-
PDF
- Split View
-
Views
-
Cite
Cite
Dillen van der Aa, Mirte Ketel, Sofie Henckens, Mark van Berge Henegouwen, Camiel Rosman, Bastiaan Klarenbeek, Suzanne Gisbertz, 441. EXTENT AND BOUNDARIES OF LYMPH NODE STATIONS DURING MINIMALLY INVASIVE ESOPHAGECTOMY: A SURVEY AMONG DUTCH ESOPHAGEAL SURGEONS, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.191, https://doi.org/10.1093/dote/doae057.191
Close - Share Icon Share
Abstract
The optimal extent of lymph node dissection (LND), and the anatomical boundaries per lymph node station (LNS) during minimally invasive esophagectomy (MIE) for esophageal cancer remains a topic of debate. This study investigated the opinion of Dutch esophageal cancer surgeons on their routine LND extent and anatomical boundaries per LNS, during MIE.
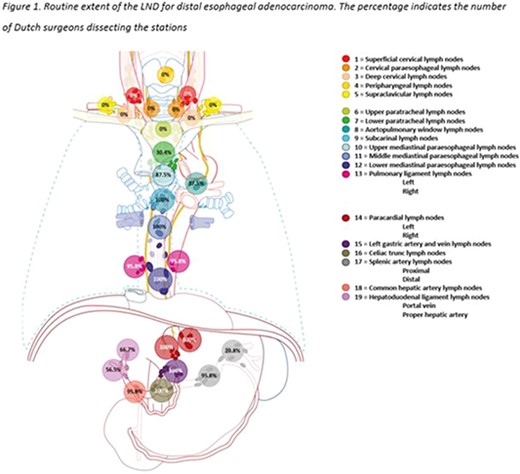
In April 2023, an English web-based cross-sectional survey was conducted. Within all 15 Dutch hospitals performing MIE, two MIE surgeons were asked to participate. The routine LND extent (quantity, specific LNS) for distal esophageal adenocarcinoma, (dis)agreement with the TIGER definition, and anatomical boundaries for each LNS in six directions were inquired.
Twenty-four Dutch MIE surgeons completed the survey (80% response rate). Consensus on the routine LND extent (85% or more of the participating surgeons) included the left and right paracardial, left gastric artery, celiac trunk, proximal splenic artery, common hepatic artery, subcarinal middle mediastinal paraoesophageal, lower mediastinal paraoesophageal, pulmonary ligament and upper mediastinal paraoesophageal LNSs. Other LNS were not widely considered routine. Although, certain anatomical boundaries were consistent among surgeons, the majority varied, even when agreeing on the TIGER definition.
Significant variations in surgical practice among Dutch esophageal surgeons, regarding their routine extent of LND and anatomical boundaries of LNSs during MIE were demonstrated. Variation may impact clinical outcomes, hampers uniform treatment strategies, and hinders comparison of performance assessments. This study highlights the need for an international follow-up study towards one uniform defined LND during MIE for esophageal cancer.