-
PDF
- Split View
-
Views
-
Cite
Cite
Johannes Grand, Cecilie Fuglsbjerg, Britt Borregaard, Mette Kirstine Wagner, Astrid Rolin Kragh, Ditte Bekker-Jensen, Astrid Duus Mikkelsen, Jacob Eifer Møller, Heidi Glud, Christian Hassager, Selina Kikkenborg, Jesper Kjaergaard, Sex differences in symptoms of anxiety, depression, post-traumatic stress disorder, and cognitive function among survivors of out-of-hospital cardiac arrest, European Heart Journal. Acute Cardiovascular Care, Volume 12, Issue 11, November 2023, Pages 765–773, https://doi.org/10.1093/ehjacc/zuad093
Close - Share Icon Share
Abstract
Anxiety, depression, and post-traumatic stress disorder (PTSD) among out-of-hospital cardiac arrest (OHCA) survivors may impact long-term recovery. Coping and perception of symptoms may vary between sexes. The aim was to explore sex differences in psychological consequences following OHCA.
This was a prospective observational study of OHCA survivors who attended a structured 3-month follow-up. Symptoms of anxiety/depression were measured using the Hospital Anxiety and Depression Scale, range 0–21, with a cut-off score of ≥8 for significant symptoms; PTSD was measured with the PTSD Checklist for DSM-5 (PCL-5), range 0–80. A score of ≥33 indicated PTSD symptoms. Cognitive function was assessed by the Montreal Cognitive Assessment. From 2016 to 2021, 381 consecutive comatose OHCA survivors were invited. Of these, 288 patients (76%) participated in the follow-up visit [53 (18%) females out of 80 survivors and 235 (82%) males out of 300 alive at follow-up (78%)]. Significant symptoms of anxiety were present in 47 (20%) males and 19 (36%) females (P = 0.01). Significant symptoms of PTSD were present in 30% of males and 55% of females (P = 0.01). Adjusting for pre-specified covariates using multivariable logistic regression, female sex was significantly associated with anxiety [odds ratio (OR): 2.18, confidence interval (CI): 1.09–4.38, P = 0.03]. This difference was especially pronounced among young females (below median age, ORadjusted: 3.31, CI: 1.32–8.29, P = 0.01) compared with young males. No significant sex difference was observed for depression or cognitive function.
Symptoms of anxiety and PTSD are frequent in OHCA survivors, and female survivors report significantly more symptoms of anxiety and PTSD compared with males. In particular, young females were significantly more symptomatic than young males.
Introduction
Out-of-hospital cardiac arrest (OHCA) is a frequent cause of mortality and intensive care unit (ICU) admission, with an incidence in Europe of 40–80 patients per 100 000 person-years,1–3 and in-hospital mortality exceeding 30% in patients comatose on admission.4,5 The primary anoxic insult occurs during arrest, while subsequently compromised oxygen delivery and reperfusion injury to the brain potentially worsen brain injury.6 OHCA survivors, who are discharged alive, show a spectrum of neurological, cognitive, and emotional impairments.3,7,8 The level of care after hospital discharge is, among other factors, dependent on whether the survivor has a good neurological outcome, meaning the ability to attend to one’s own bodily needs and be independent.9 However, increasing attention has been put towards subclinical cognitive and emotional impairments, which is not always apparent to clinicians.8,10 Most impairments are mild to moderate, and some survivors recover cognitively and emotionally during the first 3 months after cardiac arrest.9 However, 25–50% of OHCA survivors still show signs of cognitive impairments after 3 months.9 The realization of the near-fatal event often comes in the aftermath, and anxiety, depression, and post-traumatic stress disorder (PTSD) are common consequences.11 Thus, the assessment of physical and non-physical impairments before hospital discharge can help identify rehabilitation needs.3 Cognitive impairments are dynamic, and systematic 3-month follow-up after hospital discharge is recommended by guidelines.3 Identifying high-risk populations may aid in targeting specialized follow-up and rehabilitation for those who need it the most. Female sex has been reported to be associated with significantly more anxiety compared with males after in-hospital cardiac arrest11–14 and in the general population.15 The aim of this study was to explore sex differences in symptoms of anxiety, depression, PTSD, cognitive function, and self-perceived health status after discharge among OHCA survivors hospitalized at a cardiovascular ICU.
Methods
Study design, setting, and patients
The study was a prospective observational cohort study investigating patients admitted to the cardiac ICU at the Heart Centre of Rigshospitalet, Copenhagen, Denmark, from April 2016 through November 2021. Patients were eligible if they were admitted to the department after OHCA of presumed cardiac origin, if they were adults, and if they were discharged alive from the hospital. Patients were included in this study 3 months after hospital discharge. Patients were excluded if they were too ill to participate. The local ethics committee approved the study protocol (H-17035667). In line with Danish legislation, written informed consent was obtained from the patients. The Danish Data Protection Agency approved the handling of data.
After discharge, survivors and their relatives were invited to a 3-month follow-up visit led by a nurse and/or physician at the intensive care department. Patients were contacted by letter, and if no response, the patients were contacted by telephone. In patients unable to transport themselves to the hospital, they were offered a visit in their home. Due to the COVID-19 pandemic restrictions, a proportion of the participants had longer follow-up times. We pre-specified a before/after COVID-19 sensitivity analysis. A structured test battery was given to each patient including cognitive testing and self-reported outcomes of mental health and health status. All tests have been validated previously.
Post-cardiac arrest care and haemodynamic measurements
All patients were admitted to the ICU and sedated, intubated, and mechanically ventilated with propofol and fentanyl titrated to attain a Richmond Agitation–Sedation Scale (RASS) score of −4. Active temperature control was initiated immediately after ICU admission, aiming at a target temperature of 36°C for 24 h, followed by rewarming by 0.5°C per hour. Emergency coronary angiography (CAG) was performed in all patients presenting with ST-segment elevations or if the attending physician found an indication for the procedure. Norepinephrine was the primary vasopressor and was used to treat hypotension. Guideline-directed multimodal prognostication strategies were used to evaluate neurological prognosis in patients not spontaneously awakening after tapering of sedation.3
Data collection
Sociodemographic and clinical characteristics
Pre-hospital data were systematically collected according to Utstein guidelines.16 Demographic characteristics (sex, age, and comorbidities) were collected from patient charts during hospitalization. Likewise, data on cardiac arrest characteristics were collected from the hospital electronic chart.
