-
PDF
- Split View
-
Views
-
Cite
Cite
Markus Bettin, Matthias Koopmann, Gerold Mönnig, Christian Pott, Delayed occurrence of an accelerated idioventricular rhythm with alternating bundle branch block after myocardial infarction as predictor of sudden cardiac arrest: a case report, European Heart Journal - Case Reports, Volume 4, Issue 6, December 2020, Pages 1–7, https://doi.org/10.1093/ehjcr/ytaa378
Close - Share Icon Share
Abstract
Accelerated idioventricular rhythm (AIVR) is known as reperfusion arrhythmia in the setting of acute myocardial infarction (AMI). In healthy individuals, it is usually considered to be benign. Alternating bundle branch block (ABBB) often progresses to complete atrioventricular block requiring permanent pacemaker implantation. We report a case of delayed appearance of AIVR following myocardial infarction (MI) in combination with ABBB as precursor of sudden cardiac arrest due to ventricular fibrillation (VF).
A 62-year-old male with pre-existing left bundle branch block (LBBB) was admitted with an acute non-ST segment elevation MI. He underwent successful percutaneous coronary intervention (PCI) of a subtotal proximal left anterior descending artery (LAD) stenosis. Before and after PCI the electrocardiogram (ECG) demonstrated sinus rhythm with LBBB. The patient was discharged 5 days after PCI, left ventricular function at this time was moderately reduced (ejection fraction of 40%). After another 5 days, the patient was admitted for elective cardiac rehabilitation. At this time, the ECG demonstrated an AIVR with right bundle branch block morphology. Due to ABBB, the patient was scheduled for permanent pacemaker implantation. Before pacemaker implantation could take place, the patient developed a sudden cardiac arrest due to VF and was successfully resuscitated. A follow-up coronary angiography revealed no novel lesions. A cardiac resynchronization therapy defibrillator was implanted for secondary prevention of sudden cardiac death.
Delayed occurrence of AIVR in combination with ABBB following AMI could be a predictor of sudden cardiac death. These patients are probably at high risk for malignant ventricular arrhythmias.
Accelerated idioventricular rhythm (AIVR) usually occurs in acute myocardial infarction (MI) as marker of reperfusion and is mostly considered to be benign.
In our case, delayed occurrence of idioventricular rhythm with alternating bundle branch block (ABBB) was a precursor for ventricular fibrillation and sudden cardiac arrest.
Therefore, patients with documented AIVR with ABBB following MI and reduced ejection fraction should be monitored thoroughly not only for bradycardia, but also for ventricular tachyarrhythmias.
Introduction
Accelerated idioventricular rhythm (AIVR) is defined as a ventricular rhythm with three or more consecutive monomorphic beats due to an ectopic focus localized in the bundle of His or the Purkinje fibres, accompanied by gradual onset and termination.1 Accelerated idioventricular rhythm can be seen in young patients with structurally normal hearts and is usually considered to be a benign rhythm abnormality.2 In healthy individuals with no structural heart disease, AIVR may be caused by increased vagal and decreased sympathetic tone.3 However, in the setting of acute myocardial infarction (MI) it can occur as reperfusion arrhythmia.4 Furthermore, AIVR has been described in other clinical situations, e.g. during drug-intoxication with digitalis.5
Alternating bundle branch block (ABBB) is defined as the intermittent presence of left bundle branch block (LBBB) in turn with intermittent right bundle branch block (RBBB), which is documented on one or successive electrocardiograms (ECGs).6 In this setting, the current guideline on cardiac pacing of the European Society of Cardiology (ESC)7 recommends pacemaker implantation even in asymptomatic patients (Class IC recommendation). Especially patients with ABBB following MI are at high risk for the development of complete heart block.8
We present the case of a 62-year-old male with delayed occurrence of an AIVR and ABBB after MI, who survived sudden cardiac arrest.
