-
PDF
- Split View
-
Views
-
Cite
Cite
Takayuki Matsumoto, Keita Imai, Yuki Goda, Yuki Fujimitsu, Toshifumi Kajioka, Hideaki Kihara, Yuji Funaki, Shigeru Imaki, Masato Ueno, Questionnaire Survey for Inflammatory Bowel Disease Patients in Japan; A Web-Based Japan, Crohn’s Disease, Ulcerative Colitis, Patients Survey, Crohn's & Colitis 360, Volume 5, Issue 4, October 2023, otad069, https://doi.org/10.1093/crocol/otad069
Close - Share Icon Share
Abstract
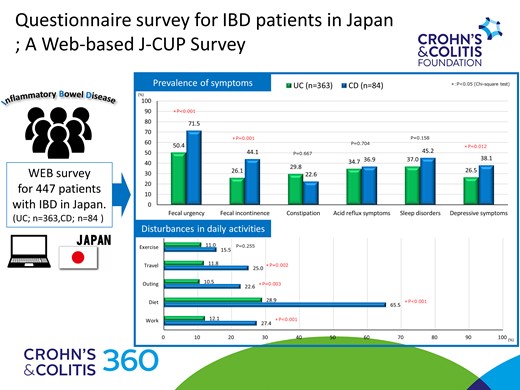
The prevalence of inflammatory bowel disease (IBD) in Japan has been increasing. We aimed to clarify the symptoms of patients with IBD in Japan using an internet-based questionnaire survey.
Overall, 805 patients with IBD were asked to complete an internet-based questionnaire addressing their history of disturbances in daily activities, prevalence of fecal urgency, incontinence, and treatment preferences.
Responses were obtained from 447 patients with IBD (mean age: 54 years; 70% were men), comprising 363 patients with ulcerative colitis (UC), and 84 with Crohn’s disease (CD). Notably, 16% of patients with UC and 35% with CD took over 1 year until the diagnosis of IBD, and 5% of patients with CD visited more than 5 medical institutions. Patients with CD were more likely to experience disturbances in their diet, work, travel, and outings than those with UC. Fecal urgency and incontinence were significantly more frequent in patients with CD than in those with UC (72% vs. 44%, and 50% vs. 26%, respectively). In contrast, 26% of the men and 37% of women with IBD had constipation. Acid reflux, sleep disorders, and depressive symptoms were present in approximately 30% of the patients. Oral administration was preferred.
Patients with IBD in Japan experience more severe disturbances in their daily activities, and these are more severe in those with CD than those with UC. In addition to fecal urgency and incontinence, care is required for constipation, acid reflux, sleep disorders, and depressive symptoms.
Lay Summary
An Internet-based survey of IBD patients was conducted in Japan which concluded that CD patients experienced more severe disturbances in their daily activity than UC patients. The survey also demonstrated actual diagnosis times and subjective symptoms and treatment preferences.
Introduction
Inflammatory bowel disease (IBD), classified into ulcerative colitis (UC), and Crohn’s disease (CD), is an intractable disease of unknown causes whose prevalence has been increasing in recent years.1–3 The main symptoms of IBD are diarrhea, abdominal pain, fever, weight loss, and bloody stools, and an early diagnosis is required because diagnostic delay can increase surgical risk.4–8
Patients with IBD experience an impaired quality of life (QOL). We previously reported on the QOL of IBD patients and disturbances in their daily activities in an internet survey of IBD patients.9 Recently, fecal urgency has been attracting attention as a factor impairing the QOL in IBD.10–13 Furthermore, various complications have been reported in patients with IBD, including sleep disorders and depressive symptoms.14–18 Thus, we conducted another internet-based survey referred to as the J-CUP survey (Japan, Crohn’s disease, Ulcerative colitis, Patients) to investigate the actual status of patients with IBD in Japan.
Methods
Survey Instruments
Between June 17 and 21, 2023, 805 patients with IBD (644 with UC and 161 with CD) registered with the Cross Marketing Corporation (Tokyo, Japan) were asked to participate in a questionnaire survey via email. Cross Marketing Corporation is a company that specializes in surveys and has registered patients with various diseases in Japan. In this case, patients with UC and CD were asked to cooperate in the survey.
