-
Views
-
Cite
Cite
Thiziri Tala-Ighil, Dea Garcia-Hermoso, Frédéric Dalle, Sophie Cassaing, Juliette Guitard, Karine Boukris-Sitbon, Thomas Obadia, Olivier Lortholary, Valérie Letscher-Bru, Marie-Pierre Ledoux, Taïeb Chouaki, Anne Pauline Bellanger, Célia Rouges, Marie Elisabeth Bougnoux, Maxime Moniot, Marc Pihet, Vincent Dubée, Frédéric Gabriel, Florent Morio, Lilia Hasseine, Christine Bonnal, Maud Gits-Muselli, Estelle Perraud-Cateau, Caroline Mahinc, Muriel Nicolas, Elisabeth Chachaty, Camille Cordier, Laurence Lachaud, Laura Courtellemont, Benoït Henry, Cécile Angebault, Gilles Gargala, Adélaïde Chesnay, Marie Liesse Pacreau, Laure Kamus, Nicole Desbois-Nogard, Magalie Demar, Loïc Epelboin, Alexandre Alanio, Eric Dannaoui, Fanny Lanternier, for the French Mycoses Study Group , Epidemiology and Prognostic Factors Associated With Mold-Positive Blood Cultures: 10-Year Data From a French Prospective Surveillance Program (2012–2022), Clinical Infectious Diseases, Volume 80, Issue 3, 15 March 2025, Pages 529–539, https://doi.org/10.1093/cid/ciae594
Close - Share Icon Share
Abstract
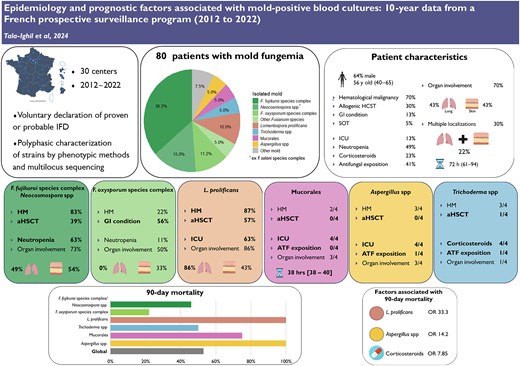
While invasive fusariosis and lomentosporiosis are known to be associated with fungemia, overall data on mold-related fungemia are limited, hampering early management. This study aimed to describe the epidemiology of mold-positive blood cultures.
Epidemiological and clinical data on mold-positive blood cultures from 2012 to 2022 were obtained from the RESSIF database. Pseudofungemia was excluded using modified Duthie and Denning criteria. Univariable and multivariable Firth logistical regression was used to study factors associated with 90-day mortality.
Fusarium spp accounted for 67.5% of the 80 events, involving predominantly Fusarium fujikuroi spp complex (FFSC), Neocosmospora spp, and Fusarium oxysporum spp complex (FOSC). Lomentospora prolificans was the second most frequent (10%), followed by Trichoderma spp, Aspergillus spp, and Mucorales (5% each).
Most patients had a history of hematological malignancy (HM) (70%). Forty-three percent had undergone allogeneic hematopoietic stem cell transplantation. Cutaneous and pulmonary lesions were common (43% each). Median time to blood culture positivity was 72 hours.
HM and neutropenia were commonly reported in patients with FFSC, Neocosmospora spp, and L. prolificans fungemia. Pulmonary lesions were frequent in cases of L. prolificans fungemia. Patients with gastrointestinal conditions were frequently diagnosed with FOSC molds. HM (75%), particularly acute myeloblastic leukemia, was frequent in patients with Aspergillus spp fungemia. All patients with Trichoderma spp fungemia were exposed to corticosteroids.
Day 90 mortality was 53%. Independent predictive factors of day 90 mortality included L. prolificans (odds ratio [OR], 33.3), Aspergillus spp fungemia (OR, 14.2), and corticosteroid exposure (OR, 7.85).
Underlying conditions and clinical presentation vary between genera and could be considered to guide early management.