Timeline
| 22 July 2019 | Patient presents with non-ST segment elevation myocardial infarction. Immediate percutaneous coronary intervention (PCI) by DE-stent implantation into a subtotal occlusion of the proximal left anterior descending artery is performed. Electrocardiogram (ECG) before and after PCI shows sinus rhythm with previously known left bundle branch block |
| 26 July 2019 | Discharge with heart failure medication. Left ventricular ejection fraction is 40% |
| 1 August 2019 | Patient is admitted for elective cardiac rehabilitation. At this time, ECG demonstrates accelerated idioventricular rhythm with right bundle branch block. The patient is transferred to our centre for monitoring and scheduled for permanent pacemaker implantation |
| 2 August 2019 | Sudden onset of Torsade de Pointes tachycardia/ventricular fibrillation under ECG monitoring. Immediate cardiopulmonary resuscitation with two external defibrillator shocks was successfully performed. The patient survived the episode without any neurological deficits. Transfer to intensive care unit |
| 2 August 2019 | Urgent implantation of a cardiac resynchronization therapy (CRT) defibrillator as further ventricular arrhythmias occurring |
| 5 August 2020 | Routine follow-up at our implantable cardioverter-defibrillator (ICD) outpatient department. No ventricular arrhythmias are observed upon CRT-ICD readout |
| 22 July 2019 | Patient presents with non-ST segment elevation myocardial infarction. Immediate percutaneous coronary intervention (PCI) by DE-stent implantation into a subtotal occlusion of the proximal left anterior descending artery is performed. Electrocardiogram (ECG) before and after PCI shows sinus rhythm with previously known left bundle branch block |
| 26 July 2019 | Discharge with heart failure medication. Left ventricular ejection fraction is 40% |
| 1 August 2019 | Patient is admitted for elective cardiac rehabilitation. At this time, ECG demonstrates accelerated idioventricular rhythm with right bundle branch block. The patient is transferred to our centre for monitoring and scheduled for permanent pacemaker implantation |
| 2 August 2019 | Sudden onset of Torsade de Pointes tachycardia/ventricular fibrillation under ECG monitoring. Immediate cardiopulmonary resuscitation with two external defibrillator shocks was successfully performed. The patient survived the episode without any neurological deficits. Transfer to intensive care unit |
| 2 August 2019 | Urgent implantation of a cardiac resynchronization therapy (CRT) defibrillator as further ventricular arrhythmias occurring |
| 5 August 2020 | Routine follow-up at our implantable cardioverter-defibrillator (ICD) outpatient department. No ventricular arrhythmias are observed upon CRT-ICD readout |
| 22 July 2019 | Patient presents with non-ST segment elevation myocardial infarction. Immediate percutaneous coronary intervention (PCI) by DE-stent implantation into a subtotal occlusion of the proximal left anterior descending artery is performed. Electrocardiogram (ECG) before and after PCI shows sinus rhythm with previously known left bundle branch block |
| 26 July 2019 | Discharge with heart failure medication. Left ventricular ejection fraction is 40% |
| 1 August 2019 | Patient is admitted for elective cardiac rehabilitation. At this time, ECG demonstrates accelerated idioventricular rhythm with right bundle branch block. The patient is transferred to our centre for monitoring and scheduled for permanent pacemaker implantation |