The survey items included the type of disease (UC/CD), age, sex, duration of illness, area of residence, smoking status, occupation, history of bowel resection, history of hospitalization, type of attending institution (university hospital/general hospital/clinic/no hospital visits), frequency of visits, current degree of diarrhea and abdominal pain (none/mild/moderate/severe), current treatment methods, duration from the onset of symptoms until diagnosis, number of medical institutions visited, subjective symptoms (diarrhea, abdominal pain, bloody stools, fever, weight loss, etc.) observed before diagnosis, whether there were any disturbances in daily activities, exercise, travel, outing, diet, and work (very much/somewhat/none), specific symptoms (frequently/sometimes/none), and fecal urgency. Specifically, the following questions were prepared: (1) are you unable to hold your urge to go to the toilet or frequently need to go to the toilet (urgency), (2) do you experience stool leakage or observe stools in your underwear (incontinence), (3) do you experience constipation (constipation). (4) do you have any acid reflux symptoms (acid reflux symptoms), (5) do you have trouble sleeping (difficulty falling asleep, waking up in the middle of the night, taking sleeping pills, or sleep disorders), and (6) do you feel depressed (depressive symptoms). Regarding preferences for treatment methods, acceptability rating scores ranged from 1 to 10, with the most preferred treatment methods being oral therapy, in-hospital infusion, subcutaneous injection therapy, or self-injection therapy. The problems and concerns regarding the disease were surveyed through free text. Time to diagnosis, number of medical facilities visited, subjective symptoms observed before diagnosis, and presence of specific symptoms were compared separately for UC and CD. Consent to conduct the survey was obtained from the patients via the Internet.
Statistical Analysis
Statistical analysis was conducted using the Pearson chi-square test for categorical data and Student’s t-test for continuous variables; a P-value < .05 was considered statistically significant.
Results
Demographics of the Patients
Responses were received from 447, 363, and 84 patients with IBD, UC, and CD, respectively. No responses were considered ineligible, and all patients were included in the analysis. The mean age was 53.9 years, mean duration of disease was 16.5 years, and 70.0% of the patients were men (Table 1). Occupational status was full-time (47.9%), part-time (16.3%), student (0%), housework (8.7%), other (4.5%), or unemployed (22.6%). Diarrhea, abdominal pain, and other subjective symptoms were not present in 43.8% of the patients, mild in 40.3%, moderate in 15.7%, and severe in 1.3%.
| Number of patients . | 447 . |
|---|---|
| UC | 81.2% (363/447) |
| CD | 18.8% (84/447) |
| Sex (male) | 70.0% (313/447) |
| Age (mean ± SD) | 53.9 ± 11.2 years |
| Disease duration (mean ± SD) | 16.5 ± 10.9 years |
| Working status | |
| Full-time | 47.9% (214/447) |
| Part-time | 16.3% (73/447) |
| Student | 0% (0/447) |
| Housework | 8.7% (39/447) |
| Other | 4.5% (20/447) |
| Unemployed | 22.6% (101/447) |
| Smoking | |
| Present | 17.0% (76/447) |
| Past | 33.1% (148/447) |
| Never | 49.9% (223/447) |
| History of resection | 17.2% (77/447) |
| Number of hospitalizations (mean ± SD) | 2.7 ± 8.7 |
| Degree of current symptoms | |
| None | 43.8% (191/447) |
