-
PDF
- Split View
-
Views
-
Cite
Cite
Vikas Reddy Maddali, Srikar Miryala, Yagna Sreekanth Bellamkonda, Praveen Nagula, Cardiac tamponade due to primary hypothyroidism: acute management and approach to prevent recurrence—a case report, European Heart Journal - Case Reports, Volume 4, Issue 3, June 2020, Pages 1–5, https://doi.org/10.1093/ehjcr/ytaa071
Close - Share Icon Share
Abstract
Hypothyroidism is a common endocrine disorder resulting from deficiency of thyroid hormone, with iodine deficiency remains the foremost cause. It is more common in women with increasing incidence in the elderly. The manifestations of hypothyroidism results from the hypometabolism in the body at cellular level and affects all organs. Although there can be an incidental diagnosis of the disorder, the presentation with cardiac signs and symptoms is rare. We report a case of primary hypothyroidism with dysmorphic features manifesting as massive pericardial effusion with cardiac tamponade at presentation.
A female aged 20 years presented with lethargy, constipation, and dyspnoea of 6 months duration. On examination, she was short-statured and had dysmorphic features with hypotension, raised jugular venous pressure (JVP), muffled heart sounds, and thyroid stimulating hormone >100 uIU/mL. Chest X-ray showed cardiomegaly and 2DEcho confirmed cardiac tamponade for which emergency pericardiocentesis was done.
Cardiovascular manifestations in hypothyroidism are dyspnoea and decreased exercise tolerance. Bradycardia, diastolic hypertension, cardiomegaly, and non-pitting or pitting peripheral oedema may be seen on physical examination. Mild pericardial effusion is common and generally asymptomatic. Massive pericardial effusion being manifested at presentation primarily as a sign of hypothyroidism is rare. A few cases have been mentioned in the literature in India and western population. Rarely, hypothyroidism presents with massive pericardial effusion resulting in cardiac tamponade as in our case.
Hypothyroidism is a common endocrine disorder resulting from deficiency of thyroid hormone, with iodine deficiency remains the foremost cause.
Pericardial effusion in overt hypothyroidism is common (incidence 3–6%), but cardiac tamponade and pretamponade as a presentation in newly diagnosed hypothyroidism is rare.
Differential diagnosis includes secondary hypothyroidism, hypopituitarism, vitamin D deficiency, and hypophosphataemia.
Introduction
Hypothroidism, characterized by elevated level of serum thyroid stimulating hormone (TSH) with lower or normal free thyroxine (fT4), is predominant worldwide, particularly in iodine deficient regions.1 Pericardial effusion in overt hypothyroidism is common (incidence 3–6%), but cardiac tamponade and pretamponade as a presentation in newly diagnosed hypothyroidism is rare. For patients diagnosed with cardiac tamponade without sinus tachycardia, hypothyroidism should be suspected.2 Here, we report an uncommon case of primary hypothyroidism with cardiac tamponade.
