-
PDF
- Split View
-
Views
-
Cite
Cite
Raul Fernandez-Prado, Alberto Ortiz, A sudden decrease in serum creatinine and estimated glomerular filtration rate: clinical implications of administrative gender assignment in transgender persons, Clinical Kidney Journal, Volume 13, Issue 6, December 2020, Pages 1107–1108, https://doi.org/10.1093/ckj/sfz152
Close - Share Icon Share
The choice of gender to estimate glomerular filtration rate (eGFR) in transgender persons may have a profound impact on clinical decision making and care [1]. However, few physicians are aware of this fact. In gender- and creatinine-based eGFR equations, gender is a surrogate for muscle mass [2]. Thus, even though there are no official guidelines to deal with the issue, it seems reasonable to choose the gender in the equation based on the individual’s actual muscle mass rather than on the current administrative or self-identity gender, or better still, to measure GFR in clinical situations where a precise value is required [3]. In this regard, transgender female creatinine values resemble male ones [4]. We report a 40-year-old female referred to nephrology for a sudden ‘decrease’ in eGFR that could be traced to the gender change in administrative records. Over recent years her serum creatinine had ranged from 0.90 to 1.03 mg/dL and eGFR from 100 to 112 mL/min/1.73 m2. However, in April 2019, serum creatinine was 0.93 mg/dL but, surprisingly, eGFR had dropped to 77 mL/min/1.73 m2 according to Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (Figure 1). Discussion of the issue with the patient disclosed that she was a transgender female and had been on hormone therapy (cyproterone and estradiol) for 10 years, although this was not reflected in the electronic clinical records. A recent change in gender in the hospital administrative records resulted in a change in the automated equation to calculate eGFR from male to female. Indeed, the CKD-EPI ‘male’ eGFR remained stable at 103 mL/min/1.73 m2 and 24-h creatinine clearance was 122 mL/min. The topic of GFR estimation in transgender persons is not addressed in recent guidelines [5], and the lack of understanding by primary care physicians or specialists of the issues involved may potentially lead to unnecessary and even potentially invasive diagnostic procedures. A closer integration of the administrative, clinical biochemistry and clinical levels of care may decrease the possibility of harm by creating physician alerts triggered by recent changes in gender in administrative records, which provide information on potential biochemical implications.
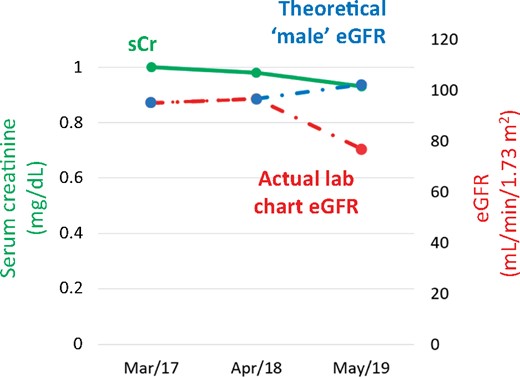
Serum creatinine and eGFR over recent years. eGFR is automatically estimated from serum creatinine and administrative databases containing gender and date of birth information. In April 2019, a marked decrease in eGFR (red data point representing clinical biochemistry records) was not associated with an increase in serum creatinine. The decrease in eGFR was traced to a change in the administrative gender from male to female, which resulted in an automatic switch from the male to the female CKD-EPI equation. The blue data points represent eGFR values estimated from the male CKD-EPI equation.
CONFLICT OF INTEREST STATEMENT
None declared.





Comments