| Mild | 40.3% (180/447) |
| Moderate | 15.7% (70/447) |
| Severe | 1.3% (6/447) |
| Visiting institutions | |
| University hospital | 18.3% (82/447) |
| General hospital | 51.2% (231/447) |
| Clinic | 30.0% (134/447) |
| No regular visits | 0% (0/447) |
| Frequency of visits | |
| Once a week | 0% (0/447) |
| Once every 2 weeks | 1.6% (7/447) |
| Once a month | 26.12 (117/447) |
| Once every 2 months | 42.3% (189/447) |
| Once every 3 months | 28.2% (126/447) |
| Less often than that | 1.8% (8/447) |
| Treatment methods | |
| Oral therapy | 92.4% (413/447) |
| Nutritional therapy | 10.7% (48/447) |
| Infusion or injection therapy | 15.9% (71/447) |
| Self-injection therapy | 6.0% (27/447) |
| Topical therapy | 15.9% (71/447) |
| Other | 1.6% (7/447) |
| None | 2.2% (10/447) |
| Number of patients . | 447 . |
|---|---|
| UC | 81.2% (363/447) |
| CD | 18.8% (84/447) |
| Sex (male) | 70.0% (313/447) |
| Age (mean ± SD) | 53.9 ± 11.2 years |
| Disease duration (mean ± SD) | 16.5 ± 10.9 years |
| Working status | |
| Full-time | 47.9% (214/447) |
| Part-time | 16.3% (73/447) |
| Student | 0% (0/447) |
| Housework | 8.7% (39/447) |
| Other | 4.5% (20/447) |
| Unemployed | 22.6% (101/447) |
| Smoking | |
| Present | 17.0% (76/447) |
| Past | 33.1% (148/447) |
| Never | 49.9% (223/447) |
| History of resection | 17.2% (77/447) |
| Number of hospitalizations (mean ± SD) | 2.7 ± 8.7 |
| Degree of current symptoms | |
| None | 43.8% (191/447) |
| Mild | 40.3% (180/447) |
| Moderate | 15.7% (70/447) |
| Severe | 1.3% (6/447) |
| Visiting institutions | |
| University hospital | 18.3% (82/447) |
| General hospital | 51.2% (231/447) |
| Clinic | 30.0% (134/447) |
| No regular visits | 0% (0/447) |
| Frequency of visits | |
| Once a week | 0% (0/447) |
| Once every 2 weeks | 1.6% (7/447) |
| Once a month | 26.12 (117/447) |
| Once every 2 months | 42.3% (189/447) |
| Once every 3 months | 28.2% (126/447) |
| Less often than that | 1.8% (8/447) |
| Treatment methods | |
| Oral therapy | 92.4% (413/447) |
| Nutritional therapy | 10.7% (48/447) |
| Infusion or injection therapy | 15.9% (71/447) |
| Self-injection therapy | 6.0% (27/447) |
| Topical therapy | 15.9% (71/447) |
| Other | 1.6% (7/447) |
| None | 2.2% (10/447) |
Abbreviation: UC: ulcerative colitis, CD: Crohn’s disease.
| Number of patients . | 447 . |
|---|---|
| UC | 81.2% (363/447) |
| CD | 18.8% (84/447) |
| Sex (male) | 70.0% (313/447) |
| Age (mean ± SD) | 53.9 ± 11.2 years |
| Disease duration (mean ± SD) | 16.5 ± 10.9 years |
| Working status | |
| Full-time | 47.9% (214/447) |
| Part-time | 16.3% (73/447) |
| Student | 0% (0/447) |
| Housework | 8.7% (39/447) |
| Other | 4.5% (20/447) |
| Unemployed | 22.6% (101/447) |
| Smoking | |
| Present | 17.0% (76/447) |
| Past | 33.1% (148/447) |
| Never | 49.9% (223/447) |
| History of resection | 17.2% (77/447) |
| Number of hospitalizations (mean ± SD) | 2.7 ± 8.7 |
| Degree of current symptoms | |
| None | 43.8% (191/447) |
| Mild | 40.3% (180/447) |
| Moderate | 15.7% (70/447) |
| Severe | 1.3% (6/447) |
| Visiting institutions | |
| University hospital | 18.3% (82/447) |
| General hospital | 51.2% (231/447) |
| Clinic | 30.0% (134/447) |
| No regular visits | 0% (0/447) |
| Frequency of visits | |
| Once a week | 0% (0/447) |
| Once every 2 weeks | 1.6% (7/447) |
| Once a month | 26.12 (117/447) |
| Once every 2 months | 42.3% (189/447) |
| Once every 3 months | 28.2% (126/447) |