Timeline
| 10 June 2019 | Admitted with New York Heart Association (NYHA) Class IV dyspnoea, hypotension, elevated JVP, and muffled heart sounds with history of hypothyroidism [thyroid stimulating hormone (TSH) >100 uIU/mL)] on irregular treatment. |
| On the day of admission | Chest X-ray showed cardiomegaly. |
Electrocardiogram showed low voltage complexes with electrical alternans:
| |
| 1 day later |
|
| 2 days later |
|
| 3 days later | She was discharged with Tab.Levothyroxine 75 µg and was kept on follow-up. |
| 3 months later (follow-up) | Patient remained asymptomatic with TSH of 20 uIU/mL. |
| 10 June 2019 | Admitted with New York Heart Association (NYHA) Class IV dyspnoea, hypotension, elevated JVP, and muffled heart sounds with history of hypothyroidism [thyroid stimulating hormone (TSH) >100 uIU/mL)] on irregular treatment. |
| On the day of admission | Chest X-ray showed cardiomegaly. |
Electrocardiogram showed low voltage complexes with electrical alternans:
| |
| 1 day later |
|
| 2 days later |
|
| 3 days later | She was discharged with Tab.Levothyroxine 75 µg and was kept on follow-up. |
| 3 months later (follow-up) | Patient remained asymptomatic with TSH of 20 uIU/mL. |
| 10 June 2019 | Admitted with New York Heart Association (NYHA) Class IV dyspnoea, hypotension, elevated JVP, and muffled heart sounds with history of hypothyroidism [thyroid stimulating hormone (TSH) >100 uIU/mL)] on irregular treatment. |
| On the day of admission | Chest X-ray showed cardiomegaly. |
Electrocardiogram showed low voltage complexes with electrical alternans:
| |
| 1 day later |
|
| 2 days later |
|
| 3 days later | She was discharged with Tab.Levothyroxine 75 µg and was kept on follow-up. |
| 3 months later (follow-up) | Patient remained asymptomatic with TSH of 20 uIU/mL. |
| 10 June 2019 | Admitted with New York Heart Association (NYHA) Class IV dyspnoea, hypotension, elevated JVP, and muffled heart sounds with history of hypothyroidism [thyroid stimulating hormone (TSH) >100 uIU/mL)] on irregular treatment. |
| On the day of admission | Chest X-ray showed cardiomegaly. |
Electrocardiogram showed low voltage complexes with electrical alternans:
| |
| 1 day later |
|
| 2 days later |
|
| 3 days later | She was discharged with Tab.Levothyroxine 75 µg and was kept on follow-up. |
| 3 months later (follow-up) | Patient remained asymptomatic with TSH of 20 uIU/mL. |
Case presentation
A 20-year female presented with complaints of dyspnoea of 6 months duration. Dyspnoea progressed from New York Heart Association Class II to Class IV over 1 month prior to her presentation. She had a history of lethargy and constipation for which she consulted a primary physician and a diagnosis of primary hypothyroidism has been made. Levothyroxine 50 µg was prescribed to her, but she was non-compliant. Her prenatal and perinatal period was uneventful. She is the youngest of her four siblings. Her eldest sister was also diagnosed as having hypothyroidism and is on Levothyroxine 25 µg. Attainment of menarche was at 14 years, and the frequency of menstrual cycles were irregular.
On examination, she was conscious, coherent, obeying verbal commands. Her weight was 22 kg and height was 130 cm with a body mass index of 13 kg/m2. She had coarse, dry skin, hoarseness of voice, proportional skeletal immaturity, cold peripheral extremities, hypotonia, alopecia, and absence of secondary sexual characters. Extraoral examination revealed a euryprosopic facial form, with puffiness of the face and periorbital swelling, with a widened nasal bridge. The patient was leptoprosopic (Facial index = 92%) and dolichocephalic (Cephalic index =72.9%) (Figure 1). Intraoral examination revealed good oral hygiene with mixed dentition and multiple retained deciduous teeth.
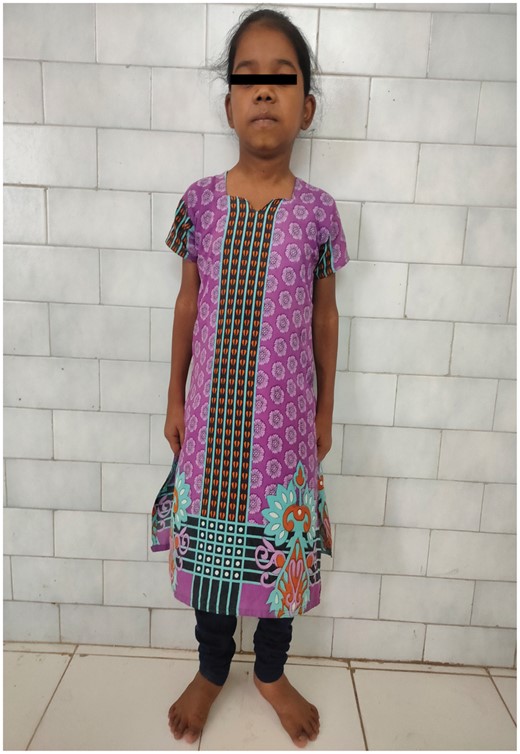
Euryprosopic facial form, Proportional skeletal immaturity with a widened nasal bridge.
