-
PDF
- Split View
-
Views
-
Cite
Cite
Sorin Giusca, Andrej Schmidt, Grigorios Korosoglou, A case report of distal radial puncture in a patient with acute upper limb ischaemia: the last hope of the cardiologist?, European Heart Journal - Case Reports, Volume 6, Issue 7, July 2022, ytac215, https://doi.org/10.1093/ehjcr/ytac215
Close - Share Icon Share
Abstract
Patients with acute limb ischaemia (ALI) present with acute symptoms, requiring prompt diagnosis and expedited treatment to preserve the viability of the affected ischaemic tissue.
We present an 83-year-old female patient with upper ALI due to thrombotic occlusion of the left brachial artery. Concomitantly, the patient had a first diagnosis of atrial fibrillation and was not on treatment with oral anticoagulation. Transfemoral thrombectomy using a 6F Rotarex® catheter resulted in removal of the thrombus from the brachial artery. However, significant amounts of debris embolized distally, causing occlusion of both the radial and ulnar arteries. The debris was successfully removed after puncture of the distal radial artery and retrograde thrombus aspiration using a 5F Envoy catheter. This manoeuver led to flow restoration in both the radial and ulnar arteries and to complete resolution of ischaemic symptoms of the patient.
Interventionists may consider distal radial puncture not only as an access site for coronary angiography but also as an option for the endovascular management of ALI in cases of cardiac embolism, as described herein or in cases of thrombotic complications during routine catheterization and percutaneous coronary intervention. Herein, we describe the case of an 83-year-old patient, who presented with acute upper limb ischaemia. Due to embolization of thrombotic debris during Rotarex® catheter thrombectomy, flow further diminished in the ulnar and radial arteries. The last hope for successful interventional treatment was thrombectomy from distally after retrograde puncture of the distal radial artery. This unique manoeuver led to flow restoration and complete recovery of the patient without the need for open surgery.
To know the clinical presentations and risk factors associated with acute upper limb ischaemia.
To recognize clinical and imaging findings in acute upper limb ischaemia, including the diagnosis of atrial fibrillation by electrocardiography, use of Duplex sonography and angiography.
To recognize the role of the distal transradial access as a rescue access site for thrombus retrieval in case antegrade techniques fail or are not possible.
Introduction
Endovascular techniques for the treatment of peripheral artery disease (PAD) continuously developed during the last decades, currently emerging as the first choice of treatment, especially in elderly and frail patients with co-morbidities and high perioperative risk.1,2 Especially in acute limb ischaemia (ALI), which in most cases occurs due to thrombotic vessel occlusion, patients present with acute symptoms including ischaemic pain, paleness, pulselessness, and paraesthesia of the affected limb. Such patients require prompt diagnosis of the underlying thromboembolism and expedited reperfusion treatment to preserve the viability of the affected tissue.3 Atrial fibrillation is a condition mostly associated with ischaemic events of thrombotic nature.4 Traditionally, surgical thromboembolectomy was used for the treatment of acute upper limb ischaemia. However, minimal invasive techniques such as thrombus aspiration, mechanical thrombectomy, and ultrasound-assisted thrombolysis have emerged as valuable alternatives and are currently endorsed by current guidelines.3
Timeline
| Time . | Events . |
|---|---|
| Day 1 | |
| 14.00 | Patient presented in our emergency department with ischaemic symptoms |
| 14.05 | Clinical examination revealed upper limb ischaemia |
| 14.10 | Electrocardiography exhibited atrial fibrillation with a resting heart rate of 110 b.p.m. |
| 14.15 | Duplex sonography revealed thrombotic occlusion of the axillary and brachial arteries |
| 15.00 | Digital subtraction angiography performed confirming suspected diagnosis |
| 15.10 | Rotarex mechanical thrombectomy |
| 15.25 | Envoy catheter attempted from antegrade (not possible due to limited catheter length) |
| 15.45 | Puncture of the distal radial artery |
| 15.50 | 5F Envoy catheter aspiration from retrograde |
| 16.15 | Complete flow restoration in both the radial and ulnar arteries |
| Day 2 | Duplex sonography at the next day showing good flow profiles |
| Day 4 | Patient discharged |
| After 3 months | Patient remains uneventful without ischaemic symptoms or functional deficits |
| Time . | Events . |
|---|---|
| Day 1 | |
| 14.00 | Patient presented in our emergency department with ischaemic symptoms |
| 14.05 | Clinical examination revealed upper limb ischaemia |