| Less often than that | 1.8% (8/447) |
| Treatment methods | |
| Oral therapy | 92.4% (413/447) |
| Nutritional therapy | 10.7% (48/447) |
| Infusion or injection therapy | 15.9% (71/447) |
| Self-injection therapy | 6.0% (27/447) |
| Topical therapy | 15.9% (71/447) |
| Other | 1.6% (7/447) |
| None | 2.2% (10/447) |
| Number of patients . | 447 . |
|---|---|
| UC | 81.2% (363/447) |
| CD | 18.8% (84/447) |
| Sex (male) | 70.0% (313/447) |
| Age (mean ± SD) | 53.9 ± 11.2 years |
| Disease duration (mean ± SD) | 16.5 ± 10.9 years |
| Working status | |
| Full-time | 47.9% (214/447) |
| Part-time | 16.3% (73/447) |
| Student | 0% (0/447) |
| Housework | 8.7% (39/447) |
| Other | 4.5% (20/447) |
| Unemployed | 22.6% (101/447) |
| Smoking | |
| Present | 17.0% (76/447) |
| Past | 33.1% (148/447) |
| Never | 49.9% (223/447) |
| History of resection | 17.2% (77/447) |
| Number of hospitalizations (mean ± SD) | 2.7 ± 8.7 |
| Degree of current symptoms | |
| None | 43.8% (191/447) |
| Mild | 40.3% (180/447) |
| Moderate | 15.7% (70/447) |
| Severe | 1.3% (6/447) |
| Visiting institutions | |
| University hospital | 18.3% (82/447) |
| General hospital | 51.2% (231/447) |
| Clinic | 30.0% (134/447) |
| No regular visits | 0% (0/447) |
| Frequency of visits | |
| Once a week | 0% (0/447) |
| Once every 2 weeks | 1.6% (7/447) |
| Once a month | 26.12 (117/447) |
| Once every 2 months | 42.3% (189/447) |
| Once every 3 months | 28.2% (126/447) |
| Less often than that | 1.8% (8/447) |
| Treatment methods | |
| Oral therapy | 92.4% (413/447) |
| Nutritional therapy | 10.7% (48/447) |
| Infusion or injection therapy | 15.9% (71/447) |
| Self-injection therapy | 6.0% (27/447) |
| Topical therapy | 15.9% (71/447) |
| Other | 1.6% (7/447) |
| None | 2.2% (10/447) |
Abbreviation: UC: ulcerative colitis, CD: Crohn’s disease.
Time to Diagnosis
The time from symptom onset to diagnosis was less than 1 month in 24.5% of patients with UC and 15.5% of patients with CD and more than 1 year in 15.4% of patients with UC and 34.5% of patients with CD (Figure 1). Diagnoses were made in 58.1% of patients with UC and 27.4% of patients with CD at the first medical institution; however, 9.7% of the patients with UC and 17.8% with CD visited 3 or more institutions. Bloody stools were significantly more common in the UC group than in the CD group. Additionally, abdominal pain, fever, weight loss, and other symptoms were significantly more common in the CD group (P < .05) (Figure 2).
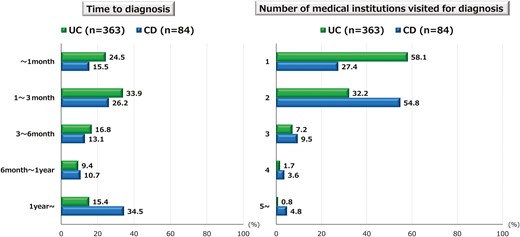
Time to diagnosis and number of medical institutions visited. The figures show the time taken from the onset of inflammatory bowel disease (IBD) symptoms to the diagnosis of ulcerative colitis (UC) and Crohn’s disease (CD), and the number of medical institutions consulted.
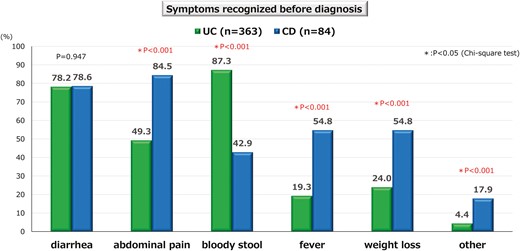
Symptoms recognized before diagnosis. Diarrhea is not significantly different between ulcerative colitis (UC) and Crohn’s disease (CD); however, bloody stools are significantly more common in UC, whereas abdominal pain, fever, weight loss, and other symptoms are significantly more common in CD.
Disturbances in Daily Activities
Disturbances in daily activities of either very much or somewhat, were significantly more frequent in patients with CD than in those with UC (P < .05) for travel, outings, diet, and work (Figure 3). The percentage of patients with CD and dietary disturbances was particularly high (65.5%).
