-
PDF
- Split View
-
Views
-
Cite
Cite
Elizabeth D Paratz, Laura Ross, Dominica Zentner, Natalie Morgan, Heinrich Bouwer, Matthew Lynch, Sarah Parsons, Andre La Gerche, Intracoronary IgG4-related disease as an unusual cause of sudden cardiac arrest: a case series, European Heart Journal - Case Reports, Volume 6, Issue 2, February 2022, ytac050, https://doi.org/10.1093/ehjcr/ytac050
Close - Share Icon Share
Abstract
IgG4-related disease (IgG4-RD) is a fibro-inflammatory condition classically causing retroperitoneal fibrosis, aortitis, thyroiditis, or pancreatitis. Diagnosis includes the presence of lymphoplasmacytic infiltrate (with >40% ratio IgG4+:IgG plasma cells) and fibrosis. Cardiac involvement may include aortic, pericardial, or coronary disease. Coronary manifestations encompass obstructive intra-luminal lesions, external encasing pseudo-tumour on imaging, or lymphoplasmacytic arteritis.
Case 1: A fit and healthy 50-year-old man was found deceased. His only known medical condition was treated Hashimoto’s thyroiditis. Post-mortem examination demonstrated an isolated severe stenosis of the left anterior descending (LAD) coronary artery without histopathological evidence of acute myocardial infarction. Coronary plaque histopathology showed florid IgG4-positive plasma cell infiltrate throughout all layers of the artery with dense fibrous tissue connective tissue stroma, all features consistent with coronary artery IgG4-RD. Case 2: A 48-year-old man collapsed at work. Computed tomography scan 1 week prior reported an ill-defined para-aortic retroperitoneal soft tissue density. No cardiac symptoms were reported in life. Post-mortem examination showed coronary arteritis and peri-arteritis with sclerosing peri-aortitis in the LAD. There was myocardial fibrosis of the anterior left ventricle and focal myocarditis of the right ventricle.
IgG4-related disease presenting as sudden cardiac death without any preceding symptoms is very rare (six prior cases identified on literature review). Reported targeted successful interventions for intracoronary IgG4-RD diagnosed in life have included steroid therapy and B cell depleting therapy (i.e. rituximab). If cardiac symptoms are present in a patient with known IgG4-RD, cardiac investigations should be promptly arranged.
IgG4-related disease (IgG4-RD) is a rare and unusual cause of non-atherosclerotic coronary artery disease that may manifest as sudden cardiac arrest.
An index of suspicion for IgG4-RD affecting coronary arteries should be maintained for select patients with IgG4-RD reporting cardiac symptoms, or coronary disease and unexplained systemic signs.
Multidisciplinary physician investigation is strongly encouraged in order to diagnose IgG4-RD given the complexity of diagnosis.
Primary Specialties involved other than cardiology
Rheumatology, Forensic Pathology
Introduction
IgG4-related disease (IgG4-RD) is an autoimmune fibro-inflammatory condition that was first defined as a distinct condition in 2001. It most commonly presents with submandibular gland, lymph node or orbital involvement.1 Recognized cardiac manifestations include aortitis or pericardial manifestations. Coronary involvement has only been infrequently reported.2
This case series describes two patients referred to the Victorian Institute of Forensic Medicine (VIFM) in Victoria, Australia after sudden death, who were found on post-mortem examination to have IgG4-RD coronary disease.