Her pulse rate was 130/min with a blood pressure of 90/60 mmHg over the right arm. She had respiratory rate of 26/min, saturation at room air being 100%. On auscultation, distant heart sounds were heard. The electrocardiogram showed low voltage complexes and electrical alternans (Figure 2A). Chest X-ray showed massive cardiomegaly with normal lung fields and typical ‘water bottle’ configuration (Figure 3A). 2D echocardiography showed massive pericardial effusion with signs of cardiac tamponade including collapse of right ventricle free wall in diastole (Figure 4) with left ventricular ejection fraction of 58%. A provisional diagnosis of primary hypothyroidism presenting as massive pericardial effusion with cardiac tamponade was made.
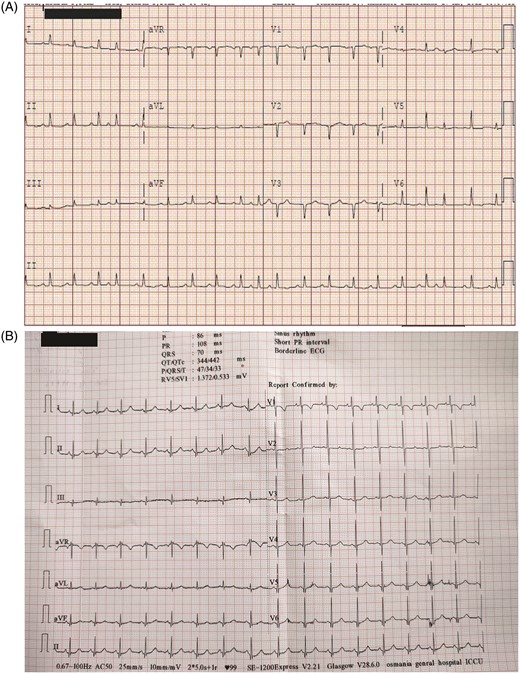
(A) Electrocardiogram showing low voltage complexes and electrical alternans. (B) Electrocardiogram post pericardiocentesis showing normal voltage complexes and resolution of electrical alternans.
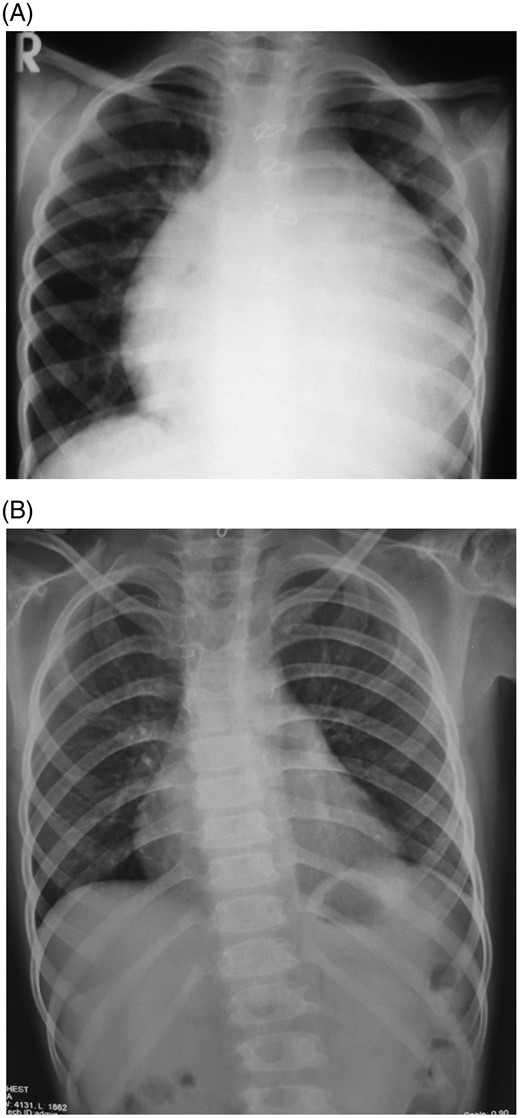
(A) Chest X-ray PA view showing massive cardiomegaly with normal lung fields and typical ‘water bottle’ configuration. (B) Chest X-ray post pericardiocentesis showing resolution of pericardial effusion.