Neurological and cognitive function
Neurological function was measured by the cerebral performance category (CPC) scale by a trained nurse or study investigator at 3 months.17 A good neurological outcome was defined as a CPC of 1 or 2.
Cognitive screening with the Montreal Cognitive Assessment (MoCA) test was performed by a certified physician or nurse. The score ranges from 0 to 30, and cognitive impairment is defined as a score of 25 or below.18
Self-reported outcome measures
Hospital Anxiety and Depression Scale
Symptoms of anxiety and depression were evaluated with the Hospital Anxiety and Depression Scale (HADS).19 The HADS consists of two 7-item scales evaluating self-reported symptoms of anxiety (HADS-A) and symptoms of depression (HADS-D) for the past week. The highest possible score for each scale is 21, with higher scores representing more psychological distress. This standardized questionnaire is designed to assess mood disorders in non-psychiatric populations. The scale is used with a cut-off score of 8 or higher, indicating the presence of symptoms of anxiety and/or depression.19
EuroQol 5-Dimension 5-Level
EuroQol 5-Dimension 5-Level (EQ-5D-5L) (Danish version 2.1)20 is a self-reported questionnaire that consists of five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension has five response levels ranging from no problems to extreme problems. Individuals are asked to choose the response level that best describes their current emotional state. The response levels are then used to calculate a score for the anxiety/depression dimension. This variable is assessed as a binary variable according to values reported above or below the cut-off value for significant symptoms. The Visual Analogue Scale (VAS) of the EQ-5D-5L questionnaire is a 20 cm horizontal line marked with tick marks at each centimetre, with ‘best imaginable health state’ at one end and ‘worst imaginable health state’ at the other end. The respondent is asked to rate their own health state by drawing a vertical line on the scale between the two endpoints to indicate their own perceived health status. The VAS score ranges from 0 to 100. The VAS score provides a quantitative measure of the respondent’s overall health status.20
Post-traumatic stress disorder
The PTSD Checklist for DSM-5 (PCL-5) is a self-reported measure that assesses the presence and severity of symptoms of PTSD in adults. The PCL-5 is based on the criteria for PTSD outlined in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders. The PCL-5 consists of 20 items, each of which corresponds to a symptom of PTSD. The items are rated on a 5-point Likert scale, ranging from 0 (not at all) to 4 (extremely). The total score on the PCL-5 ranges from 0 to 80, with higher scores indicating greater severity of PTSD symptoms. A score of 33 or higher is typically used as a cut-off for indicating a probable PTSD diagnosis.21 The PCL-5 is used in clinical and research settings to assess PTSD symptoms, monitor treatment progress, and evaluate the effectiveness of interventions.21
Outcomes
The primary outcome was crude symptoms of anxiety and/or symptoms of depression assessed by the HADS score at 90 days or more after OHCA. Exploratory outcomes were (i) cognitive function, (ii) symptoms of traumatic distress, and (iii) self-reported health status and will be evaluated as both continuous variables and binary scores according to the acknowledged cut-off values.
Statistical analysis
Patients were grouped according to sex. Data were reported as mean and standard deviation (SD) or interquartile range (IQR) with 25 and 75 percentiles for continuous variables, as appropriate. Cognitive test data and self-reported outcome measures were calculated in two ways. First, the continuous value was used. Second, the specified cut-off level for each score was used to transform the result into a binary outcome. Differences in cognitive test data and self-reported outcome measures among women and men were carried out using Student’s t-tests for continuous outcomes, and for categorical outcomes, the Pearson χ2 test and Fisher’s exact test were used, as appropriate.
Multivariable logistic regression models were used to assess associations between sexes and outcomes. Pre-specified covariates were as follows: (i) age (above/below the median of the whole population), (ii) time from OHCA to return of spontaneous circulation (ROSC) in minutes, (iii) initial rhythm (shockable/non-shockable), (iv) body mass index (BMI), and (v) time from OHCA to date of follow-up. The lactate level at arrival was also pre-specified but removed from the analysis due to a high degree of collinearity with time to ROSC, thus compromising model assumptions.
Single-item missing data in any of the individual questionnaires (outcome measures) were not possible in the electronic survey. Missing data were considered insignificant if <5%. If larger proportions of missing data were present, a worst-case best-case analysis was done as a sensitivity analysis. Due to the two components of the primary outcome, the significance level was adjusted ad modum Bonferroni to a P-value of 0.025. All other outcomes are considered exploratory using a P-value of 0.05 to indicate statistical significance. Statistical analyses were performed using SAS statistical software version 9.4 (SAS Institute, Cary, NC, USA). Figures were created in GraphPad Prism version 8.0 (GraphPad Software, San Diego, CA, USA). All tests were two-tailed.
Results
During the inclusion period, 748 consecutive patients were screened. At 90 days, 381 (51%) were alive (Figure 1). Of this group, 288 (76%) participated in the structured follow-up. Baseline differences among participants and non-participants are found in Supplementary material online, Table S1. The groups were overall similar; however, more males than females attended follow-up, and acute CAG was more frequent in attendees. Of the 288 patients included, 235 (82%) were male and 53 (18%) were female.
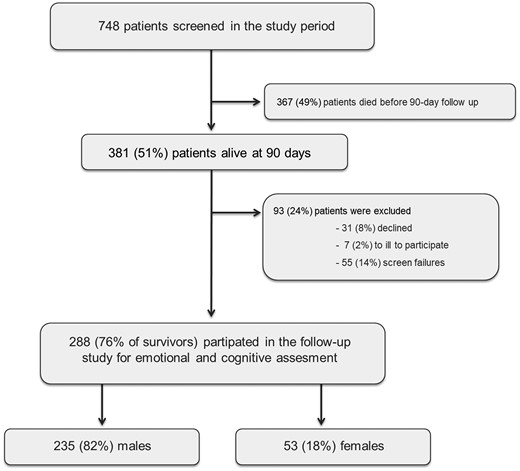
Included patients in the study. Screen failures are patients who were never invited to follow-up due to logistical reasons such as moving to another country or not returning the invite.
