-
PDF
- Split View
-
Views
-
Cite
Cite
Shana Tehrani, Sudhir Rathore, Vinod Achan, Changing paradigm for treatment of heavily calcified coronary artery disease. A complementary role of rotational atherectomy and intravascular lithotripsy with shockwave balloon: a case report, European Heart Journal - Case Reports, Volume 5, Issue 1, January 2021, ytaa456, https://doi.org/10.1093/ehjcr/ytaa456
Close - Share Icon Share
Abstract
Management of heavily calcified coronary arteries is still a major challenge in interventional cardiology. Inadequate stent expansion in calcific lesions is the single most important predictor of stent thrombosis and in-stent restenosis. Rotational atherectomy (RA) is an important tool to modify the calcium burden but is associated with limitations and requires specific skills. Intravascular lithotripsy (IVL) is a novel technique to treat calcified stenotic lesions and has been proposed as an alternative to RA with promising results.
We report a case of a patient with severely calcified right coronary artery stenosis successfully treated with combination of RA and IVL.
In this case, we demonstrate that the RA and IVL are complementary strategies, not sufficient on their own and not alternative to each other.
Learning points
Rotational atherectomy and intravascular lithotripsy are not mutually exclusive but can be complementary strategies.
Shockwave intravascular lithotripsy is a major development but not a substitute for rotational atherectomy in the treatment of calcified coronary lesions.
Introduction
Calcified coronary lesions increase the complexity of percutaneous coronary intervention (PCI). They are associated with stent under-expansion and subsequent stent thrombosis, restenosis and hence the adverse outcomes.1 Therefore, optimal preparation of the calcific lesions prior to stent deployment is crucial. Among the available techniques to disrupt the underlying calcium, rotational atherectomy (RA) is an effective tool but with limitations and potential complications. Intravascular lithotripsy (IVL) (Shockwave Medical Inc.) is a new technique for calcium modification with promising results that has been proposed as an alternative to RA.2–6
We hereby present a case of a severely calcified right coronary artery (RCA) successfully treated with combination of RA and IVL and demonstrates that RA and IVL are complementary strategies and not alternative to each other.