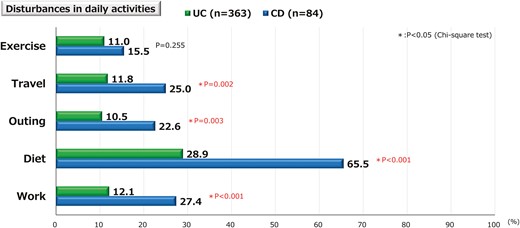
Disturbances in daily activities. With regard to disturbances in daily activities, exercise is not significantly different between the ulcerative colitis (UC) and Crohn’s disease (CD) groups; however, travel, outings, diet, and work are significantly higher in the CD group.
Fecal Urgency and Incontinence
The frequencies of fecal urgency and incontinence frequently or sometimes were significantly higher (P < .05) in patients with CD (71.5% and 44.1 %, respectively) than in those with UC (50.4% and 26.1%, respectively) (Figure 4). In 84 CD patients, a comparison was made between groups with and without a history of bowel resection, but no significant difference was found in either fecal urgency or incontinence.
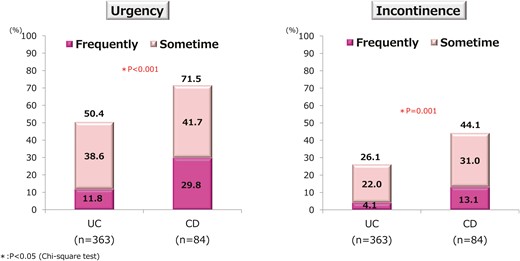
Prevalence of fecal urgency and incontinence. The prevalence of fecal urgency and incontinence are significantly higher in patients with Crohn’s disease (CD) than in those with ulcerative colitis (UC).
Other Complications
Constipation, acid reflux symptoms, sleep disorders, and depressive symptoms were also frequently observed, with depressive symptoms being significantly more common in CD (P < .05). However, there were no differences in the other symptoms according to the disease (Table 2). Notably, constipation was significantly more common in women (P < .05).
Prevalence of constipation, acid reflux symptoms, sleep disorders, and depressive symptoms.
| Complications . | . | Frequently . | Sometimes . | Frequently + sometimes . | P-value . |
|---|---|---|---|---|---|
| Constipation | UC | 7.2% (26/363) | 22.6% (82/363) | 29.8% (108/363) | P = .667 |
| CD | 3.6% (3/84) | 23.8% (20/84) | 27.4% (23/84) | ||
| Men | 4.5% (14/313) | 21.7% (68/313) | 26.2% (82/313) | *P = .027 | |
| Women | 11.2% (15/134) | 25.4% (34/134) | 36.6% (49/134) | ||
| Acid reflux symptoms | UC | 5.5% (20/363) | 29.2% (106/363) | 34.7% (126/363) | P = .704 |
| CD | 7.1% (6/84) | 29.8% (25/84) | 36.9% (31/84) | ||
| Men | 4.8% (15/313) | 28.1% (88/313) | 32.9% (103/313) | P = .134 | |
| Women | 8.2% (11/134) | 32.1% (43/134) | 40.3% (54/134) | ||
| Sleep disorders | UC | 16.3% (59/363) | 20.7% (75/363) | 37.0% (134/363) | P = .158 |
| CD | 22.6% (19/84) | 22.6% (19/84) | 45.2% (38/84) | ||
| Men | 16.3% (51/313) | 20.8% (65/313) | 37.1% (116/313) | P = .346 | |
| Women | 20.1% (27/134) | 21.6% (29/134) | 41.7% (56/134) | ||
| Depressive symptoms | UC | 8.5% (31/363) | 16.0% (58/363) | 26.5% (89/363) | *P = 0012 |
| CD | 14.3% (12/84) | 23.8% (20/84) | 38.1% (32/84) | ||
| Men | 8.6% (27/313) | 16.3% (51/313) | 24.9% (78/313) | P = .118 | |
| Women | 11.9% (16/134) | 20.1% (27/134) | 32.0% (43/134) |
| Complications . | . | Frequently . | Sometimes . | Frequently + sometimes . | P-value . |
|---|---|---|---|---|---|
| Constipation | UC | 7.2% (26/363) | 22.6% (82/363) | 29.8% (108/363) | P = .667 |
| CD | 3.6% (3/84) | 23.8% (20/84) | 27.4% (23/84) | ||
| Men | 4.5% (14/313) | 21.7% (68/313) | 26.2% (82/313) | *P = .027 | |
| Women | 11.2% (15/134) | 25.4% (34/134) | 36.6% (49/134) | ||
| Acid reflux symptoms | UC | 5.5% (20/363) | 29.2% (106/363) | 34.7% (126/363) | P = .704 |
| CD | 7.1% (6/84) | 29.8% (25/84) | 36.9% (31/84) | ||
| Men | 4.8% (15/313) | 28.1% (88/313) | 32.9% (103/313) | P = .134 | |