| 14.10 | Electrocardiography exhibited atrial fibrillation with a resting heart rate of 110 b.p.m. |
| 14.15 | Duplex sonography revealed thrombotic occlusion of the axillary and brachial arteries |
| 15.00 | Digital subtraction angiography performed confirming suspected diagnosis |
| 15.10 | Rotarex mechanical thrombectomy |
| 15.25 | Envoy catheter attempted from antegrade (not possible due to limited catheter length) |
| 15.45 | Puncture of the distal radial artery |
| 15.50 | 5F Envoy catheter aspiration from retrograde |
| 16.15 | Complete flow restoration in both the radial and ulnar arteries |
| Day 2 | Duplex sonography at the next day showing good flow profiles |
| Day 4 | Patient discharged |
| After 3 months | Patient remains uneventful without ischaemic symptoms or functional deficits |
| Time . | Events . |
|---|---|
| Day 1 | |
| 14.00 | Patient presented in our emergency department with ischaemic symptoms |
| 14.05 | Clinical examination revealed upper limb ischaemia |
| 14.10 | Electrocardiography exhibited atrial fibrillation with a resting heart rate of 110 b.p.m. |
| 14.15 | Duplex sonography revealed thrombotic occlusion of the axillary and brachial arteries |
| 15.00 | Digital subtraction angiography performed confirming suspected diagnosis |
| 15.10 | Rotarex mechanical thrombectomy |
| 15.25 | Envoy catheter attempted from antegrade (not possible due to limited catheter length) |
| 15.45 | Puncture of the distal radial artery |
| 15.50 | 5F Envoy catheter aspiration from retrograde |
| 16.15 | Complete flow restoration in both the radial and ulnar arteries |
| Day 2 | Duplex sonography at the next day showing good flow profiles |
| Day 4 | Patient discharged |
| After 3 months | Patient remains uneventful without ischaemic symptoms or functional deficits |
| Time . | Events . |
|---|---|
| Day 1 | |
| 14.00 | Patient presented in our emergency department with ischaemic symptoms |
| 14.05 | Clinical examination revealed upper limb ischaemia |
| 14.10 | Electrocardiography exhibited atrial fibrillation with a resting heart rate of 110 b.p.m. |
| 14.15 | Duplex sonography revealed thrombotic occlusion of the axillary and brachial arteries |
| 15.00 | Digital subtraction angiography performed confirming suspected diagnosis |
| 15.10 | Rotarex mechanical thrombectomy |
| 15.25 | Envoy catheter attempted from antegrade (not possible due to limited catheter length) |
| 15.45 | Puncture of the distal radial artery |
| 15.50 | 5F Envoy catheter aspiration from retrograde |
| 16.15 | Complete flow restoration in both the radial and ulnar arteries |
| Day 2 | Duplex sonography at the next day showing good flow profiles |
| Day 4 | Patient discharged |
| After 3 months | Patient remains uneventful without ischaemic symptoms or functional deficits |
Case presentation
Herein, we present a case of an 83-year-old female patient who presented with acute left upper limb pain, pulselessness, and paraesthesia. The patient had a history of arterial hypertension and was on treatment with 16 mg candesartan per day at the time of admission. Duplex sonography revealed thrombotic occlusion of the axillary and brachial arteries and severely diminished flow both in the ulnar and radial arteries. Electrocardiography exhibited atrial fibrillation with a resting heart rate of 110 b.p.m. Due to the severe symptoms of the patient, staged as Rutherford grade IIB, reperfusion was promptly scheduled and performed. Thus, after puncture of the right common femoral artery, digital subtraction angiography confirmed the occlusion of the distal axillary and brachial artery (Figure 1A) with slow flow reconstitution in the ulnar and radial arteries (Figure 1B). (Video 1) Rotarex® 6F mechanical thrombectomy catheter was performed (Figure 1C), which resulted in thrombus resolution in the brachial artery but unfortunately led to relevant peripheral embolization, causing occlusion of both the radial and ulnar arteries (Figure 1D). (Video 2) Since (i) catheter aspiration was not possible due to limited catheter lengths and (ii) the diameter of the 6F Rotarex® catheter was considered too large for selective thrombectomy in the radial and ulnar arteries, puncture of the distal radial was attempted to facilitate retrograde thrombus aspiration. Indeed, the distal radial artery could be successfully punctured in the snuff box using the antegrade wire as a marker. After successful puncture, a 0.018″ guidewire and a 5F sheath were inserted into the artery (Figure 1E). Subsequently 5F Envoy catheter aspiration was performed (Figure 1F and G), which lead to complete flow restoration in both the radial and ulnar arteries of the patient (Figure 1H–J) (Video 3) and to complete resolution of her ischaemic symptoms. Duplex sonography at the next day revealed biphasic flow of the brachial and hyperaemic monophasic flow of the distal radial and ulnar artery.