Mean age was 59 ± 13 years; 88% of cardiac arrests were witnessed by a bystander; cardiopulmonary resuscitation (CPR) was initiated before arrival of emergency medical services in 93%; the first rhythm was shockable in 88%; time from cardiac arrest to ROSC was median 15 (Q1–Q3: 10–21) minutes. Baseline characteristics among males and females are shown in Table 1. Females were significantly younger than males (52 ± 15 vs. 60 ± 15, P = 0.0006), and male patients had more often ischaemic heart disease and emergency CAG performed at arrival compared with females. All other baseline characteristics were not significantly different among males and females.
| . | Total population . | Male . | Female . | P-value . |
|---|---|---|---|---|
| . | n = 288 . | n = 235 (82%) . | n = 53 (18%) . | . |
| Demography: | ||||
| Age, year (±SD) | 59 ± 13 | 60 ± 12 | 52 ± 15 | 0.0006 |
| Pre-arrest comorbidities: | ||||
| Previous AMI, n (%) | 51 (18%) | 51 (22%) | 0 (0%) | 0.0009 |
| Congestive heart failure, n (%) | 30 (11%) | 28 (12%) | 2 (4%) | 0.19 |
| Hypertension, n (%) | 123 (43%) | 107 (46%) | 16 (32%) | 0.12 |
| Previous TCI/stroke, n (%) | 16 (6%) | 16 (7%) | 0 (0%) | 0.12 |
| Diabetes, n (%) | 30 (10%) | 28 (12%) | 2 (4%) | 0.08 |
| COPD, n (%) | 14 (5%) | 11 (5%) | 3 (6%) | 0.75 |
| Chronic kidney disease, n (%) | 8 (3%) | 8 (3%) | 0 (0%) | 0.35 |
| Atrial fibrillation, n (%) | 34 (12%) | 30 (13%) | 4 (8%) | 0.52 |
| Cardiac arrest characteristics: | ||||
| Witnessed arrest, n (%) | 251 (88%) | 203 (87%) | 48 (92%) | 0.30 |
| Bystander CPR, n (%) | 260 (93%) | 213 (93%) | 47 (94%) | 0.73 |
| Shockable primary rhythm, n (%) | 251 (88%) | 205 (88%) | 46 (88%) | 0.93 |
| Time to ROSC, min (Q1–Q3) | 15 (10–21) | 15 (10–20) | 14 (10–21) | 0.48 |
| Lactate at admission, mmol/L (Q1–Q3) | 4.3 (2.9–7.7) | 4.2 (2.6–7.0) | 4.6 (3.0–7.4) | 0.19 |
| Acute CAG, n (%) | 215 (89%) | 185 (92%) | 30 (79%) | 0.01 |
| PCI, n (%) | 96 (33%) | 84 (36%) | 12 (23%) | 0.06 |
| LVEF at hospital admission | 36 ± 14 | 36 ± 14 | 39 ± 14 | 0.24 |
| Time from cardiac arrest until follow-up date, days (Q1–Q3) | 97.5 (90–149) | 99 (90–145) | 92 (90–156) | 0.66 |
| . | Total population . | Male . | Female . | P-value . |
|---|---|---|---|---|
| . | n = 288 . | n = 235 (82%) . | n = 53 (18%) . | . |
| Demography: | ||||
| Age, year (±SD) | 59 ± 13 | 60 ± 12 | 52 ± 15 | 0.0006 |
| Pre-arrest comorbidities: | ||||
| Previous AMI, n (%) | 51 (18%) | 51 (22%) | 0 (0%) | 0.0009 |
| Congestive heart failure, n (%) | 30 (11%) | 28 (12%) | 2 (4%) | 0.19 |
| Hypertension, n (%) | 123 (43%) | 107 (46%) | 16 (32%) | 0.12 |
| Previous TCI/stroke, n (%) | 16 (6%) | 16 (7%) | 0 (0%) | 0.12 |
| Diabetes, n (%) | 30 (10%) | 28 (12%) | 2 (4%) | 0.08 |
| COPD, n (%) | 14 (5%) | 11 (5%) | 3 (6%) | 0.75 |
| Chronic kidney disease, n (%) | 8 (3%) | 8 (3%) | 0 (0%) | 0.35 |
| Atrial fibrillation, n (%) | 34 (12%) | 30 (13%) | 4 (8%) | 0.52 |
| Cardiac arrest characteristics: | ||||
| Witnessed arrest, n (%) | 251 (88%) | 203 (87%) | 48 (92%) | 0.30 |
| Bystander CPR, n (%) | 260 (93%) | 213 (93%) | 47 (94%) | 0.73 |
| Shockable primary rhythm, n (%) | 251 (88%) | 205 (88%) | 46 (88%) | 0.93 |
| Time to ROSC, min (Q1–Q3) | 15 (10–21) | 15 (10–20) | 14 (10–21) | 0.48 |
| Lactate at admission, mmol/L (Q1–Q3) | 4.3 (2.9–7.7) | 4.2 (2.6–7.0) | 4.6 (3.0–7.4) | 0.19 |
| Acute CAG, n (%) | 215 (89%) | 185 (92%) | 30 (79%) | 0.01 |
| PCI, n (%) | 96 (33%) | 84 (36%) | 12 (23%) | 0.06 |
| LVEF at hospital admission | 36 ± 14 | 36 ± 14 | 39 ± 14 | 0.24 |
| Time from cardiac arrest until follow-up date, days (Q1–Q3) | 97.5 (90–149) | 99 (90–145) | 92 (90–156) | 0.66 |
AMI, acute myocardial infarction; CAG, coronary angiography; COPD, chronic obstructive pulmonary disease; CPR, cardiopulmonary resuscitation; Q1–Q3, interquartile range; LVEF, left ventricular ejection fraction; n, number; PCI, percutaneous coronary intervention; ROSC, return of spontaneous circulation; SD, standard deviation; TCI, transitory cerebral ischaemia.