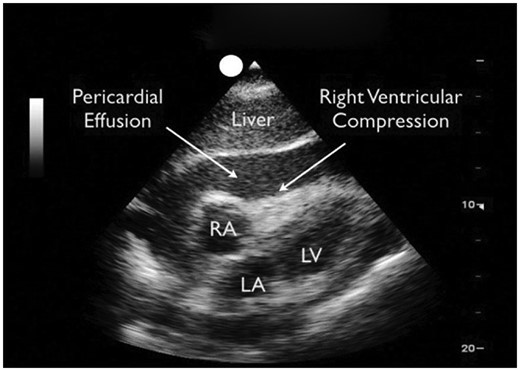
2D echocardiography sub costal view showing massive pericardial effusion and right ventricular diastolic collapse.
Patient was immediately taken to cardiac cath lab for pericardiocentesis after non-invasive monitoring [non-invasive blood pressure (NIBP), pulse oxymetry, and continuous electrocardiogram] was in place, patient was placed in 30° semi-reclining position. Under strict aseptic precautions, 18 G Teflon sheated needle introduced through sub-xiphoid approach. A 6-Fr dilator and introducer sheath passed over guide wire into pericardial space. The pericardial pressures recorded as 12 mmHg. Around 1000 mL of straw-coloured pericardial fluid was tapped. A pigtail catheter was placed in situ. Immediately after tapping the fluid, the patient showed dramatic recovery with pulse rate dropping to 70/min, blood pressure improving to 130/70 mmHg, and resolving dyspnoea. Electrocardiogram showed normal voltage complexes (Figure 2B). 2D echocardiogram showed immediate resolution of cardiac tamponade with mild pericardial effusion. On 2nd day, again 1000 mL of fluid was tapped, and pigtail catheter was removed the next day.
Other causes i.e., secondary hypothyroidism, hypopituitarism, vitamin D deficiency, and hypophosphataemia were ruled out by the appropriate investigations.
The haemogram showed a low haemoglobin level of 7.8 g% (normal 12.5–15.5 g%) with normocytic normochromic red blood cells on the peripheral smear. The levels of total triiodothyronine (T3) and thyroxine (T4) were significantly depressed at 0.12 ng/dL (normal 90–190 ng/dL) and 0.10 μg/dL (normal 5–12 μg/dL), respectively with thyroid stimulating hormone (TSH) of >100 uIU/mL (normal 0.35–5.5 uIU/mL). A low basal metabolic rate of 1040 kcal was recorded. Cholesterol and glucose levels were elevated to 200 mg/dL (normal 125–200 mg/dL) and 113 mg/dL (normal 70–99 mg/dL), respectively. The level of the growth hormone (2.4 ng/mL, normal 0.01–3.61 ng/mL), serum calcium (9.2 mg/dL normal 8.2–10.2 mg/dL), serum phosphorus (3.4 mg/dL normal 2.3–4.7 mg/dL), and alkaline phosphatase (57 U/L normal 50–120 U/L) were well within normal limits. Antinuclear antibodies were negative. The pericardial fluid was sent to laboratory for analysis and the report showed were as follows, proteins: 5.6 g/dL (normal 2.5–3 g/dL); sugar: 98 mg/dL (normal 60–80 mg/dL); acid fast bacilli (AFB)-negative; culture-negative for organisms; microscopy showed few mesothelial cells, cystic macrophages and occasional lymphocytes, and degenerated cells. So, the fluid was found to be an exudative.
Ultrasonography of the thyroid with a high frequency probe featured normal thyroid gland with normal size, echotexture, and normal vasculature.