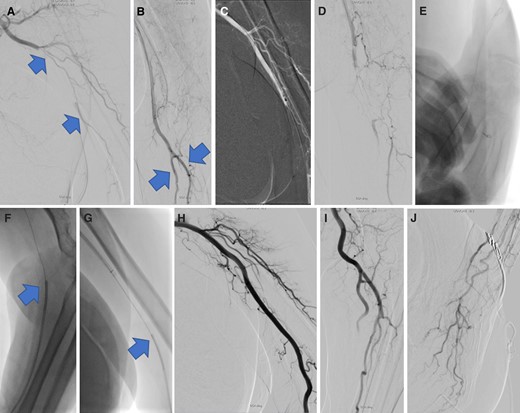
Digital subtraction angiography confirmed occlusion of the brachial artery (arrows in A) with slow flow reconstitution in the ulnar and radial arteries (arrows in B). Rotarex 6F thrombectomy was used (C), resulting in thrombus resolution in the brachial artery but leading to distal embolization and occlusion of the radial and ulnar arteries (D). Distal radial puncture, and insertion of a 5F sheath was subsequently performed (E), facilitating retrograde 5F Envoy catheter aspiration (F and G). This led to complete flow restoration in both the radial and ulnar arteries of the patient (H–J).
In addition, echocardiography was performed, demonstrating good systolic left ventricular (LV) function with normal LV (LV end-diastolic diameter = 42 mm, LV ejection fraction = 56%, and LV end-diastolic volume = 101 mL) and increased left atrial diameter (45 mm). Transoesophageal echocardiography excluded the presence of residual thrombus in the left atrial appendix. During the hospital stay, our patient spontaneously converted to sinus rhythm and was discharged without functional deficits 3 days after the index procedure. A combination treatment of rivaroxaban (15 mg/day) and clopidogrel (75 mg/day) for 3 months, followed by rivaroxaban (20 mg/day) thereafter was recommended. After 3 months, the patient remained uneventful without ischaemic symptoms or functional deficits of her hand.
Discussion
To our knowledge this is the first case, describing distal puncture of the radial artery for retrograde thrombus aspiration. Traditionally, the radial artery has been used for many years in interventional cardiology as an access site of the first choice for cardiac catheterization and percutaneous coronary intervention (PCI). Within the last years, several studies and meta-analyses also reported on the feasibility and superior safety of the distal radial approach, also known as the ‘snuff box’ access site for cardiac interventions.5 Typically, after skin anaesthesia, the distal radial artery is punctured in the anatomical snuff box with a 20-gauge needle. The puncture is typically performed with digital palpation of the pulse. Alternatively, in cases of non-palpable distal radial arteries, ultrasound guidance may be helpful to achieve successful puncture of the vessel, since puncture of the distal radial artery may be more challenging than with a regular transradial approach due to a smaller arterial lumen diameter. In addition, special haemostatic pads are necessary to achieve haemostasis after a distal radial approach. Based on current data, however, both haemorrhagic and thrombotic complications may be lower with a distal vs. a regular radial approach, whereas the repeated use of a distal transradial approach seems to be feasible and safe.6,7 In our case, distal thrombectomy could have also been performed by a regular transradial approach. This was indeed attempted during the procedure but was not successful, possibly due to the occlusion of this part of the artery. Thus, the distal radial artery was ‘the last remaining hope’. Generally, 6F guiding sheaths can be inserted after puncture of the distal radial artery, which would allow the use of 5F or 6F aspiration catheters. In our case, due to the occlusion of distal arteries, possibly associated with vasoconstriction and vessel fragility, we decided to use lower profile a 5F approach first for distal thrombectomy.
The incidence of ALI is about 1.5 cases per 10 000 individuals annually and is associated with a high rate of limb loss up to 40% and death rates up to 20% during the index hospitalization.8 Most of the thromboembolic events associated with arterial occlusion originate from the heart, usually associated with undiagnosed atrial fibrillation. Current guidelines recommend expedited diagnosis and treatment of patients with ALI.3 However, the treatment of choice among endovascular and surgical approaches is still not clear and therefore subject of ongoing research. Basically, both surgical and endovascular techniques may be considered, with the latter possibly having lower mortality rates, particularly in elderly and frail patients. In addition, local lysis is frequently used to treat thrombotic occlusion of peripheral vessels. However, even though with local lysis substantially lower dosages are necessary compared with systemic lysis, both with local and systemic lysis, bleeding complications need to be considered especially with older patients. Therefore, our primary strategy in such cases is restoration of flow by mechanical means, including Rotarex catheter thrombectomy and catheter aspiration. If flow cannot be restored by these means, or large thrombotic burden remains despite partial restoration of flow, local lysis is performed as a bail-out strategy. In this regard, a comparative study revealed the advantage of mechanical thrombectomy compared with local lysis, which was associated with reduced rates of major bleeding, shorter hospitalization, and lower costs in patients with ALI.9 Advantages and disadvantages of the different strategies, including mechanical thrombectomy, catheter aspiration, and local lysis, are depicted in Table 1.
