-
PDF
- Split View
-
Views
-
Cite
Cite
Yerramareddy Vijayachandra, Shalini Mani, Futuristic robotic percutaneous coronary intervention with innovative physiology optimization: a case report, European Heart Journal - Case Reports, Volume 6, Issue 7, July 2022, ytac276, https://doi.org/10.1093/ehjcr/ytac276
Close - Share Icon Share
Abstract
Robotic percutaneous coronary intervention (R-PCI) is being preferred over traditional PCI procedures owing to reduced radiation exposure to the personnel performing this technique. However, there are some challenges in using pressure wires in R-PCI.
This is the first article reporting the usage of pressure wire navigation in R-PCI. We have discussed a case of severe mid-right coronary artery disease, managed with physiology-assisted R-PCI. Software features of R-PCI such as Rotate-On-Retract were effectively used to negotiate Pressure Wire™ X across the tortuous artery. Stenting was successfully carried out with Pressure Wire™ X/R-PCI without any adverse events during or after the procedure.
Pressure Wire™ X was used with certain modifications to negotiate tortuous arteries. The R-PCI procedure was carried out successfully without any adverse events during or after the procedure.
Robotic percutaneous coronary intervention (R-PCI) has an ever-growing evidence base to support its use and has been successfully utilized in treating highly complex coronary lesions.
To recognize the innovative usage of pressure wire in R-PCI.
To recognize the utilization of physiology guidance and imaging optimization in R-PCI.
Introduction
Robotic percutaneous coronary intervention (R-PCI) is increasingly gaining acceptance owing to the reduced radiation exposure to the personnel (Figure 1A).1 Increasing innovation in this field has also contributed to the ease of wiring and precision in stenting. ‘Optimal PCI’ is gaining importance recently. Optimization by intravascular imaging with optical coherence tomography (OCT)2 and final physiology optimization with flow indices such as instantaneous wave-free ratio (iFR) with a final iFR of 0.95 has been shown to result in better procedural success and long-term outcomes.3,4 A state-of-the-art R-PCI should ideally incorporate all these components. There are some challenges in using pressure wires in R-PCI which can be overcome with modifications in the technique. We present a case of state-of-the-art robotic Precision ‘Optimal PCI’ with flow optimization using Pressure Wire™ X and imaging optimization with OCT.
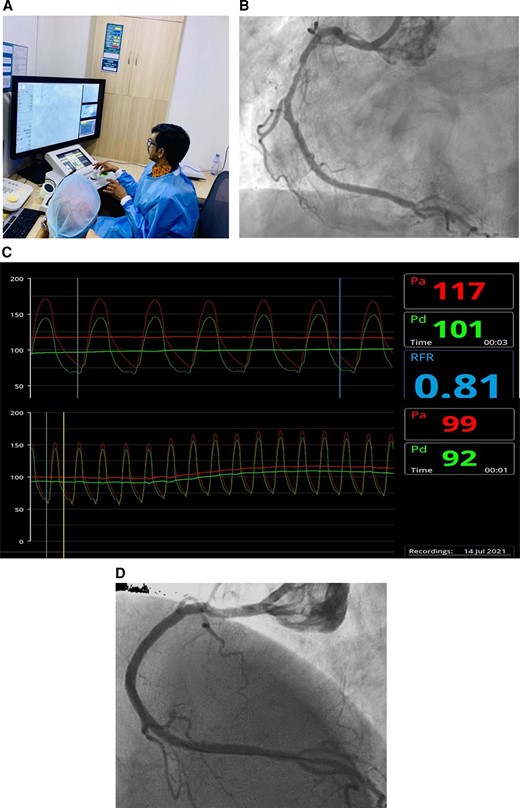
(A) The interventional cardiologist performing robotic percutaneous coronary intervention from the robotic console situated outside the radiation field. (B) Severe long-segment mid-right coronary artery disease, multiple side branches. (C) Resting Pd/Pa and baseline resting full-cycle ratio. (D) Final result.