Timeline
| . | Patient 1 . | Patient 2 . |
|---|---|---|
| Presentation | 50- year-old Caucasian man | 48-year-old Caucasian man |
| Pre-mortem | No known cardiac medical history or symptoms |
|
| At time of cardiac arrest | Cardiac arrest while chopping wood | Cardiac arrest while at work |
| Post-mortem examination | 90% proximal left anterior descending (LAD) coronary lesion identified | Multi-vessel coronary per-arteritis and sclerosing peri-aortitis |
| Additional post-mortem investigations | Histopathology of LAD lesion demonstrated extensive infiltrate of plasma cells with large number of IgG4+ and IgG+ cells. Dense fibrous connective tissue stroma which was storiform in areas | Histopathology of coronary arteries demonstrated transmural inflammation, with large number of IgG4+ cells |
| . | Patient 1 . | Patient 2 . |
|---|---|---|
| Presentation | 50- year-old Caucasian man | 48-year-old Caucasian man |
| Pre-mortem | No known cardiac medical history or symptoms |
|
| At time of cardiac arrest | Cardiac arrest while chopping wood | Cardiac arrest while at work |
| Post-mortem examination | 90% proximal left anterior descending (LAD) coronary lesion identified | Multi-vessel coronary per-arteritis and sclerosing peri-aortitis |
| Additional post-mortem investigations | Histopathology of LAD lesion demonstrated extensive infiltrate of plasma cells with large number of IgG4+ and IgG+ cells. Dense fibrous connective tissue stroma which was storiform in areas | Histopathology of coronary arteries demonstrated transmural inflammation, with large number of IgG4+ cells |
| . | Patient 1 . | Patient 2 . |
|---|---|---|
| Presentation | 50- year-old Caucasian man | 48-year-old Caucasian man |
| Pre-mortem | No known cardiac medical history or symptoms |
|
| At time of cardiac arrest | Cardiac arrest while chopping wood | Cardiac arrest while at work |
| Post-mortem examination | 90% proximal left anterior descending (LAD) coronary lesion identified | Multi-vessel coronary per-arteritis and sclerosing peri-aortitis |
| Additional post-mortem investigations | Histopathology of LAD lesion demonstrated extensive infiltrate of plasma cells with large number of IgG4+ and IgG+ cells. Dense fibrous connective tissue stroma which was storiform in areas | Histopathology of coronary arteries demonstrated transmural inflammation, with large number of IgG4+ cells |
| . | Patient 1 . | Patient 2 . |
|---|---|---|
| Presentation | 50- year-old Caucasian man | 48-year-old Caucasian man |
| Pre-mortem | No known cardiac medical history or symptoms |
|
| At time of cardiac arrest | Cardiac arrest while chopping wood | Cardiac arrest while at work |
| Post-mortem examination | 90% proximal left anterior descending (LAD) coronary lesion identified | Multi-vessel coronary per-arteritis and sclerosing peri-aortitis |
| Additional post-mortem investigations | Histopathology of LAD lesion demonstrated extensive infiltrate of plasma cells with large number of IgG4+ and IgG+ cells. Dense fibrous connective tissue stroma which was storiform in areas | Histopathology of coronary arteries demonstrated transmural inflammation, with large number of IgG4+ cells |
Case summary
Patient 1
A 50-year-old Caucasian man experienced a sudden cardiac arrest while chopping wood. He was found pulseless by bystanders and declared deceased by paramedics. His only known medical history was that of treated Hashimoto’s thyroiditis. Interview of his next of kin and treating general practitioner endorsed that he never reported cardiac symptoms in life and had never undergone cardiac investigations. Due to the unexplained nature of his sudden death, the patient was referred to the coroner for further investigations.
Post-mortem examination demonstrated a severe lesion in the proximal left anterior descending (LAD) coronary artery with 90% luminal narrowing (Figure 1). The macroscopic examination did not reveal recent or remote infarct in the corresponding myocardium. The aorta and left main coronary artery appeared macroscopically normal.

On histopathological analysis of the LAD lesion, there was an extensive infiltrate of plasma cells extending from the tunica adventitia to the media. These plasma cells showed kappa and lambda immunoreactivity, with a large number of IgG4+ and IgG+ cells. There was a dense fibrous connective tissue stroma which in areas was storiform with occasional eosinophils at the periphery of the vessels. Focal obliterative phlebitis was also seen.
With regards to extra-cardiac autopsy findings, Hashimoto’s thyroiditis was confirmed with dense lymphoid follicle formation and associated fibrosis. His lungs also showed minor interstitial inflammation. There was no overt disease identified of the aorta, pancreas, or any retroperitoneal fibrosis to implicate these organs as being simultaneously affected by IgG4-RD.
The cause of death was determined to be florid IgG4-RD primarily affecting the LAD coronary artery, causing severe stenosis.
Patient 2
A 48-year-old Caucasian man collapsed at work and was unable to be resuscitated. The patient was being investigated for lethargy and weight loss at the time of his death with a computed tomography scan performed 1 week prior to death reporting splenomegaly and an ill-defined para-aortic soft tissue density within the retroperitoneum. A desquamating dermatitis of the hands was noted in the days prior to death. A strong family history of autoimmune conditions was present. No cardiac symptoms had been reported during any pre-mortem evaluations.