| Women | 8.2% (11/134) | 32.1% (43/134) | 40.3% (54/134) | ||
| Sleep disorders | UC | 16.3% (59/363) | 20.7% (75/363) | 37.0% (134/363) | P = .158 |
| CD | 22.6% (19/84) | 22.6% (19/84) | 45.2% (38/84) | ||
| Men | 16.3% (51/313) | 20.8% (65/313) | 37.1% (116/313) | P = .346 | |
| Women | 20.1% (27/134) | 21.6% (29/134) | 41.7% (56/134) | ||
| Depressive symptoms | UC | 8.5% (31/363) | 16.0% (58/363) | 26.5% (89/363) | *P = 0012 |
| CD | 14.3% (12/84) | 23.8% (20/84) | 38.1% (32/84) | ||
| Men | 8.6% (27/313) | 16.3% (51/313) | 24.9% (78/313) | P = .118 | |
| Women | 11.9% (16/134) | 20.1% (27/134) | 32.0% (43/134) |
Abbreviation: UC, ulcerative colitis; CD, Crohn’s disease;
*P < .05 (chi-square test).
Prevalence of constipation, acid reflux symptoms, sleep disorders, and depressive symptoms.
| Complications . | . | Frequently . | Sometimes . | Frequently + sometimes . | P-value . |
|---|---|---|---|---|---|
| Constipation | UC | 7.2% (26/363) | 22.6% (82/363) | 29.8% (108/363) | P = .667 |
| CD | 3.6% (3/84) | 23.8% (20/84) | 27.4% (23/84) | ||
| Men | 4.5% (14/313) | 21.7% (68/313) | 26.2% (82/313) | *P = .027 | |
| Women | 11.2% (15/134) | 25.4% (34/134) | 36.6% (49/134) | ||
| Acid reflux symptoms | UC | 5.5% (20/363) | 29.2% (106/363) | 34.7% (126/363) | P = .704 |
| CD | 7.1% (6/84) | 29.8% (25/84) | 36.9% (31/84) | ||
| Men | 4.8% (15/313) | 28.1% (88/313) | 32.9% (103/313) | P = .134 | |
| Women | 8.2% (11/134) | 32.1% (43/134) | 40.3% (54/134) | ||
| Sleep disorders | UC | 16.3% (59/363) | 20.7% (75/363) | 37.0% (134/363) | P = .158 |
| CD | 22.6% (19/84) | 22.6% (19/84) | 45.2% (38/84) | ||
| Men | 16.3% (51/313) | 20.8% (65/313) | 37.1% (116/313) | P = .346 | |
| Women | 20.1% (27/134) | 21.6% (29/134) | 41.7% (56/134) | ||
| Depressive symptoms | UC | 8.5% (31/363) | 16.0% (58/363) | 26.5% (89/363) | *P = 0012 |
| CD | 14.3% (12/84) | 23.8% (20/84) | 38.1% (32/84) | ||
| Men | 8.6% (27/313) | 16.3% (51/313) | 24.9% (78/313) | P = .118 | |
| Women | 11.9% (16/134) | 20.1% (27/134) | 32.0% (43/134) |
| Complications . | . | Frequently . | Sometimes . | Frequently + sometimes . | P-value . |
|---|---|---|---|---|---|
| Constipation | UC | 7.2% (26/363) | 22.6% (82/363) | 29.8% (108/363) | P = .667 |
| CD | 3.6% (3/84) | 23.8% (20/84) | 27.4% (23/84) | ||
| Men | 4.5% (14/313) | 21.7% (68/313) | 26.2% (82/313) | *P = .027 | |
| Women | 11.2% (15/134) | 25.4% (34/134) | 36.6% (49/134) | ||
| Acid reflux symptoms | UC | 5.5% (20/363) | 29.2% (106/363) | 34.7% (126/363) | P = .704 |
| CD | 7.1% (6/84) | 29.8% (25/84) | 36.9% (31/84) | ||
| Men | 4.8% (15/313) | 28.1% (88/313) | 32.9% (103/313) | P = .134 | |
| Women | 8.2% (11/134) | 32.1% (43/134) | 40.3% (54/134) | ||
| Sleep disorders | UC | 16.3% (59/363) | 20.7% (75/363) | 37.0% (134/363) | P = .158 |
| CD | 22.6% (19/84) | 22.6% (19/84) | 45.2% (38/84) | ||
| Men | 16.3% (51/313) | 20.8% (65/313) | 37.1% (116/313) | P = .346 | |
| Women | 20.1% (27/134) | 21.6% (29/134) | 41.7% (56/134) | ||
| Depressive symptoms | UC | 8.5% (31/363) | 16.0% (58/363) | 26.5% (89/363) | *P = 0012 |
| CD | 14.3% (12/84) | 23.8% (20/84) | 38.1% (32/84) | ||
| Men | 8.6% (27/313) | 16.3% (51/313) | 24.9% (78/313) | P = .118 | |
| Women | 11.9% (16/134) | 20.1% (27/134) | 32.0% (43/134) |
Abbreviation: UC, ulcerative colitis; CD, Crohn’s disease;