Timeline
Case details
A 52-year-old woman with diabetes presented with chronic stable angina and a strongly positive treadmill test with normal left ventricular function. She underwent coronary angiography, which revealed the mild disease of the left system with severe long-segment mid-right coronary artery (RCA) disease (Figure 1B). She was taken up for a robotic Precision PCI of RCA with physiology and imaging optimization. This would enable precise stent positioning and improve the accuracy for better patient outcomes.
The RCA was a dominant vessel with an initial shepherd-crook and proximal tortuousities with multiple side branches in the mid-segment. The RCA was engaged with a JR 3.5 guide catheter, and a Pressure Wire™ X (Abbott Vascular, USA) was introduced into the guide catheter for physiology assessment and also for performing the PCI procedure (see Supplementary material online, Video S1). We used the Pressure Wire™ X system for assessing flow ratios (resting Pd/Pa) and resting full-cycle ratio (RFR) (Figure 1C) as it is the only wireless system and would be more suitable for use in R-PCI. The zeroing of the pressures was done keeping the Pressure Wire X flat on the table, the transmitter switched on, and the wire was then introduced into the guide catheter that was already secured to the robotic drive. Further advancement of the pressure wire was done robotically using the guidewire joystick (Figure 1 and see Supplementary material online, Video S2).
Once the pressure wire sensor was in the normal proximal RCA, the wireless transmitter was connected to the proximal end of the wire jutting out of the robotic drive cassette with the cath lab nurse supporting it with her hand (Figure 2 and see Supplementary material online, Video S2), making sure there was no lag in the wire, and then equalization was done. After equalization, the pressure wire was advanced robotically; the Rotate-on-Retract (ROR) feature facilitated easy negotiation of the pressure wire across the mid-RCA and placement of the wire in the distal vessel.

The resting Pd/Pa and RFR were measured and the wireless transmitter was disconnected (without putting the transmitter off) for carrying out further steps of the PCI procedure on the same wire. The resting Pd/Pa was 0.93 and the baseline RFR was 0.81, suggesting significant ischaemia.
A 2.5 × 15 mm balloon (NC Trek; Abbott Vascular, USA) was robotically advanced into the lesion and pre-dilatation was done at 12 atm. The same balloon was used to precisely measure the needed stent length, which measured as 32.5 mm. A 2.5 × 33 mm Xience Xpedition® drug-eluting stent (Abbott Vascular, USA) was then robotically advanced into position and deployed at 14 atm. The stent boost revealed a well-expanded stent while angiography revealed a well-deployed stent with the good angiographic results (Figure 1D and see Supplementary material online, Video S3).
After the stent balloon was removed, the pressure wire transmitter was reconnected to the end of the wire, with the cath lab nurse supporting it with her hand as before ensuring there was no lag in the wire. The post-stenting measurements were then recorded; Pd/Pa was 1.0 and RFR was 0.99. Since the initial equalization was done in the same way, and as the pressure wire transmitter was not switched off during the entire procedure, the elevated placement of the transmitter did not affect the accuracy of pressure measurement.
The OCT image was then acquired after manually loading the OCT Dragonfly Optis catheter to the desired position distal to the stent. The OCT run revealed a well-opposed, well-expanded stent (minimal stent expansion 89%; minimal stent area 4.89 mm2). There was no evidence of edge dissection, thrombus, tissue prolapse, or geographic miss (Figure 3A and B).
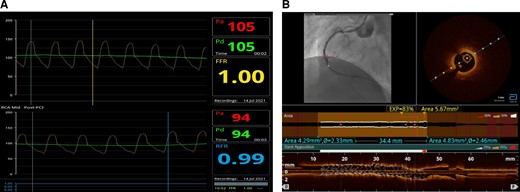
(A) Post-procedure Pd/Pa and resting full-cycle ratio. (B) Post-procedure optical coherence tomography.
Finally, the Pressure Wire X was robotically retracted to check for pressure drift and there was no pressure drift. This also reassured that the physiology assessment was not impacted by the modified steps performed to adapt it to R-PCI.