Post-mortem examination showed multi-vessel coronary artery peri-arteritis and features suggestive of IgG4-RD. Sclerosing peri-aortitis was also identified in the common iliac artery and abdominal aorta. There was myocardial fibrosis of the left ventricle and focal myocarditis in the right ventricle.
Histopathology of the main coronary arteries demonstrated transmural inflammation, with an infiltrate of plasma cells and lymphocytes and a large number of IgG4+ cells. There was fibrous tissue infiltration of the adventitia, some of which was storiform and occasional eosinophils at the periphery of vessels. Non-obstructive atherosclerotic plaques were also identified.
Extra-cardiac findings at autopsy included steatohepatitis, splenomegaly (with normal histology), and diverticular disease.
The cause of death was determined to be ischaemic heart disease as a consequence of coronary arteritis and peri-arteritis with IgG4+ cells.
Discussion
These two cases are unusual in that they describe non-atherosclerotic mechanisms of fatal coronary artery obstruction, with coronary stenosis caused by direct infiltration of IgG4+ plasma cells. The post-mortem nature of these cases provides a rare opportunity for detailed histological coronary artery analysis, directly implicating IgG4+ infiltration as the culprit pathology.
Although the interaction of coronary artery disease and connective tissue disease has been well-described, these cases present a novel form of interaction. Typically, atherosclerotic coronary artery disease is accelerated in diseases such as systemic lupus erythematosus and rheumatoid arthritis due to systemic inflammation. In those conditions, the hyper-inflammatory state acts as a promoter of typical atherosclerosis. However, in the IgG4-RD cases described, the accumulation of pathological non-atherosclerotic stenosis occurred due to direct disease infiltration, with potential implications for clinical management.
How common is cardiac and particularly coronary involvement in IgG4-related disease?
IgG4-related disease is a rare autoimmune disease defined by a characteristic clinical presentation and the presence of fibro-inflammatory lesions, with dense lymphocytic infiltrate and storiform fibrosis and an elevated ratio of IgG4+ to IgG4 cells1 (Figure 2). Unlike most autoimmune conditions, it affects males more commonly, with a reported preponderance of up to 15:12: the reasons for this marked gender disparity are unclear.
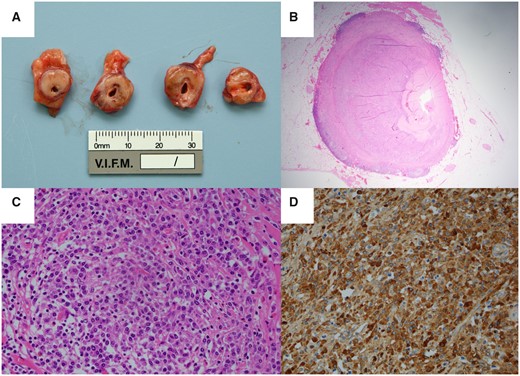
(A) Cross-sections of the proximal left anterior descending coronary artery demonstrate infiltration by firm, pale tissue atypical for atherosclerotic plaque. (B) There is near-complete luminal occlusion. (C) Haematoxylin and eosin staining identifies a florid and extensive infiltrate of plasma cells that extend from the tunica adventitia to the media. (D) IgG4 immunostaining demonstrates that a high proportion of these cells are IgG4+.
The most common reported forms of cardiac involvement in IgG4-RD are aortitis or pericardial involvement (up to 50% of cases of inflammatory aortitis are believed to be due to IgG4-RD).3 Coronary artery involvement has only been identified very rarely in case reports and may include obstructive intracoronary lesions, external encasing pseudo-tumour, or aneurysm formation.4 It is possible that coronary artery involvement from IgG4-RD remains an under-reported disease manifestation due to it being falsely attributed to atherosclerotic coronary artery disease clinically, which is very common in middle-aged and older males.
Patient identification
In both cases, our patients lacked pre-mortem cardiac symptoms. This underscores the challenging nature of identifying patients at risk for sudden cardiac arrest. A review of the literature reveals that most patients with sudden cardiac arrest as a complication of IgG4-RD coronary disease had no prior cardiac symptoms (Table 1). Sudden cardiac death occurred exclusively in males, with a wide age range of 38–91 years.