Pros and contras of different endovascular strategies for the treatment of acute limb ischaemia
| . | Advantages . | Disadvantages and potential complications . |
|---|---|---|
| Mechanical thrombectomy (Rotarex catheter) |
|
|
| Catheter aspiration |
|
|
| Local lysis |
|
|
| . | Advantages . | Disadvantages and potential complications . |
|---|---|---|
| Mechanical thrombectomy (Rotarex catheter) |
|
|
| Catheter aspiration |
|
|
| Local lysis |
|
|
Pros and contras of different endovascular strategies for the treatment of acute limb ischaemia
| . | Advantages . | Disadvantages and potential complications . |
|---|---|---|
| Mechanical thrombectomy (Rotarex catheter) |
|
|
| Catheter aspiration |
|
|
| Local lysis |
|
|
| . | Advantages . | Disadvantages and potential complications . |
|---|---|---|
| Mechanical thrombectomy (Rotarex catheter) |
|
|
| Catheter aspiration |
|
|
| Local lysis |
|
|
Oral anticoagulation is the pharmacologic treatment of choice after re-establishment of antegrade flow in such cases with cardioembolic arterial occlusion in patients with atrial fibrillation. In our case, we decided to treat our patient with oral anticoagulation and clopidogrel for 3 months due to possible intimal irritation caused by relatively large lumen (5F) aspiration catheter in this rather small radial artery. Notably, single oral anticoagulation or a shorter duration of dual pathway inhibition of only 4 weeks may also have been sufficient. On the other hand, the dose of the oral anticoagulation was reduced to 15 mg during the duration of the dual pathway inhibition.
Recently, the advantages of the retrograde vs. the antegrade recanalization approach for the treatment of patients with chronic PAD have been demonstrated.10 The low complication rate of endovascular treatment may be partially transferable in the ALI setting, especially in cases with subacute thrombosis or mixed aetiology, being related to both embolism and chronic PADs.
Conclusions
The emerging technical developments within the last decade offer several advantages of minimal invasive treatment over traditional surgical techniques. Herein, we report on the retrograde retrieval of thrombotic material after distal radial puncture in a patient with upper ALI. Interventionists may consider this as an option for the endovascular management of ALI in cases of cardiac embolism, as described herein or in cases of thrombotic complications during routine transradial cardiac catheterization and PCI.
Lead author biography
 Prof. Dr Grigorios Korosoglou was born on 10 November 1976. Since January 2015, he is the Chair of the Department of Cardiology and Vascular Medicine in the GRN Academic Teaching Hospital Weinheim. He and his group have published over 190 peer-reviewed scientific articles on cardiac imaging, focusing on imaging the atherosclerotic plaque and the detection of myocardial ischaemia. Furthermore, he is currently the elected Vice Chair (2018–2021) of the working group cardiac computed tomography. Grigorios Korosoglou has received several prizes and institutional grants for experimental and clinical studies in cardiac imaging and vascular medicine.
Prof. Dr Grigorios Korosoglou was born on 10 November 1976. Since January 2015, he is the Chair of the Department of Cardiology and Vascular Medicine in the GRN Academic Teaching Hospital Weinheim. He and his group have published over 190 peer-reviewed scientific articles on cardiac imaging, focusing on imaging the atherosclerotic plaque and the detection of myocardial ischaemia. Furthermore, he is currently the elected Vice Chair (2018–2021) of the working group cardiac computed tomography. Grigorios Korosoglou has received several prizes and institutional grants for experimental and clinical studies in cardiac imaging and vascular medicine.
Supplementary material
Supplementary material is available at European Heart Journal – Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written informed consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidelines.
Conflict of interest: None declared.
Funding: None declared.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- anticoagulation
- atrial fibrillation
- percutaneous coronary intervention
- ischemia
- coronary angiography
- cardiologists
- ultrasonography, doppler, duplex
- ischemia, limb, acute
- cardiac embolism
- embolization
- brachial artery
- catheterization
- radial artery
- surgical procedures, operative
- thrombectomy
- ulnar artery
- arm
- diagnosis
- thrombus
- catheters
- thrombotic occlusion
- thrombus aspiration
- acute ischemia of upper limb
- site of access
- chronic limb-threatening ischemia
- fluid flow




Comments