-
Views
-
Cite
Cite
Philipp M Doldi, Kornelia Löw, Julius Steffen, Julius Fischer, Maximilian Tischmacher, Nike Knufinke, Thomas J Stocker, Hans Theiss, Konstantinos Rizas, Konstantin Stark, Christian Hagl, Michael Näbauer, Steffen Massberg, Jörg Hausleiter, Simon Deseive, Impact of dual atrioventricular valve disease on outcomes in patients undergoing transcatheter aortic valve replacement, European Heart Journal - Cardiovascular Imaging, 2025;, jeaf112, https://doi.org/10.1093/ehjci/jeaf112
Close - Share Icon Share
Abstract
Current guidelines provide no recommendations for the management of patients with dual atrioventricular valve regurgitation (DAVR) undergoing transcatheter aortic valve replacement (TAVR), and existing data on its clinical impact remain absent. Therefore, we aimed to provide detailed insights into the impact of DAVR on outcomes after TAVR, with the potential to refine clinical risk stratification tools and influence future management guidelines.
We retrospectively analysed 3491 consecutive patients who underwent TAVR between 2013 and 2021. DAVR was defined as the presence of both mitral regurgitation (MR) and tricuspid regurgitation (TR) ≥ 2+. Patients were divided into four groups based on echocardiography before TAVR: no/mild atrioventricular (AV) regurgitation, isolated MR ≥ 2+, isolated TR ≥ 2+, and DAVR. DAVR was present in 269 patients (7.7%) and was associated with significantly reduced 3-year survival (47.3%) compared with isolated MR (64.3%), isolated TR (54.4%), and no/mild AV regurgitation (73.0%, P < 0.001). Multivariate analysis identified DAVR as an independent predictor of 3-year mortality [hazard ratio (HR): 1.36, 95% confidence interval (CI), 1.1–1.8, P = 0.021]. A leading TR ≥ 3+ in DAVR patients was associated with a particularly poor prognosis (3-year survival: 27%). While an MR improvement following TAVR was linked to better survival (HR: 0.45, 95% CI, 0.30–0.69, P < 0.001), a TR improvement had no significant impact on survival (HR: 0.69, 95% CI: 0.45–1.05, P = 0.086). Notably, 54% of DAVR patients continued to experience significant exertional dyspnoea at follow-up (NYHA ≥ II).
These findings underscore the importance of recognizing DAVR as a high-risk condition in TAVR patients, highlighting the need for refined risk stratification tools and potential adjunctive therapeutic strategies to improve outcomes.
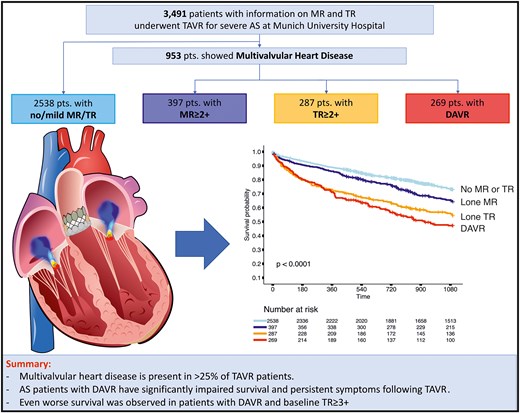
DAVR impacts outcome in patients with severe AS undergoing TAVR. This graphical abstract demonstrates an overview of the study cohort with atrioventricular valve regurgitation and corresponding Kaplan–Meier curves for each group (no/mild AV regurgitation, MR ≥ 2+, TR ≥ 2+, DAVR)