| 2 August 2019 | Sudden onset of Torsade de Pointes tachycardia/ventricular fibrillation under ECG monitoring. Immediate cardiopulmonary resuscitation with two external defibrillator shocks was successfully performed. The patient survived the episode without any neurological deficits. Transfer to intensive care unit |
| 2 August 2019 | Urgent implantation of a cardiac resynchronization therapy (CRT) defibrillator as further ventricular arrhythmias occurring |
| 5 August 2020 | Routine follow-up at our implantable cardioverter-defibrillator (ICD) outpatient department. No ventricular arrhythmias are observed upon CRT-ICD readout |
| 22 July 2019 | Patient presents with non-ST segment elevation myocardial infarction. Immediate percutaneous coronary intervention (PCI) by DE-stent implantation into a subtotal occlusion of the proximal left anterior descending artery is performed. Electrocardiogram (ECG) before and after PCI shows sinus rhythm with previously known left bundle branch block |
| 26 July 2019 | Discharge with heart failure medication. Left ventricular ejection fraction is 40% |
| 1 August 2019 | Patient is admitted for elective cardiac rehabilitation. At this time, ECG demonstrates accelerated idioventricular rhythm with right bundle branch block. The patient is transferred to our centre for monitoring and scheduled for permanent pacemaker implantation |
| 2 August 2019 | Sudden onset of Torsade de Pointes tachycardia/ventricular fibrillation under ECG monitoring. Immediate cardiopulmonary resuscitation with two external defibrillator shocks was successfully performed. The patient survived the episode without any neurological deficits. Transfer to intensive care unit |
| 2 August 2019 | Urgent implantation of a cardiac resynchronization therapy (CRT) defibrillator as further ventricular arrhythmias occurring |
| 5 August 2020 | Routine follow-up at our implantable cardioverter-defibrillator (ICD) outpatient department. No ventricular arrhythmias are observed upon CRT-ICD readout |
Case presentation
A 62-year-old male with no eminent clinical history presented at our centre with an acute non-ST segment elevation myocardial infarction. Twelve-lead ECG showed sinus rhythm (SR) with previously known LBBB (Figure 1). Laboratory tests indicated a rise of cardiac troponin I. Urgent coronary angiography revealed a single coronary vessel disease with a subtotal occlusion of the proximal LAD (Figure 2). Successful percutaneous coronary intervention (PCI) was performed immediately. No arrhythmias were detected on monitor and his permanent rhythm was identical to the rhythm before PCI. After 5 days of hospitalization, the patient was discharged in good condition. Due to reduced left ventricular function (ejection fraction 40%), medical treatment of heart failure was initiated (bisoprolol 5 mg o.d., spironolactone 25 mg o.d., ramipril 5 mg o.d.).
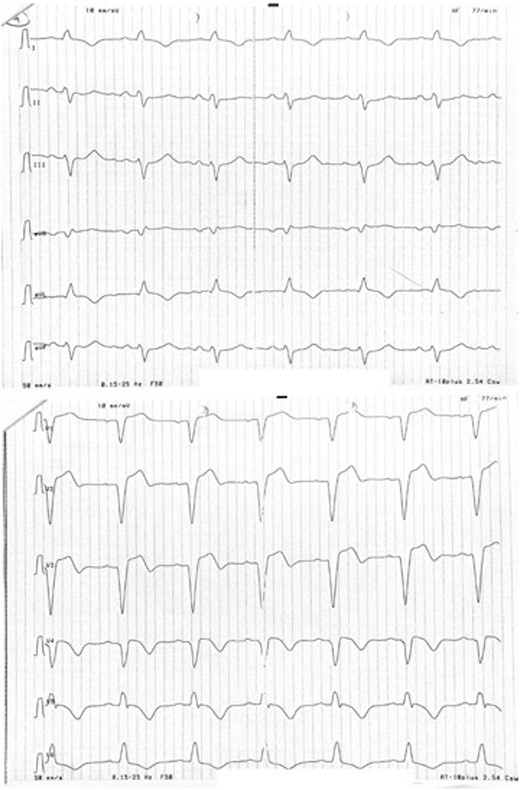
Sinus rhythm with pre-existing left bundle branch block. There were no electrocardiographic differences before and after percutaneous coronary intervention. Some remaining ST-T elevation could be an indicator of ischaemia in the setting of left bundle branch block.
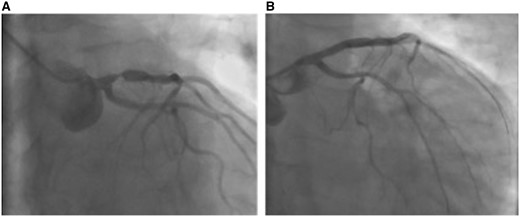
Coronary angiography and percutaneous coronary intervention. Coronary angiography revealed a subtotal stenosis of the proximal left anterior descending artery (A), which was treated by implantation of a single drug-eluting stent (B).