| . | Total population . | Male . | Female . | P-value . |
|---|---|---|---|---|
| . | n = 288 . | n = 235 (82%) . | n = 53 (18%) . | . |
| Demography: | ||||
| Age, year (±SD) | 59 ± 13 | 60 ± 12 | 52 ± 15 | 0.0006 |
| Pre-arrest comorbidities: | ||||
| Previous AMI, n (%) | 51 (18%) | 51 (22%) | 0 (0%) | 0.0009 |
| Congestive heart failure, n (%) | 30 (11%) | 28 (12%) | 2 (4%) | 0.19 |
| Hypertension, n (%) | 123 (43%) | 107 (46%) | 16 (32%) | 0.12 |
| Previous TCI/stroke, n (%) | 16 (6%) | 16 (7%) | 0 (0%) | 0.12 |
| Diabetes, n (%) | 30 (10%) | 28 (12%) | 2 (4%) | 0.08 |
| COPD, n (%) | 14 (5%) | 11 (5%) | 3 (6%) | 0.75 |
| Chronic kidney disease, n (%) | 8 (3%) | 8 (3%) | 0 (0%) | 0.35 |
| Atrial fibrillation, n (%) | 34 (12%) | 30 (13%) | 4 (8%) | 0.52 |
| Cardiac arrest characteristics: | ||||
| Witnessed arrest, n (%) | 251 (88%) | 203 (87%) | 48 (92%) | 0.30 |
| Bystander CPR, n (%) | 260 (93%) | 213 (93%) | 47 (94%) | 0.73 |
| Shockable primary rhythm, n (%) | 251 (88%) | 205 (88%) | 46 (88%) | 0.93 |
| Time to ROSC, min (Q1–Q3) | 15 (10–21) | 15 (10–20) | 14 (10–21) | 0.48 |
| Lactate at admission, mmol/L (Q1–Q3) | 4.3 (2.9–7.7) | 4.2 (2.6–7.0) | 4.6 (3.0–7.4) | 0.19 |
| Acute CAG, n (%) | 215 (89%) | 185 (92%) | 30 (79%) | 0.01 |
| PCI, n (%) | 96 (33%) | 84 (36%) | 12 (23%) | 0.06 |
| LVEF at hospital admission | 36 ± 14 | 36 ± 14 | 39 ± 14 | 0.24 |
| Time from cardiac arrest until follow-up date, days (Q1–Q3) | 97.5 (90–149) | 99 (90–145) | 92 (90–156) | 0.66 |
| . | Total population . | Male . | Female . | P-value . |
|---|---|---|---|---|
| . | n = 288 . | n = 235 (82%) . | n = 53 (18%) . | . |
| Demography: | ||||
| Age, year (±SD) | 59 ± 13 | 60 ± 12 | 52 ± 15 | 0.0006 |
| Pre-arrest comorbidities: | ||||
| Previous AMI, n (%) | 51 (18%) | 51 (22%) | 0 (0%) | 0.0009 |
| Congestive heart failure, n (%) | 30 (11%) | 28 (12%) | 2 (4%) | 0.19 |
| Hypertension, n (%) | 123 (43%) | 107 (46%) | 16 (32%) | 0.12 |
| Previous TCI/stroke, n (%) | 16 (6%) | 16 (7%) | 0 (0%) | 0.12 |
| Diabetes, n (%) | 30 (10%) | 28 (12%) | 2 (4%) | 0.08 |
| COPD, n (%) | 14 (5%) | 11 (5%) | 3 (6%) | 0.75 |
| Chronic kidney disease, n (%) | 8 (3%) | 8 (3%) | 0 (0%) | 0.35 |
| Atrial fibrillation, n (%) | 34 (12%) | 30 (13%) | 4 (8%) | 0.52 |
| Cardiac arrest characteristics: | ||||
| Witnessed arrest, n (%) | 251 (88%) | 203 (87%) | 48 (92%) | 0.30 |
| Bystander CPR, n (%) | 260 (93%) | 213 (93%) | 47 (94%) | 0.73 |
| Shockable primary rhythm, n (%) | 251 (88%) | 205 (88%) | 46 (88%) | 0.93 |
| Time to ROSC, min (Q1–Q3) | 15 (10–21) | 15 (10–20) | 14 (10–21) | 0.48 |
| Lactate at admission, mmol/L (Q1–Q3) | 4.3 (2.9–7.7) | 4.2 (2.6–7.0) | 4.6 (3.0–7.4) | 0.19 |
| Acute CAG, n (%) | 215 (89%) | 185 (92%) | 30 (79%) | 0.01 |
| PCI, n (%) | 96 (33%) | 84 (36%) | 12 (23%) | 0.06 |
| LVEF at hospital admission | 36 ± 14 | 36 ± 14 | 39 ± 14 | 0.24 |
| Time from cardiac arrest until follow-up date, days (Q1–Q3) | 97.5 (90–149) | 99 (90–145) | 92 (90–156) | 0.66 |
AMI, acute myocardial infarction; CAG, coronary angiography; COPD, chronic obstructive pulmonary disease; CPR, cardiopulmonary resuscitation; Q1–Q3, interquartile range; LVEF, left ventricular ejection fraction; n, number; PCI, percutaneous coronary intervention; ROSC, return of spontaneous circulation; SD, standard deviation; TCI, transitory cerebral ischaemia.
Supplementary material online, Table S2 shows differences among sexes for excluded patients. Hypertension is more prevalent in excluded females compared with excluded males, but overall, the findings were similar to the findings of Table 1, though numbers were smaller and missing data larger.
Crude differences in cognitive function and self-reported outcomes at follow-up
The score for HADS-A was significantly lower in males (4.5 ± 3.9) compared with females (6.1 ± 3.9) (P = 0.007). In addition, 47 (20%) males and 19 (36%) females fulfilled the criteria for significant anxiety (score above 8) (P = 0.01) (Figure 2). No sex difference was observed for HADS-D.
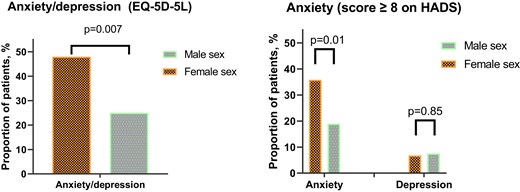
Proportion of males and females fulfilling the criteria for symptoms of anxiety and/or depression recorded on two different questionnaires, namely the Hospital Anxiety and Depression Scale and EuroQol 5-Dimension 5-Level.