She was discharged after 4 days of admission with Tab.Levothyroxine 75 µg/day and was kept on follow-up initially every month for 3 months to monitor for reaccumulation of pericardial fluid and thyroid dosage adjustments were made once in every 6–8 weeks as per TSH to prevent recurrence. Her follow-up investigations included anthropometry, freeT4, TSH, chest X-ray, 2DEcho with advice regarding dietary intake and avoidance of antithyroid drugs. After 3 months of follow-up, she was stable with no complaints of dyspnoea and repeat chest X-ray (Figure 3B) and 2DEcho showed no evidence of reaccumulation of pericardial fluid with TSH 20 uIU/mL.
Discussion
Hypothroidism, characterized by elevated level of serum TSH with lower or normal free thyroxine (fT4), is predominant worldwide, particularly in iodine deficient regions.1 Cardiovascular manifestations in hypothyroidism are dyspnoea and decreased exercise tolerance. Bradycardia, diastolic hypertension, muffled heart sounds, cardiomegaly, and non-pitting or pitting peripheral oedema may be seen on physical examination.3,4 Mild pericardial effusion is common in hypothyroid states and generally asymptomatic in nature. But massive pericardial effusion presenting primarily as a sign of hypothyroidism is rare.5–9
The manifestations of hypothyroidism results from the reduction in metabolic activity and deposition of glycosaminoglycans.10 Facial puffiness with periorbital oedema, proportional skeletal immaturity, cold extremities, coarse and dry skin, with sparse hair, hoarseness of voice, and muscular hypotonia are the findings commonly observed in hypothyroidism.
The pathophysiologic changes include increased systemic capillary permeability and disturbances in electrolyte metabolism. Other hypothesis includes extravasation of albumin and inadequate lymphatic drainage, accounts for the exudative nature of the accumulated fluid in this disorder. Because of the insidious and non-specific characteristics of the signs and symptoms of hypothyroidism along with rare occurrence of massive pericardial effusion in some patients, the possibility of hypothyroidism may be overlooked in the differential diagnosis of massive pericardial effusions.
Other differential diagnosis includes secondary hypothyroidism, hypopituitarism, vitamin D deficiency, and hypophosphataemia. The main stay of treatment of hypothyroidism causing pericardial effusion is simple thyroxine replacement, but in few exceptional cases when the patient presents with a tamponade mandates urgent pericardiocentesis as in our case where 2000 mL of pericardial fluid was aspirated and patient became asymptomatic.
The clinical resolution of pericardial effusion is satisfactory in majority of the hypothyroid patients with thyroxine replacement therapy, but it takes as long as months or years after the patient reach the euthyroid state. In our patient, at the end of 3 months of follow-up her thyroid status was well controlled and she had no symptoms related to cardiovascular system.
Although essentially treatment remains similar to other kinds of pericardial effusion with tamponade, identifying the primary disorder in a patient where other causes cannot be found out is very difficult. So, high degree of suspicion is necessary in which hypothyroidism is endemic so as to give long lasting cure for the patient from this reversible but uncommon entity.
Conclusions
Hypothyroidism is common problem in India. Though pericardial effusion and tamponade secondary to thyroid dysfunction are rare in western scenarios, in India we do get cases because of high burden of primary disease. As diagnostic and therapeutic modalities are sophisticated in nature, including primary hypothyroidism as a differential diagnosis of pericardial effusion and cardiac tamponade looks essential in India.
Informed consent
This case report has been done after obtaining informed consent from the patient.
Patient perspective
Most pressing query of our patient was whether she would suffer from recurrent cardiac tamponade in the near future. She was reassured about her cause of cardiac tamonade and its preventive nature and the importance of continuing Levothyroxine supplementation with regular follow-up’s for dose adjustment. She remained asymptomatic till date.
Lead author biography
Dr Vikas Reddy Maddali, MBBS is from Andhra Medical College, Visakhapatnam. He did post graduation from Guntur Medical College, Guntur; at present, he is pursuing second post graduation in Cardiology at Osmania Medical College, Hyderabad, Telangana, India.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.





Comments