At admission in our Department of Cardiac Rehabilitation 10 days after PCI, the ECG demonstrated an AIVR with RBBB (Figure 3). Laboratory tests showed no electrolyte abnormalities. The patient was transferred to our intermediate care unit and was scheduled for CRT (cardiac resynchronization therapy) -pacemaker implantation. Eighteen hours after admission, sustained ventricular tachyarrhythmia was documented on ECG monitor. The morphology was compatible with Torsade de Pointes tachycardia degenerating into ventricular fibrillation (VF) (Figure 4). Shortly before the event, ECG monitor readouts showed SR with LBBB switching to AIVR with RBBB morphology (Figure 5). Two external defibrillator shocks had to be delivered and return of spontaneous circulation was achieved after 10 min of cardiopulmonary resuscitation. Another two episodes occurred after transfer to intensive care unit. Repeat coronary angiography revealed no novel coronary lesion. During the whole case history, no prolongation of the QT-interval was observed. A CRT-implantable cardioverter-defibrillator (ICD) for secondary prevention was implanted on the same day (device settings: DDD 50/min, VT-zone 188/min, VF-zone 200/min). During the implantation procedure, another three episodes of ventricular tachyarrhythmia occurred. Therefore, we began an antiarrhythmic therapy with amiodarone. After 5 months, pharmacological antiarrhythmic therapy was ceased. At follow-up of 12 months, no further episodes were found upon ICD-interrogation. Biventricular pacing was 98% and ejection fraction had slightly improved (45%).
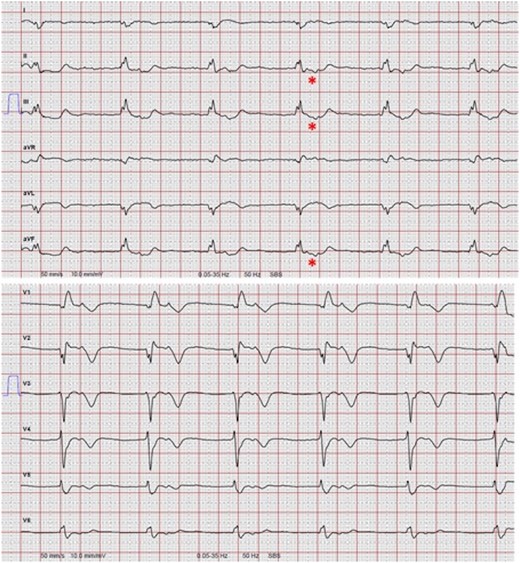
Accelerated idioventricular rhythm with right bundle branch block morphology. The electrocardiogram was recorded 10 days post-intervention at admission for cardiac rehabilitation. No P-waves precede the QRS, but the QRS appears to be followed by retrograde P-waves detectible during the ST-segment. Retrograde P-waves exhibit a vector negative in leads II, III, and aVF (*). Thus, the most likely diagnosis is an accelerated idioventricular rhythm. The wide QRS shows right bundle branch morphology.
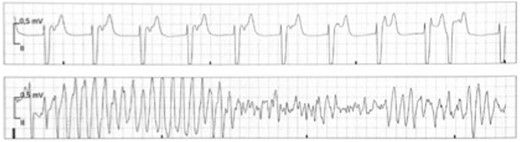
Onset of Torsade de Pointes tachycardia/ventricular fibrillation. Again, there are retrograde P-waves visible during the ST-segment confirming accelerated idioventricular rhythm. Following a short–long–short sequence, R-on-T-phenomenon initiates malignant ventricular arrhythmia compatible with Torsade de Pointes tachycardia degenerating into ventricular fibrillation.

Shift from sinus rhythm with left bundle branch block to accelerated idioventricular rhythm with right bundle branch block seconds before onset of Torsade de Pointes tachycardia/ventricular fibrillation. The fourth QRS in the second row is probably a fusion complex (*). Note that in contrast to P-wave morphology in accelerated idioventricular rhythm, P-waves during sinus rhythm exhibit an inferior axis.
Discussion
To the best of our knowledge, this is the first description of a patient who after previous MI exhibited a delayed occurrence of an AIVR combined with ABBB immediately before sudden cardiac arrest.
Escape rhythm with RBBB morphology and baseline LBBB has been reported before.9 However, the clinical significance of this finding remains undetermined. Accelerated idioventricular rhythm has been identified to be a non-specific marker for reperfusion after MI, but previous studies have found no prognostic impact on the clinical course.3 Usually, AIVR in patients with MI develops at the time of reperfusion.4 The proposed mechanism is abnormal automaticity which affects Ca2+-dependent slow diastolic depolarization.10 Remarkably, in our case, AIVR was documented relatively late after MI. Although the nature of AIVR is considered to be benign, there is also limited evidence that AIVR is associated with higher occurrence of ventricular tachycardia in the acute phase of MI.11 Possible explanations for the late occurrence of AIVR in our case may be AV nodal dysfunction due to ischaemic disturbances during the healing phase following MI or AV nodal alteration by neurocardiac dysfunction with enhanced vagal tone. However, there were no ECG recordings in the time interval between discharge and re-admission, so AIVR might have occurred at any time before re-admission. Additionally, drug-related bradycardia could have been a further culprit in this case, since the patient was treated with beta-blocker. As the patient was treated with ticagrelor, adverse side effects of this drug may also explain the late occurrence.12 Eventually, a critical combination of the described mechanisms might be a plausible explanation for the observed phenomenon in our patient.