Literature review of coronary IgG4-related disease associated with sudden cardiac arrest
| Author, year . | Case description . | Coronary findings at autopsy . | Other organs affected . | IgG4-RD diagnosed pre-mortem? . | Symptoms in life . |
|---|---|---|---|---|---|
| Gutierrez et al., 20138 | 54-year-old male with sudden cardiac arrest after syncopal event at home | Aneurysms and semi-occlusive thrombosis of proximal LAD and RCA. No significant coronary atherosclerosis, and high number of IgG4 positive cells (94 cells/HPF) | No | No | Nil detailed |
| Patel et al., 20143 | 53-year-old male with sudden cardiac arrest | Proximal coronary arteries displayed conspicuously thick walls and encased by pink-tan, fleshy tissue. Sub-acute myocardial infarction of the anterolateral left ventricular wall. | Pancreatic and renal involvement, lymphadenopathy | No | Complained of chest pain prior to asystolic cardiac arrest |
| NB coexistent severe atherosclerotic triple-vessel coronary disease and coronary thrombosis identified at autopsy. | |||||
| Inokuchi et al., 20144 | 38-year-old male with sudden cardiac death (unwitnessed) | Severe stenosis and occlusion due to atherosclerosis and thrombus in mid-distal RCA. The entire vascular wall of the RCA was thickened, particularly at these lesion sites. | No | No | Nil |
| Treacy et al., 20159 | 3 males, age range 55–91 years old with sudden cardiac death | Firm, white and whorled masses surrounding atheromatous left and right coronary arteries. Positive staining with IgG4 was identified in two of three cases, with a mean count of >50 IgG4 positive cells per HPF and IgG4: IgG ratio >50% | Not detailed | Not detailed | Not detailed |
| Bukiri et al., 202010 | 55-year-old male with sudden cardiac death | LM and LAD near-occluded with lymphocytes and plasma cells: diagnosis of obliterative/occlusive coronary vasculitis with storiform fibrosis. Staining for IgG4-expressing plasma cells not performed. | Polychondritis | Diagnosed with relapsing polychondritis aged 34 years old—on immunosuppressive therapy | Auricular chondritis |
| Nasal deformity | |||||
| Polychondritis |
| Author, year . | Case description . | Coronary findings at autopsy . | Other organs affected . | IgG4-RD diagnosed pre-mortem? . | Symptoms in life . |
|---|---|---|---|---|---|
| Gutierrez et al., 20138 | 54-year-old male with sudden cardiac arrest after syncopal event at home | Aneurysms and semi-occlusive thrombosis of proximal LAD and RCA. No significant coronary atherosclerosis, and high number of IgG4 positive cells (94 cells/HPF) | No | No | Nil detailed |
| Patel et al., 20143 | 53-year-old male with sudden cardiac arrest | Proximal coronary arteries displayed conspicuously thick walls and encased by pink-tan, fleshy tissue. Sub-acute myocardial infarction of the anterolateral left ventricular wall. | Pancreatic and renal involvement, lymphadenopathy | No | Complained of chest pain prior to asystolic cardiac arrest |
| NB coexistent severe atherosclerotic triple-vessel coronary disease and coronary thrombosis identified at autopsy. | |||||
| Inokuchi et al., 20144 | 38-year-old male with sudden cardiac death (unwitnessed) | Severe stenosis and occlusion due to atherosclerosis and thrombus in mid-distal RCA. The entire vascular wall of the RCA was thickened, particularly at these lesion sites. | No | No | Nil |
| Treacy et al., 20159 | 3 males, age range 55–91 years old with sudden cardiac death | Firm, white and whorled masses surrounding atheromatous left and right coronary arteries. Positive staining with IgG4 was identified in two of three cases, with a mean count of >50 IgG4 positive cells per HPF and IgG4: IgG ratio >50% | Not detailed | Not detailed | Not detailed |
| Bukiri et al., 202010 | 55-year-old male with sudden cardiac death | LM and LAD near-occluded with lymphocytes and plasma cells: diagnosis of obliterative/occlusive coronary vasculitis with storiform fibrosis. Staining for IgG4-expressing plasma cells not performed. | Polychondritis | Diagnosed with relapsing polychondritis aged 34 years old—on immunosuppressive therapy | Auricular chondritis |
| Nasal deformity | |||||
| Polychondritis |
HPF, high-power field; IgG4-RD, IgG4-related disease; LAD, left anterior descending coronary artery; LM, left main coronary artery; RCA, right coronary artery.