Timeline
Case presentation
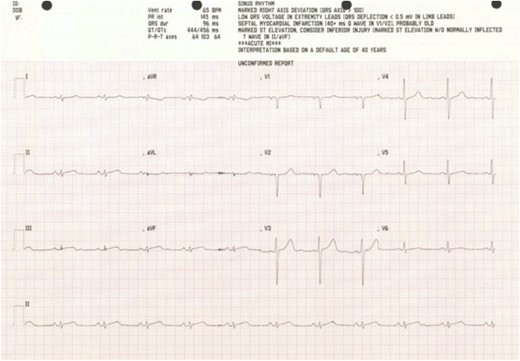
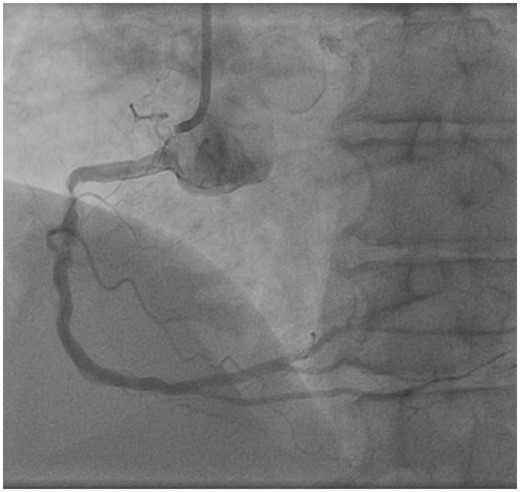
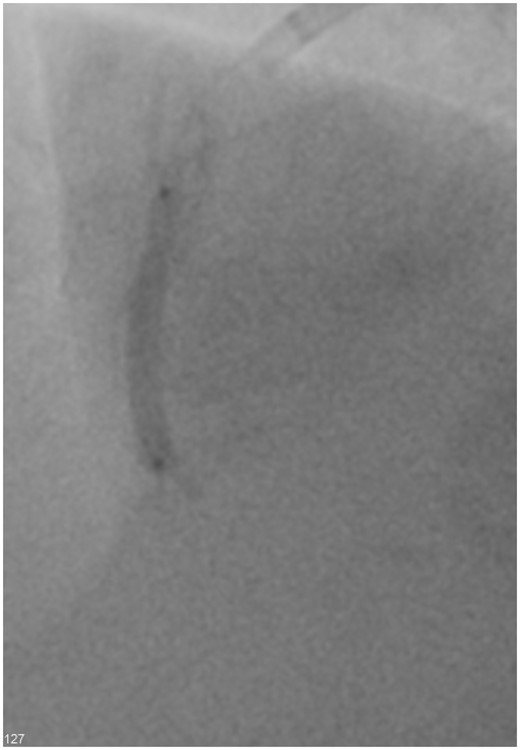
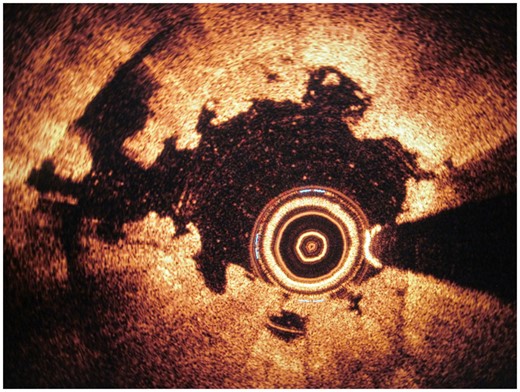
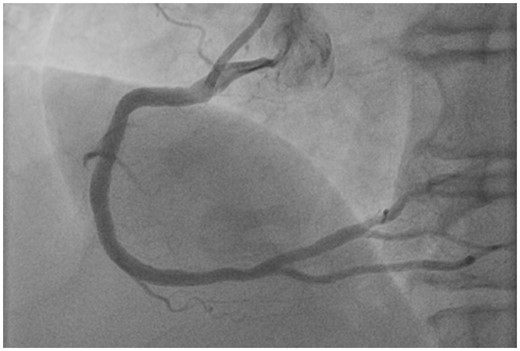
A 62-year-old man with background of type 2 diabetes mellitus, peripheral vascular disease, and hypertension developed inferior ST-segment elevation during induction for femoral popliteal bypass surgery (Figure 1). The operation was abandoned and he was urgently transferred to the cardiac catheterization laboratory. Coronary angiography was performed via right radial access route using 5 Fr JR4 and JL3.5 diagnostic catheters. Coronary angiography showed critical heavily calcified stenosis in the RCA (Figure 2, Video 1) and long segment of moderate disease in the left anterior descending artery (LAD). The left main and circumflex arteries showed non-obstructive disease. Percutaneous coronary intervention to the RCA was performed using a 6 Fr AL1 guide catheter and PT2 moderate support guidewire. It was not possible to fully inflate 2.5 mm semi-compliant and non-complaint balloons (NCB) (Figure 3). Therefore, decision was made to proceed to IVL with Shockwave Balloon. However, passing the optical coherence tomography catheter or 2.5 mm IVL balloon was not possible. Subsequently, RA with 1.5 and 1.75 mm burrs was carried out followed by NCB inflation (Figure 4), which facilitated passage of the 2.5 × 12 mm IVL balloon. Sequential 8 cycles of 10 pulses each of lithotripsy were delivered. Optical coherence tomography post-IVL confirmed micro-fractures in the calcium (Figure 5). Following this, 3.0 × 12 mm and 3.5 × 20 mm NCBs were used to further prepare the lesion. A Resolute Onyx 4.0 × 38 mm stent was positioned with the support of a Medtronic Telescope guide extension catheter. The stent was post-dilated using a 4.0 × 20 mm NCB to high pressure. Final angiography demonstrated excellent stent expansion and apposition (Figure 6, Video 2). The patient remained haemodynamically stable throughout the procedure and did not require any support. Echocardiography post-PCI showed normal left ventricular systolic function without regional wall motion abnormalities. Staged pressure wire assessment of the LAD showed FFR level of 0.8, therefore, PCI was not performed. The patient has been followed up in the outpatient clinic and has made a good progress.
