. The patient did not experience any adverse effects related to the medications during the follow-up. In December 2018, the patient moved to another region and monitoring was taken over by the local hospital.
Discussion
We show that severe hypercholesterolaemia in a patient with nephrotic syndrome was successfully treated with a multi-pharmacological approach. The recommended LDL-C treatment target for very high cardiovascular risk patients with history of myocardial infarction and coronary revascularization is <1.4 mmol/L according to the current ESC/EAS guidelines.7 Based on the findings during the coronary angiography and OCT we consider that the patient has established coronary heart disease and benefits from very intensive LDL-C lowering therapy. Very low LDL-C levels in the circulation does not seem to disturb important cholesterol-dependent functions such as steroid hormone production and enterohepatic bile acid circulation according to data from studies on human physiology and rare genetic diseases.8 The treating physicians were not alarmed by the LDL-C levels obtained in this patient and were comfortable to continue with the multi-pharmacological therapy leading to an LDL-C of 0.6 mmol/L.
The patient’s underlying therapy-resistant kidney disease (FSGS) led to a steady decline in kidney function. End-stage kidney disease would ultimately have contributed to reduced proteinuria and improved plasma albumin and blood lipids in this patient. However, the rapid and substantial effect observed on plasma albumin and LDL-C after treatment with SGLT2-inhibitor does not correspond to the small decline in eGFR during the same time period, indicating a specific mechanism of action other than reduced GFR.
The success in reaching recommended LDL-C target for this patient can be attributed to the multi-pharmacological approach with SGLT2 and PCSK9 inhibitors on top of conventional lipid-lowering therapy. The recognized protein-sparing effect of SGLT2 inhibitors9 could in this case (plasma albumin +41% after start of empagliflozin) contribute to increased oncotic pressure and thereby help to reduce hepatic LDL overproduction. Speculatively, SGLT2 inhibition could also assist in reducing urinary loss of the PCSK9 antibody. It has been previously reported that the serum half-life of monoclonal antibody drug rituximab is significantly reduced in patients with nephrotic syndrome partially due to urinary loss.10 Evolocumab and rituximab are similar in size, which could support the theory that urinary leakage of evolocumab might be significant in nephrotic patients. It should be noted that the patient received ACE-inhibition in full dose (enalapril 20 mg/day) during the full-time period and the treating physicians did not consider changing the dose at any time. A limitation of this study is that we did not measure the concentration of evolocumab antibody in plasma or in the urine.
Lipid-lowering by PCSK9-inhibition in patients with nephrotic syndrome has been reported previously11,12 but with less persistent nephrosis or varying success in reaching an LDL-C level below 1.4 mmol/L. In this case, although evolocumab had a lipid-lowering effect, it was the combination with SGLT2-inhibitor that made it possible to achieve the recommended LDL-C target and also a reduction of Lp(a) was observed. Lipoprotein(a) increased slightly during the first two treatment attempts with evolocumab which was unexpected. Previous studies have shown a class effect of PCSK9-inhibition on Lp(a) levels leading to a reduction of ∼20–27%.3 It is conceivable that the first two attempts with evolocumab were too short to evaluate the effect on Lp(a) due to Lp(a)’s relatively long plasma turnover time.13
In summary, in patients with nephrotic syndrome and cardiovascular disease a multi-pharmacological approach including reducing proteinuria should be considered to improve the efficacy of lipid-lowering therapy, especially when the protein-based PCSK9 inhibitors are considered.
Patient perspective
This young man with nephrotic syndrome and a myocardial infarction caused by a coronary thrombus highlights the importance adherence to prescribed drugs. The patient had poor compliance to prescribed medications, including dalteparin due to fear of self-injections, which ultimately contributed to the STEMI. After the STEMI, the patient became aware of the seriousness of his medical condition and was thereafter, to the best of our knowledge, adherent to the medical treatment. Management of the extreme hypercholesterolaemia often seen in nephrotic syndrome requires a multi-pharmacological approach. This case underscores the importance of an informed patient in order to achieve a successful treatment.
Lead author biography
Simon Sjuls was born in Aland Islands, Finland, in 1993. He is a fifth-year medical student at the Karolinska Institute, Sweden. He is engaged in research about hereditary dyslipidaemias including lipoprotein(a) and cardiovascular disease at the Department of Medicine, Karolinska Institute and Karolinska University Hospital, Stockholm.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: JB has received consultancy fees and an investigator-initiated study grant from Amgen. AB reports grants and personal fees from Astra Zeneca, personal fees from ChemoCentryx, personal fees from Merck/MSD, personal fees from Abbvie outside the submitted work.
Funding: None declared.
References
- atorvastatin
- myocardial infarction
- nephrotic syndrome
- proteinuria
- st segment elevation myocardial infarction
- ldl cholesterol lipoproteins
- hypercholesterolemia
- lipoproteins
- cholesterol
- glucose
- follow-up
- focal glomerulosclerosis
- urinary tract
- antibodies
- pharmacology
- sodium
- lipid-lowering therapy
- ezetimibe
- pcsk9 gene
- sodium-glucose transporter 2 inhibitors
- evolocumab
- empagliflozin
- pcsk9 inhibitors





Comments