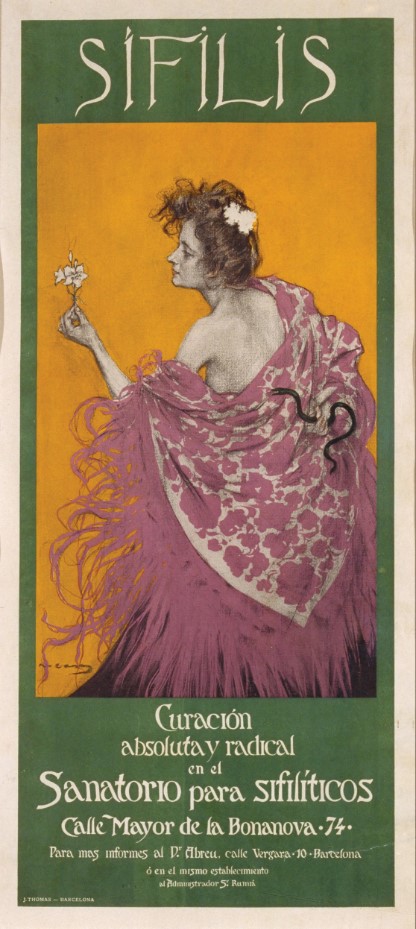
Cover image
Volume 78, Issue 1, 15 January 2024
In the Literature
IN THE LITERATURE
State-of-the-Art Review
Executive Summary: State-of-the-Art Review: Persistent Enterococcal Bacteremia
Voices of ID
Personal Stories From a World Turned Upside Down: Introducing the Voices of ID Collection
Timing
Embracing Diversity, Equity, and Inclusion: Am I Part of the Picture?
Mothers’ Days
Invited Commentary
Emerging Roles of (1→3)-β-D-Glucan in Cerebrospinal Fluid for Detection and Therapeutic Monitoring of Invasive Fungal Diseases of the Central Nervous System
Antimicrobial Resistance
Individualized Antibiotic Plans as a Quality Improvement Initiative to Reduce Carbapenem Use for Hematopoietic Cell Transplant Patients at a Freestanding Pediatric Hospital
Individualized antibiotic plans are a well-received tool that support antimicrobial stewardship principles in medically complex patients. We used this novel resource to decrease carbapenem use in pediatric patients receiving hematopoietic cell transplant without overall increase in bloodstream infection or mortality.
Impact of the COVID-19 Pandemic on Inpatient Antibiotic Use in the United States, January 2019 Through July 2022
Identifying Effective Durations of Antibiotic Therapy for the Treatment of Carbapenem-resistant Enterobacterales Bloodstream Infections: A Multicenter Observational Study
Bacterial Infections
Clinical and Genomic Characterization of a Cohort of Patients With Klebsiella pneumoniae Bloodstream Infection
In a cohort of patients with Klebsiella pneumonia bacteremia, most infections were caused by strains that lacked canonical features associated with invasion. Patients given an ineffective first antibiotic were more likely to die, highlighting the need to rapidly identify resistance.
Rifampin Based Therapy for Patients With Staphylococcus aureus Native Vertebral Osteomyelitis: A Systematic Review and Meta-analysis
This meta-analysis showed that adjunctive rifampin therapy may be associated with lower risk of Staphylococcus aureus native vertebral osteomyelitis treatment failure. A randomized trial is necessary to corroborate these findings, given the very low certainty of evidence.
Clinical Trials
Immunogenicity of High-Dose Versus MF59-Adjuvanted Versus Standard Influenza Vaccine in Solid Organ Transplant Recipients: The Swiss/Spanish Trial in Solid Organ Transplantation on Prevention of Influenza (STOP-FLU Trial)
In this randomized-controlled trial, solid-organ transplant recipients receiving the MF59-adjuvanted and the high-dose influenza vaccines had higher antibody responses than patients receiving the standard influenza vaccine. All 3 vaccines were well tolerated. Rates of breakthrough influenza were similar between groups.
COVID-19/SARS-CoV-2
Cost-Effectiveness of Universal Asymptomatic Preoperative SARS-CoV-2 Polymerase Chain Reaction Screening: A Cost-Utility Analysis
In the base case analysis, asymptomatic preoperative universal SARS-CoV-2 PCR screening is not cost-effective. The cost-effectiveness depends mainly on the test-positive rate, the frequency of postoperative pulmonary complications, and screening costs.
