-
PDF
- Split View
-
Views
-
Cite
Cite
Pasquale F Finelli, New Onset Focal Tremor in Patient With Human Immunodeficiency Virus, Clinical Infectious Diseases, Volume 75, Issue 10, 15 November 2022, Pages 1861–1863, https://doi.org/10.1093/cid/ciab960
Close - Share Icon Share
CASE
A 34-year-old woman with congenital human immunodeficiency virus (HIV)/AIDS presented with a 10-day history of intermittent right arm and leg shaking movements. The movements happen multiple times during the day, last seconds to a minute, occurred at rest but mostly with intention and did not impair awareness. She had been on antiretroviral therapy (ART) until 2 years ago and resumed treatment 1 month prior to left extremity shaking. Six months prior to the current admission her CD4 count = 92 cells/cumm, human immunodeficiency virus type 1 (HIV-1) RNA = 270 525 copies/mL, and HIV-1 RNAlog10(VL) log10copies/mL = 5.43.
Patient was afebrile with stable vital signs. Neurologic findings showed intention tremor, slowed finger tapping, dysmetria, and rebound in the right upper extremity. Gait was mildly unsteady on regular and tandem walking with remainder normal.
Complete blood count showed mild anemia and leukopenia with normal routine blood chemistries and blood culture. CD4 count = 57cells/cumm, HIV-1 RNA = 586 875copies/mL (N = <40) and VL = 5.7 log copies/ml (N = <1.60). Routine cerebrospinal fluid (CSF) analysis was normal. Blood and CSF serologies and polymerase chain rection (PCR) for, Epstein-Barr virus (EBV), cytomegalovirus (CMV), cryptococcus, toxoplasmosis, mycoplasma, and varicella zoster virus were all negative including rapid plasma regain (RPR). JC virus PCR was “detected” in serum but negative in CSF. CSF culture and meningitis/encephalitis panel was negative. Electroencephalogram, transthoracic echocardiogram, chest X-ray and computed tomography (CT) scan and thallium SPECT scan of head were normal. Magnetic resonance (MR) imaging showed a nonenhancing 1 cm round lesion the Left midbrain in the area of the red nucleus with scattered multiple smaller lesions on FLAIR sequence (Figure 1).

What is your diagnosis?
Diagnosis: Progressive multifocal leukoencephalopathy
In the setting of human immunodeficiency virus (HIV) infection with low CD4 count and reinstitution of antiretroviral therapy (ART) and multiple brain lesions on magnetic resonance (MR) imaging opportunistic infection and lymphoma were leading diagnostic considerations. The negative serum and cerebrospinal fluid (CSF) serologies and polymerase chain reaction (PCR) along with nonenhancing lesions on MR imaging reduced the likelihood of toxoplasmosis, cytomegalovirus (CMV), and cryptococcal infection. Brain lymphoma was virtually excluded given the negative serology and PCR for Epstein-Barr virus (EBV) along with negative thallium SPECT scan and absence of enhancement on MR. Movement disorders in HIV patients are varied, uncommon and diverse in origin including direct HIV infection [1, 2]. Toxoplasmosis of the basal ganglia is the most common etiology of tremor (2) and the underlying pathogenesis relates to disruption of the dopaminergic system primarily involving the basal ganglia and/or connections to thalamus, brainstem, and cerebellum. Holmes tremor (also known as rubral or midbrain) manifesting a resting, postural or intentional component contralateral to the lesion, correlates with the MR midbrain lesion and best explains the movement disorder in our patient [3]. Although a variety of central nervous system (CNS) pathologies may cause Holmes tremor it most commonly is vascular in origin and rarely due to opportunistic infection in patients with HIV [4]. Holmes tremor due to midbrain toxoplasma abscess and progressive multifocal leukoencephalopathy (PML) lesions in patients with HIV, however, is described [5–9].
Despite the frequent occurrence of toxoplasmosis in HIV the absence of lesion enhancement along with a negative serology and PCR for toxoplasmosis in association with recent ART favored PML as the likely underlying disease process in our patient. Importantly, atypical MR imaging features and negative CSF JC virus PCR present in our patient are now commonly seen in the context of ART/IRIS [10]. Our patient was treated empirically for toxoplasmosis with sulfinpyrazone and pyrimethamine, as well as ART until follow-up MR imaging after 5 weeks showed lesion progression and subsequent brain biopsy confirmed the diagnosis of PML (Figure 2A, 2B). Holmes tremor with PML after reinstitution of ART is rare and heralded the neurologic presentation in our patient. Despite high dose prednisone and ART the patient showed progressive decline in cognition and gait and was admitted to the inpatient hospice service and expired 1 month after brain biopsy.
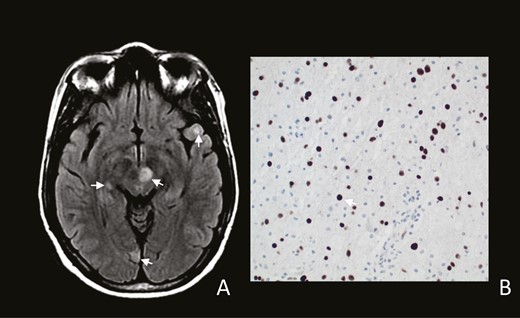
A, MR-FLAIR sequences with multiple areas of increased signal involving medial midbrain (arrow), left thalamus and right putamen with scattered smaller lesions (arrows). B, Brain biopsy showing oligodendrocyte nuclei staining positive for J-C virus (arrow) (Sv40 immunostain 200×).
References
Author notes
Potential conflicts of interest. The author: No reported conflicts of interest. The author has submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.