Table 2 shows the association between sexes and symptoms of anxiety and depression. Female sex was significantly associated with anxiety [odds ratio (OR): 2.24 (1.17–4.27), P = 0.02] but not depression [OR: 1.12 (0.36–3.49), P = 0.85]. When adjusting for pre-defined covariates, the association between female sex and anxiety was significant in multivariable analysis [ORadjusted: 2.18 (1.09–4.38), P = 0.03].
| . | OR for anxiety (score ≥ 8 on HADS-A) (n = 272) . | OR for depression (score ≥ 8 on HADS-D) (n = 272) . | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | |
| Female sex | 2.24 (1.17–4.27) | 0.02 | 2.18 (1.09–4.38) | 0.03 | 1.12 (0.36–3.49) | 0.85 | 0.98 (0.26–3.67) | 0.31 |
| Age at arrest/above 55 years | 0.64 (0.39–1.12) | 0.12 | 0.71 (0.39–1.28) | 0.25 | 0.83 (0.33–2.07) | 0.69 | 0.84 (0.32–2.19) | 0.72 |
| BMI | 0.99 (0.92–1.06) | 0.73 | 0.95 (0.89–1.02) | 0.13 | 0.98 (0.89–1.09) | 0.74 | 0.95 (0.85–1.07) | 0.39 |
| Time to ROSC, min | 0.99 (0.97–1.02) | 0.59 | 0.99 (0.97–1.03) | 0.89 | 1.00 (0.96–1.04) | 0.89 | 1.01 (0.96–1.04) | 0.81 |
| Shockable primary rhythm, yes/no | 0.97 (0.42–2.26) | 0.77 | 0.83 (0.365–1.99) | 0.68 | 0.75 (0.21–2.69) | 0.66 | 0.82 (0.22–3.14) | 0.77 |
| Time from OHCA to follow-up/10 days | 0.99 (0.98–1.02) | 0.75 | 0.99 (0.98–1.02) | 0.91 | 1.03 (1.01–1.06) | 0.01 | 1.03 (1.01–1.06) | 0.02 |
| . | OR for anxiety (score ≥ 8 on HADS-A) (n = 272) . | OR for depression (score ≥ 8 on HADS-D) (n = 272) . | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | |
| Female sex | 2.24 (1.17–4.27) | 0.02 | 2.18 (1.09–4.38) | 0.03 | 1.12 (0.36–3.49) | 0.85 | 0.98 (0.26–3.67) | 0.31 |
| Age at arrest/above 55 years | 0.64 (0.39–1.12) | 0.12 | 0.71 (0.39–1.28) | 0.25 | 0.83 (0.33–2.07) | 0.69 | 0.84 (0.32–2.19) | 0.72 |
| BMI | 0.99 (0.92–1.06) | 0.73 | 0.95 (0.89–1.02) | 0.13 | 0.98 (0.89–1.09) | 0.74 | 0.95 (0.85–1.07) | 0.39 |
| Time to ROSC, min | 0.99 (0.97–1.02) | 0.59 | 0.99 (0.97–1.03) | 0.89 | 1.00 (0.96–1.04) | 0.89 | 1.01 (0.96–1.04) | 0.81 |
| Shockable primary rhythm, yes/no | 0.97 (0.42–2.26) | 0.77 | 0.83 (0.365–1.99) | 0.68 | 0.75 (0.21–2.69) | 0.66 | 0.82 (0.22–3.14) | 0.77 |
| Time from OHCA to follow-up/10 days | 0.99 (0.98–1.02) | 0.75 | 0.99 (0.98–1.02) | 0.91 | 1.03 (1.01–1.06) | 0.01 | 1.03 (1.01–1.06) | 0.02 |
CL, confidence limit; OR, odds ratio; ROSC, return of spontaneous circulation; OHCA, out-of-hospital cardiac arrest; BMI, body mass index; min, minutes; HADS, Hospital Anxiety and Depression Scale.
| . | OR for anxiety (score ≥ 8 on HADS-A) (n = 272) . | OR for depression (score ≥ 8 on HADS-D) (n = 272) . | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | |
| Female sex | 2.24 (1.17–4.27) | 0.02 | 2.18 (1.09–4.38) | 0.03 | 1.12 (0.36–3.49) | 0.85 | 0.98 (0.26–3.67) | 0.31 |
| Age at arrest/above 55 years | 0.64 (0.39–1.12) | 0.12 | 0.71 (0.39–1.28) | 0.25 | 0.83 (0.33–2.07) | 0.69 | 0.84 (0.32–2.19) | 0.72 |
| BMI | 0.99 (0.92–1.06) | 0.73 | 0.95 (0.89–1.02) | 0.13 | 0.98 (0.89–1.09) | 0.74 | 0.95 (0.85–1.07) | 0.39 |
| Time to ROSC, min | 0.99 (0.97–1.02) | 0.59 | 0.99 (0.97–1.03) | 0.89 | 1.00 (0.96–1.04) | 0.89 | 1.01 (0.96–1.04) | 0.81 |
| Shockable primary rhythm, yes/no | 0.97 (0.42–2.26) | 0.77 | 0.83 (0.365–1.99) | 0.68 | 0.75 (0.21–2.69) | 0.66 | 0.82 (0.22–3.14) | 0.77 |
| Time from OHCA to follow-up/10 days | 0.99 (0.98–1.02) | 0.75 | 0.99 (0.98–1.02) | 0.91 | 1.03 (1.01–1.06) | 0.01 | 1.03 (1.01–1.06) | 0.02 |
| . | OR for anxiety (score ≥ 8 on HADS-A) (n = 272) . | OR for depression (score ≥ 8 on HADS-D) (n = 272) . | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | Univariable OR (95% CL) . | P-value . | Multivariable* OR (95% CL) . | P-value . | |
| Female sex | 2.24 (1.17–4.27) | 0.02 | 2.18 (1.09–4.38) | 0.03 | 1.12 (0.36–3.49) | 0.85 | 0.98 (0.26–3.67) | 0.31 |
| Age at arrest/above 55 years | 0.64 (0.39–1.12) | 0.12 | 0.71 (0.39–1.28) | 0.25 | 0.83 (0.33–2.07) | 0.69 | 0.84 (0.32–2.19) | 0.72 |
| BMI | 0.99 (0.92–1.06) | 0.73 | 0.95 (0.89–1.02) | 0.13 | 0.98 (0.89–1.09) | 0.74 | 0.95 (0.85–1.07) | 0.39 |
| Time to ROSC, min | 0.99 (0.97–1.02) | 0.59 | 0.99 (0.97–1.03) | 0.89 | 1.00 (0.96–1.04) | 0.89 | 1.01 (0.96–1.04) | 0.81 |
| Shockable primary rhythm, yes/no | 0.97 (0.42–2.26) | 0.77 | 0.83 (0.365–1.99) | 0.68 | 0.75 (0.21–2.69) | 0.66 | 0.82 (0.22–3.14) | 0.77 |
| Time from OHCA to follow-up/10 days | 0.99 (0.98–1.02) | 0.75 | 0.99 (0.98–1.02) | 0.91 | 1.03 (1.01–1.06) | 0.01 | 1.03 (1.01–1.06) | 0.02 |
CL, confidence limit; OR, odds ratio; ROSC, return of spontaneous circulation; OHCA, out-of-hospital cardiac arrest; BMI, body mass index; min, minutes; HADS, Hospital Anxiety and Depression Scale.