*P < .05 (chi-square test).
Acceptability of Treatment Methods and Most Preferred Methods
The mean acceptability scores for oral therapy, in-hospital infusion or injection therapy, and self-injection therapy were 7.7, 4.3, and 3.2, respectively, with significant differences among all groups (P < .05) (Figure 5). The preferred treatment methods were oral therapy (90.6%), in-hospital infusions or injections (6.7%), and self-injections (2.7%).
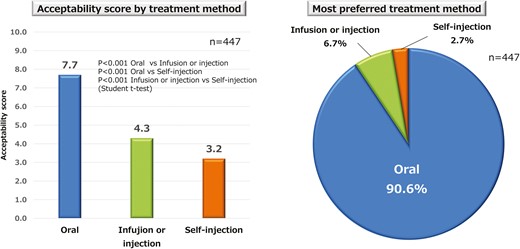
Acceptability and preferences regarding treatment methods. The mean acceptability scores for oral therapy, in-hospital infusion or injection therapy, and self-injection therapy differ significantly between groups. Oral therapy is the preferred treatment.
Troubles and Concerns With the Disease
The most frequently mentioned problem in the free-text responses was the unavailability of a toilet when going out, traveling, or working because of the urgency of bowel movements. The most frequently mentioned concerns were recurrence or worsening of the disease, risk of colorectal cancer, bowel resection, finances associated with treatment costs and work, future life, and disease course.
Discussion
In this internet-oriented survey, we investigated the present status of the diagnosis and management of IBD from the standpoint of patients and found that there is still a delay in the initial diagnosis of IBD, especially that of CD, in Japan. As found in our survey, diagnostic delay has been reported to be common in patients with CD.4–7 Although the current study did not assess the factors leading to a delayed diagnosis or its impact on disease prognosis, a meta-analysis indicated that a diagnostic delay is associated with disease progression and increased risk of surgery.4 While targeted treatment is considered important to improve the prognosis and QOL of patients, the first step is to diagnose the disease as early as possible.14,15 Our survey suggested that the diagnostic ability of medical institutions and the understanding of the disease in some patients are matters of debate in the management of IBD.
We also found that the rate of disturbance was significantly higher in the CD group than in the UC group for travel, outings, diet, and work. This observation is in accordance with our previous report.9 Since nutritional disturbances are still considered particularly important in CD in Japan,16–18 dietary disturbances may be particularly important in CD. Although the disease activity of IBD causes disturbances in daily activities, we believe that along with treatment improvements, guidance on appropriate daily living must also be provided.19
Fecal urgency has recently gained attention as an important symptom that impairs the QOL in IBD.10–13 Although validated scoring was not used in the current study, fecal urgency and incontinence were both frequent, at 50% and 26% for UC and 72% and 44% for CD, respectively, and were significantly more common in CD than in UC. Some studies have examined fecal urgency only in UC, and we believe that the higher frequency of fecal urgency in CD, as observed in this study, is valuable. Fecal urgency and QOL can be improved by appropriate treatment,20–22 and it is important to raise awareness about fecal urgency care and treat it aggressively.
