-
PDF
- Split View
-
Views
-
Cite
Cite
Hao Yin, Xu Huang, Heng Jiao, Han Tang, Lijie Tan, 399. LYMPH NODE METASTATIC PATTERNS AND SENTINEL LYMPH NODES FOR ESOPHAGEAL SQUAMOUS CELL CARCINOMA AFTER DIFFERENT NEOADJUVANT REGIMENS, Diseases of the Esophagus, Volume 37, Issue Supplement_1, September 2024, doae057.154, https://doi.org/10.1093/dote/doae057.154
Close - Share Icon Share
Abstract
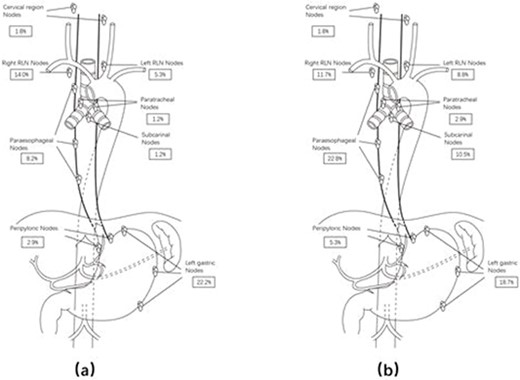
This study aimed to outline lymph node metastasis patterns in esophageal squamous cell carcinoma (ESCC) patients undergoing neoadjuvant chemoradiotherapy (nCRT) or chemotherapy (nCT), comparing regimens, assessing prognosis impact, and identifying potential sentinel lymph node stations for future individualized dissection.
Involving 578 ESCC patients undergoing nCRT (n=303) or nCT (n=275) followed by esophagectomy (2010-2022), we conducted propensity score matching, analyzing 171 pairs. Nodal metastasis patterns and station positivity associations with survival were assessed through univariate and multivariate models, adjusting for clinical factors.
Among 171 nCRT patients, 36.8% had nodal metastases, 22.8% single-station, 8.2% two-station, and 5.8% ≥3-station occurrences. Specific station positivity correlated with poorer survival. The nCRT group had fewer nodal metastases (36.8% vs 50.3%), common sites being left gastric, right recurrent laryngeal nerve, and paraesophageal region. Increased nodal stations and positive nodes correlated with worse prognosis. In nCRT, mentioned areas were prognostic; in nCT, only left gastric nodal metastases were prognostic. Single and multi-station rates were similar, but nCT had more multi-station disease. For sentinel lymph nodes, positivity in left gastric, paraesophageal, right recurrent laryngeal nerve for nCRT, and subcarinal, left recurrent laryngeal nerve, paratracheal, left gastric, paraesophageal right recurrent laryngeal nerve for nCT, may indicate complex metastasis.
Over one-third of ESCC patients had post nCRT metastatic lymph nodes. Though nCRT reduced metastasis rates, survival outcomes didn't improve, emphasizing thorough lymph node dissection based on metastasis patterns.