Literature review of coronary IgG4-related disease associated with sudden cardiac arrest
| Author, year . | Case description . | Coronary findings at autopsy . | Other organs affected . | IgG4-RD diagnosed pre-mortem? . | Symptoms in life . |
|---|---|---|---|---|---|
| Gutierrez et al., 20138 | 54-year-old male with sudden cardiac arrest after syncopal event at home | Aneurysms and semi-occlusive thrombosis of proximal LAD and RCA. No significant coronary atherosclerosis, and high number of IgG4 positive cells (94 cells/HPF) | No | No | Nil detailed |
| Patel et al., 20143 | 53-year-old male with sudden cardiac arrest | Proximal coronary arteries displayed conspicuously thick walls and encased by pink-tan, fleshy tissue. Sub-acute myocardial infarction of the anterolateral left ventricular wall. | Pancreatic and renal involvement, lymphadenopathy | No | Complained of chest pain prior to asystolic cardiac arrest |
| NB coexistent severe atherosclerotic triple-vessel coronary disease and coronary thrombosis identified at autopsy. | |||||
| Inokuchi et al., 20144 | 38-year-old male with sudden cardiac death (unwitnessed) | Severe stenosis and occlusion due to atherosclerosis and thrombus in mid-distal RCA. The entire vascular wall of the RCA was thickened, particularly at these lesion sites. | No | No | Nil |
| Treacy et al., 20159 | 3 males, age range 55–91 years old with sudden cardiac death | Firm, white and whorled masses surrounding atheromatous left and right coronary arteries. Positive staining with IgG4 was identified in two of three cases, with a mean count of >50 IgG4 positive cells per HPF and IgG4: IgG ratio >50% | Not detailed | Not detailed | Not detailed |
| Bukiri et al., 202010 | 55-year-old male with sudden cardiac death | LM and LAD near-occluded with lymphocytes and plasma cells: diagnosis of obliterative/occlusive coronary vasculitis with storiform fibrosis. Staining for IgG4-expressing plasma cells not performed. | Polychondritis | Diagnosed with relapsing polychondritis aged 34 years old—on immunosuppressive therapy | Auricular chondritis |
| Nasal deformity | |||||
| Polychondritis |
| Author, year . | Case description . | Coronary findings at autopsy . | Other organs affected . | IgG4-RD diagnosed pre-mortem? . | Symptoms in life . |
|---|---|---|---|---|---|
| Gutierrez et al., 20138 | 54-year-old male with sudden cardiac arrest after syncopal event at home | Aneurysms and semi-occlusive thrombosis of proximal LAD and RCA. No significant coronary atherosclerosis, and high number of IgG4 positive cells (94 cells/HPF) | No | No | Nil detailed |
| Patel et al., 20143 | 53-year-old male with sudden cardiac arrest | Proximal coronary arteries displayed conspicuously thick walls and encased by pink-tan, fleshy tissue. Sub-acute myocardial infarction of the anterolateral left ventricular wall. | Pancreatic and renal involvement, lymphadenopathy | No | Complained of chest pain prior to asystolic cardiac arrest |
| NB coexistent severe atherosclerotic triple-vessel coronary disease and coronary thrombosis identified at autopsy. | |||||
| Inokuchi et al., 20144 | 38-year-old male with sudden cardiac death (unwitnessed) | Severe stenosis and occlusion due to atherosclerosis and thrombus in mid-distal RCA. The entire vascular wall of the RCA was thickened, particularly at these lesion sites. | No | No | Nil |
| Treacy et al., 20159 | 3 males, age range 55–91 years old with sudden cardiac death | Firm, white and whorled masses surrounding atheromatous left and right coronary arteries. Positive staining with IgG4 was identified in two of three cases, with a mean count of >50 IgG4 positive cells per HPF and IgG4: IgG ratio >50% | Not detailed | Not detailed | Not detailed |
| Bukiri et al., 202010 | 55-year-old male with sudden cardiac death | LM and LAD near-occluded with lymphocytes and plasma cells: diagnosis of obliterative/occlusive coronary vasculitis with storiform fibrosis. Staining for IgG4-expressing plasma cells not performed. | Polychondritis | Diagnosed with relapsing polychondritis aged 34 years old—on immunosuppressive therapy | Auricular chondritis |
| Nasal deformity | |||||
| Polychondritis |
HPF, high-power field; IgG4-RD, IgG4-related disease; LAD, left anterior descending coronary artery; LM, left main coronary artery; RCA, right coronary artery.