Other complications, such as constipation, acid reflux symptoms, sleep disorders, and depressive symptoms were also investigated. Constipation is a common disease and has been shown to impair the QOL.23–25 IBD is a disease with diarrhea as its main symptom, and constipation has been reported to occur with some frequency in remission.26 In our study, most patients had no or mild symptoms of IBD, and constipation was frequently observed. Since our study did not compare the prevalence with that of the general population, it is not known whether the prevalence is higher in patients with IBD. However, as in the general population, the prevalence is higher among women, suggesting that care is needed not only for diarrhea but also for constipation during remission.
Psychogenic care, such as sleep disorders and depressive symptoms, is also important in the management of IBD.27,28 Sleep disorders are reported to have a high complication rate in IBD, and complications of sleep disorders are also reported to lead to the recurrence of IBD.29–31 Similarly, depressive symptoms have been reported to be more prevalent in patients with IBD and are associated with the recurrence and disease activity of IBD.32–35 The prevalence of depressive symptoms was significantly higher in patients with CD than in those with UC, which may be related to the greater disturbance of daily activities and severity of CD.
The usefulness of biologics for refractory IBD has been widely demonstrated.36–40 However, biologics are inevitably administered via intravenous or subcutaneous injections. Recently, oral small molecules have become available for the treatment of IBD.41–44 Shared decision-making has made it possible for patients to choose treatments based not only on the efficacy and safety of the drug, but also on patient preferences, such as convenience.45 Thus, we evaluated the patient acceptability of the 3 administration methods. The results showed that the patients’ acceptability scores for oral therapy were significantly higher than those for hospital intravenous infusion, subcutaneous injection, and self-injection, with 91% of the patients choosing oral therapy as their preferred administration method. While similar results have been shown by European studies, the acceptability of oral therapy in our survey was the highest among those previous reports.46,47 Although our study did not consider the frequency of drug administration, we confirmed that oral therapy is a highly acceptable treatment option for patients with IBD in Japan.
This study had several limitations. The first is the possibility of a biased population owing to internet-based patient surveys. Although the proportion of male patients was high in this survey, it was similar to the general sex ratio and age structure of patients with IBD in Japan and Asian countries,48–51 and in the previous 2 surveys.9,52 In addition, the regions of residence of the respondents were less biased; thus, the bias seems to have been relatively small. Second, because this was an internet-based survey, there was a problem with the accuracy of the responses. However, Kelstrup et al. reported on the consistency of patient ratings and medical records in internet-based surveys.53 The third limitation was that we did not compare patients with the general population in this study. Therefore, it is unclear whether patients with IBD are at a higher risk of developing constipation, acid reflux symptoms, sleep disorders, and depressive symptoms.
In conclusion, our web-based survey of Japanese patients with IBD showed that some patients require time to be diagnosed with IBD. Additionally, several patients experience disturbances in their daily activities, including fecal urgency and incontinence, constipation, acid reflux symptoms, sleep disturbances, and depressive symptoms.
Acknowledgments
This survey was planned and supported by EA Pharma Co., Ltd. (Tokyo, Japan) and conducted by Cross Marketing Co., Ltd. (Tokyo, Japan).
Author Contributions
T.M. drafted the manuscript and reviewed the relevant literature. M.U. designed the survey and drafted the manuscript. K.I., Y.G., Y.F., T.K., H.K., and S.I. designed the study. Y.F. participated in data analysis. All the authors have read and approved the final version of this manuscript.
Funding
This work was supported by EA Pharma Co. Ltd.
Conflicts of Interest
T.M.: Lecture fee and consultant fee; EA Pharma Co., Ltd. K.I., Y.G., Y.F., T.K., H.K., Y.F., S.I., and M.U.: EA Pharma Co. Ltd.
Data Availability
Data not publicly available. The data used and analyzed for this study are available from the corresponding author upon reasonable request.