Impact of SARS-CoV-2 Arrival Surveillance Screening by Nucleic Acid Amplification Versus Rapid Antigen Detection on Subsequent COVID-19 Infections in Military Trainees
The efficacy of arrival severe acute respiratory syndrome coronavirus 2 surveillance screening to prevent case clusters of coronavirus disease 2019 among training groups was not different when comparing nucleic acid amplification with rapid antigen detection test.
Long-term Cardiovascular, Cerebrovascular, and Other Thrombotic Complications in COVID-19 Survivors: A Retrospective Cohort Study
In the 300 days following infection, SARS-CoV-2–infected individuals exhibited increased risk of new-incident cardiovascular and cerebrovascular complications compared with test-negative controls. Risks decreased with vaccination and boosting. Conversely, risks increased for hospitalized and severe COVID-19 cases, compared to nonhospitalized cases.
Emerging Infections
Powassan Virus Encephalitis: A Tertiary Center Experience
This large retrospective case series (2013–2022) included 16 patients with neuroinvasive Powassan virus who presented with rhombencephalitis, isolated meningitis, meningoencephalitis, meningoencephalomyelitis, and/or opsoclonus myoclonus syndrome. The 90-day mortality rate was 18.8%, with neurologic deficits seen in 72.7% of survivors.
Global Health and Neglected Tropical Diseases
Relationships Between Schistosoma mansoni Infection Intensity and Nutritional Status and Anemia Among Preschool-aged Children in Uganda
Extracorporeal Membrane Oxygenation–Dependent Fulminant Melioidosis From Caspase 4 Mutation Reversed by Interferon Gamma Therapy
HIV/AIDs
Antiretroviral Drug Exposure and Response in Obese and Morbidly Obese People With Human Immunodeficiency Virus (HIV): A Study Combining Modelling and Swiss HIV Cohort Data
Antiretroviral dose adjustment is not required a priori in obese people with HIV (PWH). Despite a 20% reduction in antiretroviral exposure and trough concentrations below target thresholds for etravirine and rilpivirine, virological response was similar between obese and nonobese PWH.
Drastic Reduction in Time to Controlled Viral Load in People With Human Immunodeficiency Virus in France, 2009–2019: A Longitudinal Cohort Study
Among 16 864 people diagnosed with HIV between 1 January 2009 and 31 December 2019, we describe considerable improvement in time from diagnosis to controlled viral load, from 254 [127–745] to 73 days [48–132] during the study period.
Misclassification of Loss to Care Among Persons With Human Immunodeficiency Virus: Improved Capture of Silent Transfers Through Surveillance Linkage Using Statewide Mandatorily Reported Laboratory Measures
Long-acting Injectable Cabotegravir/Rilpivirine Effective in a Small Patient Cohort With Virologic Failure on Oral Antiretroviral Therapy
Mycobacterial Infections
Pregnancy Outcomes in Women Screened for Tuberculosis Infection in Swedish Antenatal Care
Among immigrant women seeking Swedish antenatal care, tuberculosis infection was independently associated with stillbirth, severe preeclampsia, low birthweight, and emergency cesarean section, suggesting that tuberculosis infection may be involved in the pathogenesis of pregnancy-related disorders.
The Impact of Preventive Treatment for Multidrug- and Rifampin-Resistant Tuberculosis Exceeds Trial-Based Estimates
This modeling analysis translates forthcoming clinical trial estimates of the efficacy of drug-resistant tuberculosis preventive therapy into longer-term and population-wide effects. The full impact and cost-effectiveness of this intervention are likely to be several times greater than trials directly measure.
Pediatric and Maternal Infectious Diseases
Pregnancy and Birth Outcomes in Patients With Multidrug-Resistant Tuberculosis Treated With Regimens That Include New and Repurposed Drugs
Pre-extensively Drug-Resistant Congenital Tuberculosis in an Extremely Premature Baby
Respiratory Infections
Cost-effectiveness of Low-complexity Screening Tests in Community-based Case-finding for Tuberculosis
Active case-finding might reduce the tuberculosis (TB) diagnostic gap. We estimate that screening tests could meaningfully improve these active case-finding efforts, but only if they are highly sensitive, specific (approximately 70%–95%), and available at low costs (approaching $4.5/test all-inclusive).
