-
PDF
- Split View
-
Views
-
Cite
Cite
David J Nijssen, Johanna J Joosten, Jens Osterkamp, Richard M van den Elzen, Daniel Martijn de Bruin, Morten Bo Søndergaard Svendsen, Maria Winther Dalsgaard, Suzanne S Gisbertz, Roel Hompes, Michael P Achiam, Mark I van Berge Henegouwen, 440. QUANTIFICATION OF FLUORESCENCE ANGIOGRAPHY FOR ESOPHAGEAL PERFUSION ASSESSMENT: MEASURING AGREEMENT BETWEEN TWO SOFTWARE ALGORITHMS, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.190, https://doi.org/10.1093/dote/doae057.190
Close - Share Icon Share
Abstract
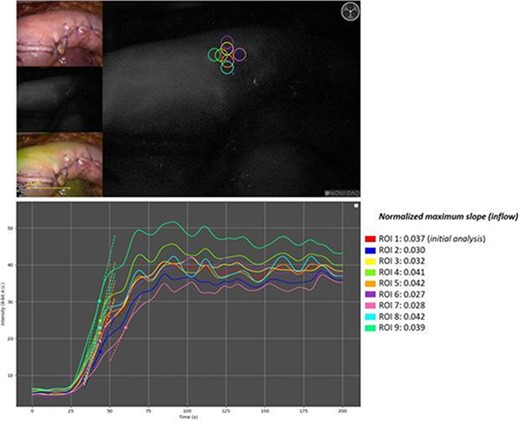
Indocyanine green fluorescence angiography (ICG-FA) may reduce perfusion related complications after esophagectomy with gastric conduit reconstruction. Software implementations for quantifying ICG-FA are emerging to overcome a subjective interpretation of the technology. Comparison between quantification algorithms is needed to judge its external validity. This study aimed to measure the agreement for esophageal perfusion assessment between two independently developed quantification software implementations.
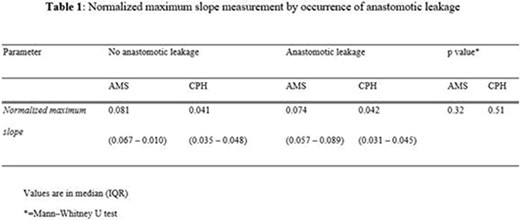
This retrospective cohort analysis included standardized ICG-FA video recordings of patients who underwent esophagectomy with gastric conduit reconstruction between August 2020 until February 2022. Recordings were analysed by two quantification software implementations: AMS and CPH. The quantitative parameter used to measure visceral perfusion was the normalized maximum slope derived from fluorescence time curves. The agreement between AMS and CPH was evaluated in a Bland-Altman analysis. The relation between the intraoperative measurement of perfusion and the incidence of anastomotic leakage was determined for both software implementations.
Seventy pre-anastomosis ICG-FA recordings were included in the study. The Bland-Altman analysis indicated a mean relative difference of +58.2% in the measurement of the normalized maximum slope when comparing the AMS software to CPH. The agreement between AMS and CPH deteriorated as the magnitude of the measured values increased, revealing a proportional (linear) bias (R2 = 0.512, p < .001). Neither the AMS nor the CPH measurements of the normalized maximum slope held a significant relationship with the occurrence of anastomotic leakage (median of 0.081 versus 0.074, p = 0.32 and 0.041 vs 0.042, p = 0.51, respectively). Divergent approaches in maximum slope determination and raw signal filtering were identified as contributing factors to the differences in outcome.
This is the first study to demonstrate technical differences in software implementations that can lead to discrepancies in ICG-FA quantification in human clinical cases. The possible variation among software-based quantification methods should be considered when interpreting studies that report quantitative ICG-FA parameters and derived thresholds, as there may be a limited external validity.