In rheumatological guidelines, screening for coronary artery involvement does not form part of guidelines for the evaluation of IgG4-RD.1 Identification of coronary disease will therefore occur only incidentally, or due to investigation of cardiac symptoms in the minority who experience these. A complementary population are those with known coronary disease who have unexplained systemic symptoms and signs such as concomitant aortitis and will be ultimately diagnosed with IgG4-RD (Figure 3). If IgG4-RD is considered as a causation of a patient’s coronary disease, multidisciplinary involvement is highly recommended to ensure that strict diagnostic criteria are met, and that possible disease mimics are considered and excluded.
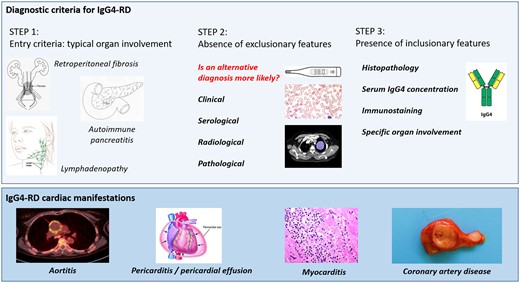
The American College of Rheumatology and European League Against Rheumatism (ACR/EULAR) guidelines emphasize the complexity of diagnosing IgG4-related disease. A variety of cardiac manifestations have been reported in the presentation of this pleiotropic disease.
Diagnosis of coronary involvement in IgG4-related disease
Diagnosis in the post-mortem setting is possible with examination of the coronary arteries. In living patients, differentiation between typical atherosclerotic vs. IgG4+ stenosis is more challenging.
Initial diagnosis of obstructive coronary disease can be achieved by conventional means such as coronary computed tomographic angiography or invasive coronary angiography. To define the lesions as being specifically IgG4-related is, however, more problematic. Current assessments of the role of magnetic resonance imaging or positron emission tomography (PET scan) to identify vascular involvement in IgG4-RD have been largely limited to medium- and large-vessel involvement.5 Coronary lesions with large pseudo-tumour formation, ectasia or circumferential mural enhancement are more likely to be recognized as being driven by vasculitis6 but, otherwise, an assessment of coronary disease as being a ‘possible’ or ‘probable’ complication of IgG4-RD may be based on clinical context and response to conventional revascularization strategies.
Management of IgG4-related disease
It is possible that failure to recognize IgG4-RD coronary disease may lead to attempted coronary revascularization, either by percutaneous coronary intervention or coronary artery bypass surgery.2,7 It is unclear whether these thickened fibrosed vessels would respond predictably to percutaneous intervention. Concerns exist for increased risk of anastomotic failure or tissue dehiscence in the setting of bypass surgery or in-stent restenosis if underlying inflammatory disease is uncontrolled.
For patients with identified coronary IgG4-RD, systemic immunotherapies such as steroid therapy and B cell depleting therapy may successfully treat coronary lesions.7 This offers a potential new paradigm for management of severe coronary disease in patients with recognized IgG4-RD. Whether such treatment reduces the incidence of sudden cardiac death is unknown, particularly if the primary trigger is a ventricular arrhythmia due to myocardial fibrosis.
Conclusion
IgG4-related disease is an unusual cause of coronary artery stenosis and may manifest as sudden cardiac death. In life, clinical suspicion for autoimmune inflammatory diseases such as IgG4-RD as the cause of coronary disease is likely limited to patients with a pre-existing IgG4-RD diagnosis. However, clinicians should be aware of the potential of this disease to cause coronary occlusion.
Lead author biography
Elizabeth D. Paratz is an early-career cardiologist and in the final year of her PhD at the Baker Heart & Diabetes Institute. She works clinically at three hospitals (St Vincent’s Hospital Melbourne, St Vincent’s Private Hospital, and Alfred Hospital) and is a clinical lecturer for Melbourne University (SVH Clinical School). She is an Associate Editor for European Heart Journal-Case Reports and regular peer reviewer for international cardiology journals. She is also Deputy Medical Director of the East Timor Hearts Fund, travelling there annually to provide volunteer cardiac services and leading ETHF’s research programme year-round.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The next of kin of each patient provided written consent for the patient’s cases to be published.
Conflict of interest: none declared.
Funding: This work was supported by the Ross Dennerstein Foundation™. E.D.P. is supported by an NHMRC/NHF co-funded Postgraduate Scholarship, RACP JJ Billings Scholarship and PSA Cardiovascular Scholarship. A.L.G. is supported by an NHF Future Leadership Fellowship and NHMRC Career Development Fellowship.





Comments