Estimating Post-treatment Recurrence After Multidrug-Resistant Tuberculosis Treatment Among Patients With and Without Human Immunodeficiency Virus: The Impact of Assumptions About Death and Missing Follow-up
Quantifying recurrence risk following successful treatment for multidrug-resistant tuberculosis, crucial to regimen evaluation, is complicated when patients die or become lost during post-treatment follow-up. We examine multiple approaches for addressing these issues and provide guidance for researchers conducting similar analyses.
Invasive Pneumococcal Disease and Potential Impact of Pneumococcal Conjugate Vaccines Among Adults, Including Persons Experiencing Homelessness—Alaska, 2011–2020
Invasive pneumococcal disease incidence increased among Alaska adults during 2011–2020, driven by increases among Alaska Native adults and adults experiencing homelessness. A substantial proportion of cases were potentially preventable by new pneumococcal conjugate vaccines.
Surgical Infectious Diseases
Infective Endocarditis After Transcatheter Versus Surgical Aortic Valve Replacement
This study compared infective endocarditis (IE) after surgical aortic valve replacement and transcatheter aortic valve replacement; 1688 patients with IE affecting the aortic valve prosthesis were included. Clinical presentation, complications, and treatment were different, but 1-year mortality rates were similar.
How We Approach Suppressive Antibiotic Therapy Following Debridement, Antibiotics, and Implant Retention for Prosthetic Joint Infection
Limited data suggest suppressive antibiotic therapy (SAT) may reduce treatment failure following debridement and implant retention (DAIR) for prosthetic joint infection. We propose a structured approach to selecting patients for SAT following DAIR incorporating known DAIR treatment failure risk factors.
Photo Quiz
A 22-Year-Old With a Left Apical Chest Mass
Vaccines
Respiratory Syncytial Virus Prefusion F Protein Vaccine Is Efficacious in Older Adults With Underlying Medical Conditions
Evaluation of Intussusception Following Pentavalent Rotavirus Vaccine (RotaTeq) Administration in 5 African Countries
The risk of intussusception following rotavirus vaccination may vary by vaccine type and socioeconomic status. In a pooled analysis of data from 5 countries in Africa, RotaTeq vaccination was not associated with an increased risk of intussusception.
The Durability of Antibody Responses of Two Doses of High-Dose Relative to Two Doses of Standard-Dose Inactivated Influenza Vaccine in Pediatric Hematopoietic Cell Transplant Recipients: A Multi-Center Randomized Controlled Trial
In pediatric hematopoietic cell transplant (HCT) recipients, 2 doses of high-dose trivalent influenza vaccine were more immunogenic than 2 doses of standard-dose quadrivalent influenza vaccine, especially when administered ≥6 months post-HCT. Influenza-specific titers remained higher than baseline for all antigens.
Correspondence
Linking the Who, What, When, and Where of Inpatient Direct Oral Penicillin Challenge With the How of Durable Penicillin Allergy Delabeling
Reply to Olans and Olans
Reduced Risk of Transfusion-Transmitted Babesiosis With Blood Donor Testing
Correction
Correction to: Gut Resistome After Oral Antibiotics in Preschool Children in Burkina Faso: A Randomized, Controlled Trial
State-of-the-Art Review
State-of-the-Art Review: Persistent Enterococcal Bacteremia
Persistent enterococcal bacteremia is a commonly encountered and morbid syndrome without a strong evidence base for optimal management practices. Here we highlight reports on the epidemiology of enterococcal bacteremia to better describe and define persistent enterococcal bacteremia, discuss factors specific to Enterococcus species that may contribute to persistent infections, and describe a measured approach to diagnostic and therapeutic strategies for patients with these frequently complicated infections. The diagnosis of persistent enterococcal bacteremia is typically clinically evident in the setting of repeatedly positive blood culture results; instead, the challenge is to determine in an accurate, cost-effective, and minimally invasive manner whether any underlying nidus of infection (eg, endocarditis or undrained abscess) is present and contributing to the persistent bacteremia. Clinical outcomes for patients with persistent enterococcal bacteremia remain suboptimal. Beyond addressing host immune status if relevant and pursuing source control for all patients, management decisions primarily involve the selection of the proper antimicrobial agent(s). Options for antimicrobial therapy are often limited in the setting of intrinsic and acquired antimicrobial resistance among enterococcal clinical isolates. The synergistic benefit of combination antimicrobial therapy has been demonstrated for enterococcal endocarditis, but it is not clear at present whether a similar approach will provide any clinical benefit to some or all patients with persistent enterococcal bacteremia.












