-
PDF
- Split View
-
Views
-
Cite
Cite
Sujata Sajjan, Reeti Khare, Filamentous Organisms in a Blood Culture, Clinical Infectious Diseases, Volume 67, Issue 6, 15 September 2018, Pages 978–979, https://doi.org/10.1093/cid/ciy093
Close - Share Icon Share
A 79-year-old male presented to our institution with a fever of 100.9oF, shaking, chills, altered mental status, and 2 episodes of seizures. His prior medical history is significant for dementia, myasthenia gravis, type 2 diabetes mellitus, hypertension, right frontal hemorrhagic stroke, benign prostatic hyperplasia, and 2 simple kidney cysts. He was diagnosed 6 weeks earlier with an Escherichia coli bacteremia with no known source and with acute cystitis and hematuria caused by Klebsiella pneumoniae. Both organisms were pansensitive, and he was treated for 4 days with piperacillin–tazobactam and for 10 days with cefdinir. Follow-up blood cultures after 2 days showed no growth. His current urinalysis results showed negative nitrite, positive leukocyte esterase, and the presence of both red and white blood cells (WBC >50 and RBC >50/high-powered field). Blood and urine cultures were sent to the laboratory. The patient was started on empiric vancomycin and piperacillin–tazobactam but expired less than 24 hours later. The anaerobic blood culture bottle flagged positive after 98 hours of incubation, with the Gram stain showing long, gram-variable filaments containing bulbous inclusions (Figure 1).
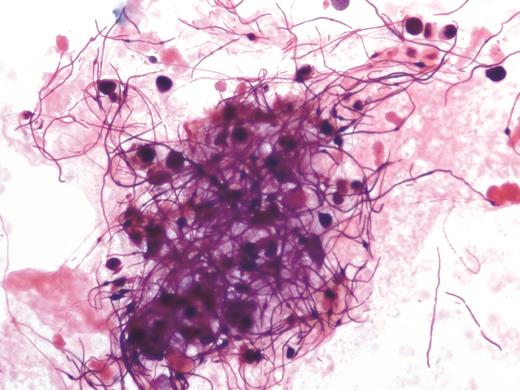
Filamentous, gram-variable organisms in a blood culture bottle that turned positive at 98 hours (magnification × 500).
What is your diagnosis?
Diagnosis: Gram-negative rods showing antibiotic treatment effect, identified as Klebsiella pneumoniae (Figure 1).
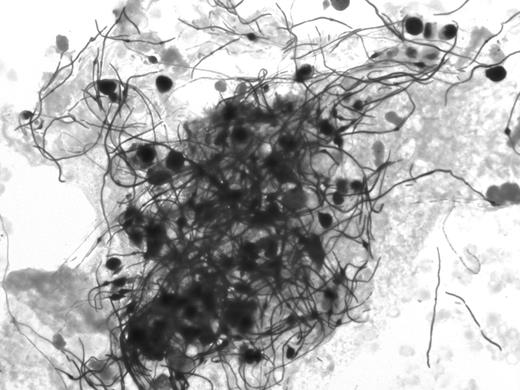
Filamentous, gram-variable organisms in a blood culture bottle that turned positive at 98 hours (original magnification, ×500).
A comprehensive polymerase chain reaction for 24 bacterial targets and 3 antibiotic resistance genes (BioFire FilmArray) was performed and detected only K. pneumoniae. The identification was confirmed from growth on culture plates using biochemical analysis (Microscan) and mass spectrometry (Vitek). The isolate was pansensitive. No other organisms grew on blood, chocolate, Sabouraud dextrose, and MacConkey agar plates. The presence of rare gram-negative bacilli seen with the Gram stain and the narrow filament diameter (1 µm) supported a bacterial, rather than fungal, cause. The Gram stain from the colony showed gram-negative rods typical of Enterobacteriaceae in subculture. Investigative Kinyoun stains from the original positive bottle were negative for acid fast bacilli.
Subinhibitory concentrations of antibiotics can cause gross morphologic changes in bacteria recovered from in clinical specimens [1]. Studies in Escherichia coli have shown that β-lactam antibiotics interacting with penicillin-binding proteins (PBPs) can cause structural changes, depending on the type of PBP involved. For instance, binding of β-lactams to PBP-1 causes bacterial cell lysis, binding to PBP-2 causes cell rounding, and binding to PBP-3 causes filamentation [2]. On the other hand, filamentation may be a response to promote bacterial survival. Some reports suggest that the large size of bacterial filaments can inhibit phagocytosis, and filamentous bacteria are better able to maintain the capacity for cell division, compared with the bacillary form [3]. “Inclusions” were also apparent in many filaments. These bulbous swellings probably represent fragile points in the filament, because lysis has been observed at these sites as the antibiotic concentration increases [1]. Antibiotic effects on bacteria should be considered when interpreting atypical Gram stains.
Note
Potential conflicts of interest. All authors: No reported conflicts of interest. The authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.