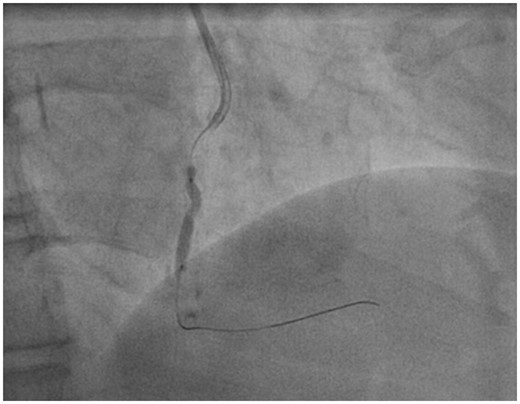
Non-compliant balloon post-rotational atherectomy and pre-intravascular lithotripsy.
Discussion
Treatment of severely calcified coronary arteries is a challenge in interventional cardiology. Sub-optimal preparation of calcific vessels results in stent under-expansion, struts malapposition, damage to the polymer, and subsequent stent thrombosis and restenosis.7,8 Although use of RA has significantly improved success rates in tackling heavily calcified lesions, this procedure requires specific skills and is sometimes associated with potentially serious complications including slow flow, no-reflow, vessel perforation, and dissection.2 Furthermore, effectiveness of RA depends on the luminal area and burr size with predictable luminal gain in the presence of circumferential calcifications and when the luminal area is smaller than the burr size.7 Calcium modification is less predictable when the burr used is smaller than the luminal area.2,7
Intravascular lithotripsy (Shockwave Medical Inc.) is a recently introduced balloon-based technique, established on the principles of renal stone treatment. Intravascular lithotripsy uses circumferential sonic pressure waves to disrupt intimal and medial calcium, or in another terms to fracture both superficial and deep wall calcification, prior to low-pressure balloon expansion. It is safe, user friendly, and is not associated with significant risks.4,5,9,10 The balloons are largely deliverable and compatible with 6 Fr Guidecatheters. Due to the absence of interaction with surrounding soft tissue, there is minimal vessel wall injury.7 Intravascular lithotripsy delivers immediate plaque modification by creating micro-fractures in the calcium deposits.6
The feasibility of IVL to modify vascular compliance in calcific coronary arteries was first demonstrated in Disrupt CAD I study.4 Its safety has been demonstrated in Disrupt CAD II study.10
Introduction of IVL has indeed transformed calcium modification. Unlike RA, it does not require specific training and is not associated with complications. It is not biased by the guidewire, therefore, fractures the calcified plaques circumferentially.10 Prospective studies and real-world experiences have shown high effectiveness of IVL in crossing the lesions and facilitating stent delivery.5,10
In this case, however, we demonstrated that this single technology is not always feasible in the presence of large calcifications.
In our case, the severely calcific lesion was not dilatable with NCB and IVL could not cross the lesion. Rotational atherectomy allowed adequate lesion preparation and delivery of IVL balloon. Rotational atherectomy is more efficient in modification of superficial calcium and IVL Shockwave balloon treats both superficial and deeper calcium. Therefore, occasionally ‘Rota- Shock’ or ‘Rota-tripsy’ might be required to modify the calcium burden sufficiently to facilitate stent delivery and expansion.
Severe calcific lesion in RCA.
Final image.
Conclusion
This case has highlighted the challenges associated with treating heavily calcified coronary arteries and the steps taken to overcome these as recommended in the calcium algorithm. Rotational atherectomy and IVL are not mutually exclusive but can be complementary strategies. Shockwave IVL is a major development but not a substitute for rotational atherectomy in the treatment of calcified coronary lesions.
Lead author biography
Shana Tehrani fellow in Interventional Cardiology, UK.
Acknowledgements
We are grateful to the cath lab staff who assisted us in the management of this patient.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Funding: none declared.






Comments