The procedure was successfully completed, and the patient was asymptomatic in the first-, third-, and sixth-month follow-up.
Discussion
Robotic-assisted PCI represents the next paradigm shift in contemporary PCI practice. It has the ability to enhance procedural accuracy for the patient while improving radiation safety and ergonomics for the operator. The radiation exposure to the patient with traditional PCI is considerably high and is associated with the risk of radiation-induced adverse effects such as cataracts.5 According to a recent study, a significant reduction in radiation exposure to the patients was reported with R-PCI compared with traditional PCI [Air kerma (mGy): 833 vs. 1235, respectively; P < 0.0005].6
Combining R-PCI with final imaging and physiology optimization as performed here has the potential to become the standard of practice in the future. The OCT catheter is not amenable for robotic advancement but can be manually advanced and OCT performed in the usual manner. However, there are some challenges to the use of pressure wire for physiology assessment in R-PCI. While the pressure wire can be advanced robotically, the maneuverability with a robotic joystick is a concern. Also, the guidewire projects out of the robotic drive cassette and cannot be placed flat on the catheterization table as in the usual non-R-PCI procedures. This poses practical difficulties in using this technology with R-PCI. We have shown the ease of navigation of pressure wire and also the modifications in technique to circumvent the problems without any errors in measurements. We utilized the wireless system of Pressure Wire X which is more suitable for use in R-PCI with simple, easily replicable modifications in technique. Resting full-cycle ratio, as measured with this system, has previously been validated with iFR.3 This ability to optimize the PCI with physiology can be of added importance in scenarios where OCT imaging optimization is not possible due to limitations with dye usage or other similar limitations. Robotic percutaneous coronary intervention with OCT imaging would help improve the outcomes for the patients and there is a need to educate patients to enable them to make an informed choice about opting for this approach.
Conclusion
Robotic Precision ‘Optimal PCI’ of RCA was carried out successfully without any adverse events during or after the procedure. We used Pressure Wire™ X for the R-PCI for physiology assessment and for carrying out the PCI procedure with certain modifications in the steps to suit R-PCI technology. While Pressure Wire™ X is perceived to be slightly more difficult to negotiate across multiple side branches, we demonstrated its easy negotiation using software features of R-PCI such as ROR. We manually loaded the OCT catheter at the end of the procedure and were able to achieve the imaging objective of Optimal PCI.
Lead author biography
 Dr. Y. Vijayachandra Reddy (Yerramareddy Vijayachandra), MD DM MRCP FACC FCSI FSCAI CCDS, is a Senior Consultant & Interventional Cardiologist at Apollo Main Hospitals, Chennai. He is well known in the field of Interventional Cardiology with extensive and versatile experience and range of professional work. He is a pioneer in transradial interventions and complex high-risk CHIP interventions including left-main, bifurcation and CTO PCIs. He is credited with pioneering work in acute MI interventions and his large body of PCI work in cardiogenic shock with unparalleled outcomes is well known. He is also versatile in coronary physiology and imaging, and facile with the gamut of PCI techniques involving Robotic PCI, Rotablation, IVL, Laser atherectomy etc.
Dr. Y. Vijayachandra Reddy (Yerramareddy Vijayachandra), MD DM MRCP FACC FCSI FSCAI CCDS, is a Senior Consultant & Interventional Cardiologist at Apollo Main Hospitals, Chennai. He is well known in the field of Interventional Cardiology with extensive and versatile experience and range of professional work. He is a pioneer in transradial interventions and complex high-risk CHIP interventions including left-main, bifurcation and CTO PCIs. He is credited with pioneering work in acute MI interventions and his large body of PCI work in cardiogenic shock with unparalleled outcomes is well known. He is also versatile in coronary physiology and imaging, and facile with the gamut of PCI techniques involving Robotic PCI, Rotablation, IVL, Laser atherectomy etc.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflicts of interest: None declared.
Funding: None declared.





Comments