Anteroseptal infarction complicated by BBB has previously been identified as a predictor of late in-hospital VF with an incidence rate of 36%.13 Involvement of the bundle branches could possibly lead to unstable re-entrant circuits in the His–Purkinje system.13 In line with these results, another case report described a patient who developed ABBB after MI.14 After implantation of a permanent pacemaker, the patient died suddenly. The authors raised suspicion that in the presence of a functional pacemaker, sudden cardiac death was rather due to ventricular tachyarrhythmia; however, telemetry data were not available in this case. Anterior MI accompanied by RBBB at presentation and new BBB (including LBBB) early after reperfusion has also been found as predictor of high 30-day post-MI mortality.15 Although not observed in the present case, bradycardia-induced VF could also occur in the presence of ABBB leading to complete heart block. Changes in ventricular activation increase the heterogeneity of repolarization, which might create a substrate for sustained polymorphic ventricular arrhythmia. Furthermore, prolonged repolarization secondary to an abrupt reduction in heart rate with complete heart block could be a potential mechanism for bradycardia induced VF, but the QT-interval was not prolonged in our case.
There are at least two explanations for ABBB in our case: at first, ischaemia/reperfusion could have initiated an ectopic focus with abnormal automaticity within the left bundle branch (LBB) distal to the site of conduction block. At second, one study analysing the electrophysiology of ABBB suggested that ABBB only arises if a novel BBB emerges and is superimposed on a pre-existing incomplete block of the contralateral bundle branch.6 As a precondition, the pre-existing contralateral BBB would have to exhibit residual conduction, despite showing all the criteria for complete BBB in the surface ECG.6 Applied to our case, during normal SR with LBBB, depolarization may have proceeded via both bundle branches. Accelerated idioventricular rhythm could than have suddenly been initiated by a focus within the bundle of His, which is supported by the short RP interval during AIVR. In this setting, the right bundle branch (RBB) may still have been refractory resulting in conduction via the LBB. Thus, as a precondition, conduction velocity in the RBB has to be faster than the LBB, but the refractory time has to be longer in the RBB.
We have found no other reports on the occurrence of AIVR and ABBB late after MI and thus - at first glance - seems to be an unusual and rare finding. However, to become aware of this constellation, there would have to be an uninterrupted in-hospital ECG monitoring exceeding the period of 3 days currently recommended by the guidelines.16 Even if prolonged in-hospital monitoring was practical, currently available monitoring algorithms would not detect norm frequent AIVR or ABBB since monitor annotation is triggered by bradycardia or tachycardia pre-settings. Thus, the constellation described in our case may be much more frequent than reported.
Due to the almost fatal course in our case, it should be discussed how to protect these patients in the early to intermediate phase after MI. One option could be to combine pacemaker implantation with an ICD-system or at least with a wearable cardioverter-defibrillator.
Nevertheless, our case should serve to sensitize physicians to not only base their risk stratification on tachycardic or bradycardic events but to scrutinize in and out of hospital ECGs after MI for AIVR with ABBB.
Lead author biography
Markus Bettin is a graduate of the University of Duisburg-Essen, Germany in 2012. He began his clinical education at the Clinic for Electrophysiology, University Hospital of Münster, Germany. Currently, he is an interventional cardiac electrophysiologist at Schuechtermann-Clinic, Bad Rothenfelde, Germany.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Acknowledgements
We would like to thank Dr Johannes Amberger and Dr Wolfgang Kranig for their contribution to this Case Report and their critical review of the manuscript.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: M.B. is supported by a fellowship of Boston Scientific Inc. All other authors declared no conflict of interest.





Comments