Adding known ischaemic heart disease to the multivariable model as a sensitivity analysis did not change this association significantly [ORadjusted: 2.42 (1.78–4.99), P = 0.02]. Ischaemic heart disease was not associated with anxiety (P = 0.17).
No other covariates were associated with symptoms of anxiety in multivariable analysis. Time from OHCA to follow-up was the only covariate associated with symptoms of depression.
Stratifying the population according to sex and age above or below the median identified women above the median age of 55 as the group with the highest risk of significant anxiety: young women, 43%; women and older than the median, 28%; young males, 21%; and males and older than the median, 19% (see Supplementary material online, Figure S1).
Adjusting for confounders, being a young female was significantly associated with more symptoms of anxiety [ORadjusted = 3.31 (1.32–8.29), P = 0.01] compared with young males.
Supplementary material online, Figure S2 illustrates the association between age and symptoms of anxiety stratified by sex.
The post-traumatic stress score was significantly lower in males (29 ± 9) than in females (37 ± 16) (P = 0.02) (Table 3). In males, 31% had a PCL-5 score of at least 33 compared with 61% in females (P = 0.01) (Figure 3). Female sex was significantly associated with PTSD defined as a PCL-5 score of 33 or more [OR: 3.46 (1.22–9.79), P = 0.02]; however, this association was not significant in the multivariable model [ORadjusted: 1.89 (0.61–6.43), P = 0.25].
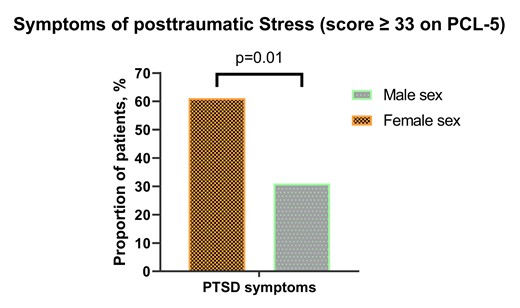
Proportion of males and females fulfilling the criteria for post-traumatic stress disorder on the Post-traumatic Stress Disorder Checklist for DSM-5 questionnaire.
Differences in patient-reported outcomes among males and females at the 3-month follow-up after out-of-hospital cardiac arrest with coma and intensive care treatment
| . | Male . | Female . | P-value . |
|---|---|---|---|
| . | n = 235 (82%) . | n = 53 (18%) . | . |
| Neurological outcome at 3 months | |||
| Cerebral performance category | |||
| CPC 1, n (%) | 214 (91%) | 49 (92%) | 0.92 |
| CPC 2—all patients, n (%) | 17 (7%) | 3 (6%) | 0.81 |
| CPC 3—all patients, n (%) | 3 (1%) | 1 (2%) | 0.66 |
| CPC 4—all patients, n (%) | 0 (0%) | 0 (0%) | — |
| Cognitive function at 3 months | |||
| Impaired cognitive function (MoCA < 26), n (%) | 74 (31%), missing = 13% | 19 (36%), missing = 18% | 0.36 |
| EQ-5D-5L | |||
| Perceived health VAS, mean (±SD) | 75 ± 18 | 68 ± 19 | 0.03 |
| Hospital Anxiety and Depression Scale | |||
| Depression, mean (±SD) | 2.6 ± 3.2 | 3.3 ± 3.4 | 0.06 |
| Anxiety, mean (±SD) | 4.5 ± 3.9 | 6.1 ± 3.9 | 0.007 |
| Post-traumatic stress disorder (PCL-5) | |||
| Mean (±SD) | 29 ± 9 | 37 ± 16 | 0.02 |
| . | Male . | Female . | P-value . |
|---|---|---|---|
| . | n = 235 (82%) . | n = 53 (18%) . | . |
| Neurological outcome at 3 months | |||
| Cerebral performance category | |||
| CPC 1, n (%) | 214 (91%) | 49 (92%) | 0.92 |
| CPC 2—all patients, n (%) | 17 (7%) | 3 (6%) | 0.81 |
| CPC 3—all patients, n (%) | 3 (1%) | 1 (2%) | 0.66 |
| CPC 4—all patients, n (%) | 0 (0%) | 0 (0%) | — |
| Cognitive function at 3 months | |||
| Impaired cognitive function (MoCA < 26), n (%) | 74 (31%), missing = 13% | 19 (36%), missing = 18% | 0.36 |
| EQ-5D-5L | |||
| Perceived health VAS, mean (±SD) | 75 ± 18 | 68 ± 19 | 0.03 |
| Hospital Anxiety and Depression Scale | |||
| Depression, mean (±SD) | 2.6 ± 3.2 | 3.3 ± 3.4 | 0.06 |
| Anxiety, mean (±SD) | 4.5 ± 3.9 | 6.1 ± 3.9 | 0.007 |
| Post-traumatic stress disorder (PCL-5) | |||
| Mean (±SD) | 29 ± 9 | 37 ± 16 | 0.02 |
MoCA, Montreal Cognitive Assessment; CPC, cerebral performance category; EQ-5D-5L, EuroQol 5-Dimension 5-Level; VAS, Visual Analogue Scale; SD, standard deviation; PCL-5, Post-traumatic Stress Disorder Checklist for DSM-5.
Differences in patient-reported outcomes among males and females at the 3-month follow-up after out-of-hospital cardiac arrest with coma and intensive care treatment
| . | Male . | Female . | P-value . |
|---|---|---|---|
| . | n = 235 (82%) . | n = 53 (18%) . | . |
| Neurological outcome at 3 months | |||
| Cerebral performance category | |||
| CPC 1, n (%) | 214 (91%) | 49 (92%) | 0.92 |
| CPC 2—all patients, n (%) | 17 (7%) | 3 (6%) | 0.81 |
| CPC 3—all patients, n (%) | 3 (1%) | 1 (2%) | 0.66 |
| CPC 4—all patients, n (%) | 0 (0%) | 0 (0%) | — |
| Cognitive function at 3 months | |||
| Impaired cognitive function (MoCA < 26), n (%) | 74 (31%), missing = 13% | 19 (36%), missing = 18% | 0.36 |
| EQ-5D-5L | |||
| Perceived health VAS, mean (±SD) | 75 ± 18 | 68 ± 19 | 0.03 |
| Hospital Anxiety and Depression Scale | |||
| Depression, mean (±SD) | 2.6 ± 3.2 | 3.3 ± 3.4 | 0.06 |
| Anxiety, mean (±SD) | 4.5 ± 3.9 | 6.1 ± 3.9 | 0.007 |
| Post-traumatic stress disorder (PCL-5) | |||
| Mean (±SD) | 29 ± 9 | 37 ± 16 | 0.02 |
| . | Male . | Female . | P-value . |
|---|---|---|---|
| . | n = 235 (82%) . | n = 53 (18%) . | . |
| Neurological outcome at 3 months | |||
| Cerebral performance category | |||
| CPC 1, n (%) | 214 (91%) | 49 (92%) | 0.92 |
| CPC 2—all patients, n (%) | 17 (7%) | 3 (6%) | 0.81 |
| CPC 3—all patients, n (%) | 3 (1%) | 1 (2%) | 0.66 |
| CPC 4—all patients, n (%) | 0 (0%) | 0 (0%) | — |
| Cognitive function at 3 months | |||
| Impaired cognitive function (MoCA < 26), n (%) | 74 (31%), missing = 13% | 19 (36%), missing = 18% | 0.36 |
| EQ-5D-5L | |||
| Perceived health VAS, mean (±SD) | 75 ± 18 | 68 ± 19 | 0.03 |
| Hospital Anxiety and Depression Scale | |||
| Depression, mean (±SD) | 2.6 ± 3.2 | 3.3 ± 3.4 | 0.06 |
| Anxiety, mean (±SD) | 4.5 ± 3.9 | 6.1 ± 3.9 | 0.007 |
| Post-traumatic stress disorder (PCL-5) | |||
| Mean (±SD) | 29 ± 9 | 37 ± 16 | 0.02 |
MoCA, Montreal Cognitive Assessment; CPC, cerebral performance category; EQ-5D-5L, EuroQol 5-Dimension 5-Level; VAS, Visual Analogue Scale; SD, standard deviation; PCL-5, Post-traumatic Stress Disorder Checklist for DSM-5.
At follow-up, 214 (91%) males and 49 (89%) females had a CPC of 1, whereas 17 (7%) and 3 (6%) had a CPC of 2, respectively. Only four patients in this cohort had a CPC > 2. No differences in CPC scores were found among sexes (Table 3). Likewise, cognitive function measured by the MoCA test was similar among sexes (P = 0.36). There was overall 14% missing for this variable, with a comparable number among sexes. Worst/best-case analysis did not change this result significantly.
Perceived health measured by EQ-5D-5L VAS was 75 ± 18 for males and 68 ± 19 for females (P = 0.03). The anxiety/depression dimension for EQ-5D-5L was significantly higher for females (Figure 2).
Correlation among anxiety symptoms and other variables
Symptoms of anxiety correlated inversely with age. The correlation was weak but statistically significant (r = 0.14, P = 0.03) (Supplementary Figure 2). Also, self-reported health correlated inversely with symptoms of anxiety (r = 0.3, P = 0.0002). Anxiety symptoms from the HADS questionnaire correlated significantly with symptoms of anxiety/depression from the EQ-5D-5L questionnaire (r = 0.52, P < 0.0001).
After COVID-19 (1 March 2020), 34% of the study population attended follow-up. Patients attending follow-up after COVID-19 were not significantly different compared with those attending follow-up before with regard to symptoms of anxiety or depression, and follow-up after COVID-19 did not significantly interact with the relationship between anxiety and sex.
Discussion
In this study, we investigated emotional sequelae and cognitive impairments based on comprehensive follow-up after OHCA with persistent coma and need for intensive care at a specialized cardiac ICU. Symptoms of anxiety were common and present in a third of patients overall, while symptoms of PTSD were present in almost half of responders. The main finding was that females had a significantly higher burden of anxiety and PTSD compared with males. At baseline, males had a higher age and more comorbidities. An additional analysis illustrated that higher anxiety was associated with younger age and a lower degree of self-reported health. Females in this cohort were younger, and young females had by far the highest risk of experiencing symptomatic anxiety.
In a recent cross-sectional survey of 176 cardiac arrest survivors (35 females) by Wagner et al.,22 patients participated in the immediate post-intensive care period before hospital discharge. This study found that female survivors of cardiac arrest reported worse psychological distress and anxiety burdens in the immediate recovery period after resuscitation. The current study confirmed these findings at the 3-month follow-up in a larger sample size of patients admitted and discharged from a specialized cardiac ICU. In addition, a recent study by Joshi et al.14 included survivors from OHCA from 2016 to 2019 through a registry. In this study, 20% reported symptoms of anxiety, and 15% reported symptoms of depression up to 4 years after the event. The authors concluded that early screening and individualized interventions are necessary to aid OHCA survivors adapt to the new situation. In the present study, we found a slightly higher prevalence of anxiety, which is possibly explained by the shorter follow-up period after OHCA.
Our findings of younger age being a factor associated with worse outcomes support the findings in a Swedish study by Viktorisson et al.23 In 94 survivors of cardiac arrest, approximately half of the participants reported reduced well-being, and young age was the only factor significantly correlated to this outcome (P = 0.02). Females reported higher scores in HADS (P = 0.001) and PCL-5 (P < 0.001). Thus, combined, the studies contribute to the notion that female sex is a risk factor for emotional health issues after OHCA.
Notably, we found significant differences in age among women and men, with men being 8 years older on average. We explain this with the different causes of OHCA, i.e. a lower prevalence of ischaemic heart disease was found among women compared with men. In this study, none of the women had previous myocardial infarction. Thus, non-ischaemic causes of OHCA seem to be relatively more common in women. Also, CAG and percutaneous coronary intervention (PCI) were much more frequent in men. Besides these few baseline differences, no other differences were found between sexes; however, this may be due to the small number of females, thus a potential type 2 error. A smaller proportion of females attended follow-up compared with males. This may be due to females being younger and thus having more obligations such as full-time jobs; however, this remains speculative since our data cannot explain this issue.
Anxiety is an important component of post-OHCA rehabilitation because mental health can have a significant impact on an individual’s quality of life, including ability to perform daily activities, maintain relationships, and engage in work or leisure activities. Identifying at-risk groups may be important information that can be used to inform healthcare decision-making, evaluate treatment, and improve the overall quality of care for OHCA survivors.3 In our study, symptoms of depression were low in general and without sex-related differences.
The findings of females experiencing significantly more symptoms of anxiety compared with male responders may indicate that female survivors perceive a traumatic event such as OHCA as more stressful and anxiety-inducing than males. Epidemiological findings show that males and females perceive disease in fundamentally different ways. Females may be more prone to report worse psychological distress and show more signs of psychopathology after a traumatic and stressful event compared with males.24,25 Approximately twice as many females as males are diagnosed with PTSD.25 However, little is known about why females report more PTSD symptoms than males. Sex-related biological factors such as hormonal regulation and gender-related factors such as lifestyle may influence disease perception.26 Males and females on average may report symptoms of anxiety differently; thus, this parameter may be susceptible to reporting bias.26
In a study by Vincent et al.27 of 139 patients surviving OHCA, after 3 months, half of the survivors had signs of post-intensive care syndrome. A study of 15 survivors after refractory OHCA treated with mechanical circulatory support found a good neurological outcome with CPC 1–2 in 93% (14/15) of patients. No severe cognitive dysfunction was discovered with a mean MoCA score of 26 ± 3 with a high quality of life.28 This study had an insufficient sample to compare sex differences. However, it is surprising that the included patients with prolonged resuscitation and need for mechanical circulatory support presented with good cognitive function and low levels of anxiety. This illustrates that we have much to learn of what induces anxiety in patients. Intuitively, lower levels of health and worse cardiac arrest circumstances would give more symptoms of anxiety in survivors. In the present study, we found an association where younger patients reported more symptoms of anxiety. Also, patients with lower levels of self-reported health had more symptoms of anxiety. One of the strengths of this study is detailed data on baseline characteristics and severity of cardiac arrest. In the multivariable-adjusted analysis, we were able to adjust for several baseline variables including OHCA characteristics, which have been a limitation in previous studies and studies from registries. Furthermore, our sample size and consecutive inclusions add to this scientific area.
Knowledge of the scope of post-OHCA long-term cognitive and emotional symptoms may help guide clinical rehabilitation programmes and need for referral to specialized care. Evidence in this area is however limited. One clinical study has indicated that early intervention for cardiac arrest survivors may have a positive impact on quality of life.29 But more randomized studies are needed.
Limitations
This study included consecutive survivors of cardiac arrest from a tertiary ICU. Even though the ICU covers a large proportion of Denmark’s inhabitants, the findings may be limited by low external validity due to the single-centre design. Furthermore, as in all follow-up studies, including self-reported outcome measures from severely sick patients, we have some degree of missing data with the potential for reporting bias and selection bias. We had 24% of potentially eligible patients who were not included: 31 (8%) declined and 7 (2%) were too ill to participate. These 38 patients could introduce selection bias. We also had 55 patients who were not invited due to screen failures, mainly due to logistical issues during the COVID-19 pandemic. Selection bias from this group cannot be ruled out but is likely less severe since this type of missing data can be characterized as missing completely at random. Looking at differences among included and non-included patients, the groups were overall similar except in two parameters. Furthermore, this was a purely observational study, and observations and associations are not necessarily equal to causal relationships. We did find evidence that confounders, at least in part, explain differences among sexes. Our sample size is relatively large compared with other studies in this area; however, since females constitute a minority, this group is small and type 2 errors cannot be excluded. Future studies should evaluate whether early identification of these patients enables preventive strategies and treatment options.
Conclusions
In long-term survivors after resuscitated OHCA with coma, female sex is associated with significantly increased anxiety and post-traumatic stress. This difference is especially pronounced among younger males vs. younger females. The overall high numbers of stress and anxiety call for emphasis on appropriate screening and therapy in this patient population, and young females may require more intensive follow-up.
Supplementary material
Supplementary material is available at European Heart Journal: Acute Cardiovascular Care online.
Acknowledgements
We acknowledge the skilled assistance from Mie Christa Larsen and Áslaug Þóra Karlsdóttir.
Funding
J.K. was supported by an unrestricted grant from the Novo Nordisk Foundation: NNF17OC0028706 and NNF22OC0079649. J.G.’s salary is supported by a research grant from the Danish Cardiovascular Academy, funded by the Novo Nordisk Foundation, grant number NNF20SA0067242, and the Danish Heart Foundation.
Data availability
The data that support the findings of this study are available from the authors upon reasonable request and authorization from the relevant authorities to share data.
References
Author notes
Conflict of interest: None declared.
- anxiety
- cardiac arrest
- coma
- depressive disorders
- follow-up
- mental processes
- sex characteristics
- post-traumatic stress disorder
- survivors
- diagnostic and statistical manual
- mixed anxiety-depressive disorder
- cognitive ability
- ptsd checklist
- out-of-hospital cardiac arrest
- hospital anxiety and depression scale
- self-report
- montreal cognitive assessment




Comments